Understanding Streptococcal Infections: Signs, Care and How to Stay Safe
If you’ve ever had a sore throat that felt worse than a regular cold, chances are you’ve met Group A Strep. That’s the bacteria behind most streptococcal infections – from strep throat to scarlet fever and even rheumatic fever if it’s left untreated. The good news? Knowing what to look for and how to act can keep you out of the doctor’s office or hospital.
Common Types of Strep Infections
The most familiar one is strep throat. It shows up as a sudden, painful sore throat, white patches on the tonsils and fever above 101°F. Kids get it more often, but adults aren’t immune.
Scarlet fever follows the same bacteria but adds a rash that feels like sandpaper and a bright red tongue – the classic “strawberry tongue.” It’s rare today thanks to antibiotics, yet still shows up during outbreaks in schools.
If a strep infection spreads to the heart or joints, it can cause rheumatic fever. Symptoms include joint pain, chest discomfort and a distinctive jerky movement called Sydenham chorea. This serious complication usually appears weeks after the original sore throat if the infection wasn’t treated.
When to See a Doctor & Treatment Options
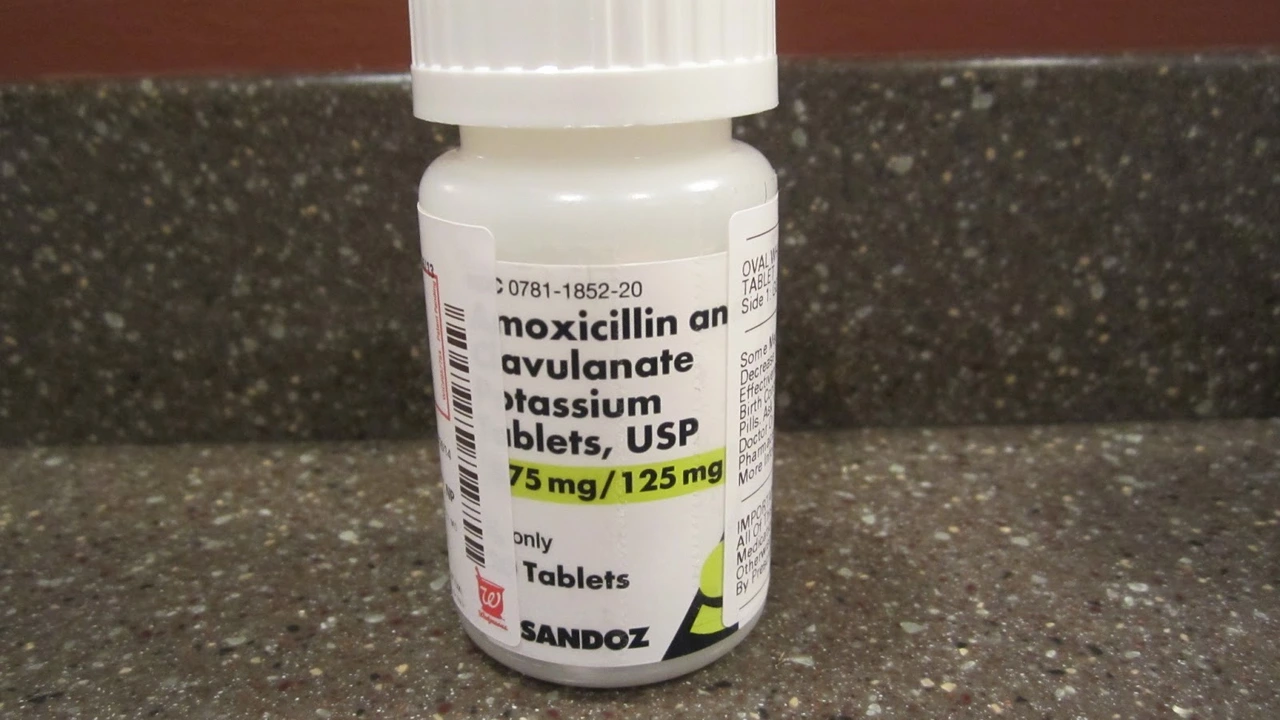
If you have any of these signs – severe sore throat, fever, swollen lymph nodes or a rash – call your healthcare provider. A quick throat swab can confirm Group A Strep. Doctors typically prescribe penicillin or amoxicillin for 10 days; this kills the bacteria and stops complications.
Got an allergy to penicillin? No problem. Alternatives like azithromycin or clarithromycin work just as well. Finish the full course, even if you feel better after a couple of days – stopping early can let the bugs survive and become resistant.
Over‑the‑counter pain relievers such as ibuprofen or acetaminophen help with fever and throat pain while the antibiotics do their job. Rest, plenty of fluids and soft foods make swallowing easier too.
Preventing streptococcal infections is mostly about hygiene. Wash your hands often, especially after coughing or sneezing. Avoid sharing drinks, utensils or toothbrushes. If you’re sick, stay home for at least 24 hours after starting antibiotics to keep the germs from spreading.
Vaccines against Strep pneumoniae exist, but they don’t protect against Group A strep. Research is ongoing, so the best defense right now is early detection and proper treatment.
Bottom line: streptococcal infections are common, treatable and usually easy to spot if you know the signs. Keep an eye on sore throats that get worse fast, watch for rash or joint pain, and don’t skip your antibiotics. A few simple habits at home can keep the bugs away and protect everyone around you.
The Use of Clindamycin in the Treatment of Streptococcal Infections
In my latest research, I've delved into the use of Clindamycin in treating Streptococcal infections. This antibiotic is highly effective against these infections due to its ability to inhibit bacterial protein synthesis. It's especially useful when patients are allergic to penicillin or when penicillin is ineffective. However, there are potential side effects, including diarrhoea and allergic reactions. Like all antibiotics, it's crucial to use Clindamycin responsibly to prevent antibiotic resistance.