Secondary Hypogonadism – What It Is and How to Manage It
If your doctor mentioned low testosterone but said the problem isn’t in the testes, they’re talking about secondary hypogonadism. In this form of low testosterone the testicles are fine; the brain’s hormone centers aren’t sending the right signals. That mix‑up can make you feel tired, lose muscle, or notice a drop in libido, just like primary low T.
Why Hormone Levels Drop
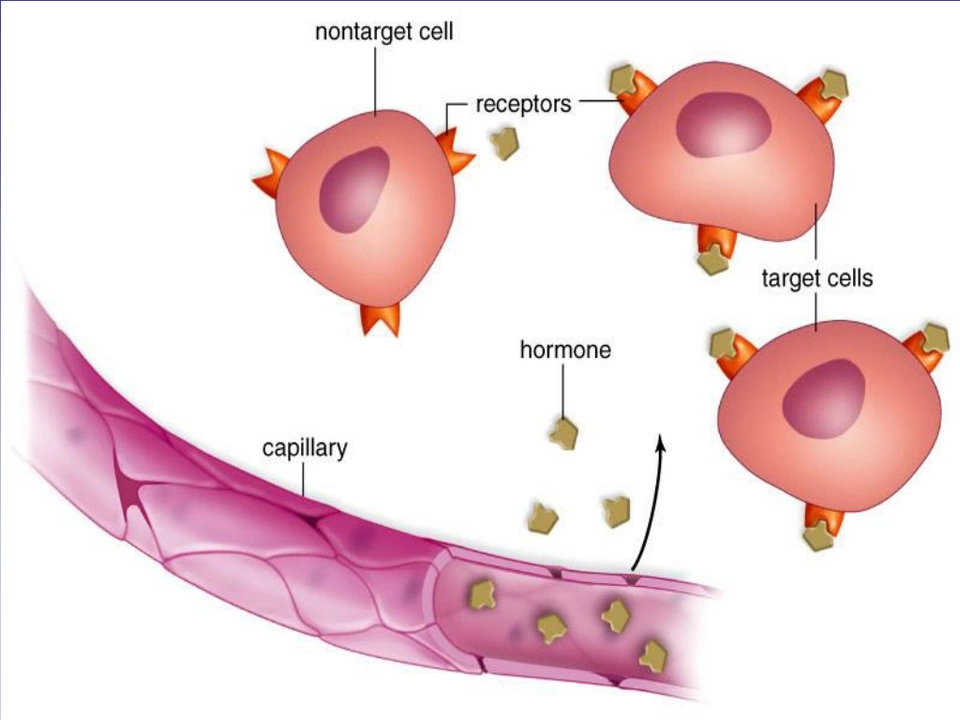
The hypothalamus and pituitary gland act like the body’s thermostat for sex hormones. They release GnRH, LH, and FSH to tell the testes to make testosterone. Anything that messes with this chain can cause secondary hypogonadism. Common culprits include pituitary tumors, head injuries, chronic stress, severe illness, or medications such as steroids and opioids.
Even simple things like uncontrolled diabetes or obesity can interfere with hormone signaling. When the brain thinks there’s enough testosterone, it cuts back on LH and FSH, leaving the testes idle. That’s why fixing the underlying issue often restores normal levels without needing direct testosterone shots.
Spotting the Signs and Getting Help
The symptoms look a lot like primary low T: low energy, reduced sex drive, mood swings, loss of muscle mass, and a bit more body fat. Because the signs are vague, many men chalk them up to aging or stress. If you notice several of these changes together, it’s worth getting blood work done.
A doctor will check total testosterone, free testosterone, LH, FSH, and sometimes prolactin. Low testosterone with low or normal LH/FSH points to secondary hypogonadism. Imaging tests like an MRI may be ordered if a pituitary problem is suspected.
Treatment starts by fixing the root cause. If a medication is the trigger, your doctor might switch you to something else. For pituitary tumors, surgery or radiation can help. When the underlying issue can’t be fully resolved, hormone replacement becomes an option.
Testosterone therapy for secondary hypogonadism works well because the testes are still capable of producing testosterone once they get the right signal. Options include gels, patches, injections, or pellets. Your doctor will pick a method that fits your lifestyle and monitor levels regularly to avoid side effects.
While on therapy, simple lifestyle moves boost results: aim for 30 minutes of moderate exercise most days, keep weight in check, get enough sleep, and limit alcohol. These steps help the brain’s hormone loop stay balanced.
If you’re dealing with secondary hypogonadism, don’t ignore it. A quick blood test can confirm what’s going on, and there are clear paths to feel better—whether that means adjusting meds, treating a pituitary issue, or adding testosterone in a safe way.
Secondary Hypogonadism and the Immune System: What You Need to Know
As a blogger, I recently came across an interesting topic, secondary hypogonadism and its connection to the immune system. Secondary hypogonadism is a condition where the testes or ovaries do not produce enough hormones, affecting the reproductive system. It turns out, there is a significant link between this condition and our immune system. Research suggests that low hormone levels can impact the immune system's function, making us more susceptible to infections and other health issues. It's important for us to understand this connection and be aware of the potential consequences on our overall health.