Every pill you swallow, every injection you get, every inhaler you use - it’s not magic. It’s chemistry. And if you don’t understand how that chemistry works, you’re flying blind when it comes to your own safety.
Medicines don’t just appear in your body and fix things. They’re designed to interact with specific targets inside you - proteins, enzymes, receptors - like a key fitting into a lock. That’s called the mechanism of action. It’s the reason aspirin stops your headache, why statins lower your cholesterol, and why some drugs can cause serious harm if used wrong.
How Medicines Actually Work
When you take a pill, it doesn’t magically know where to go. It travels through your bloodstream, often stuck to proteins like a hitchhiker on a bus. Only the free, unbound portion can actually do anything. For most drugs, 95% or more of what you swallow is tied up and inactive until it’s released.
Some medicines work right where they land. If you take a laxative for constipation, it’s acting on your gut. But if you take a painkiller like ibuprofen, it gets absorbed into your blood and travels to inflamed tissues, blocking enzymes called COX-1 and COX-2. That stops the production of prostaglandins - the chemicals that make you feel pain and swell up.
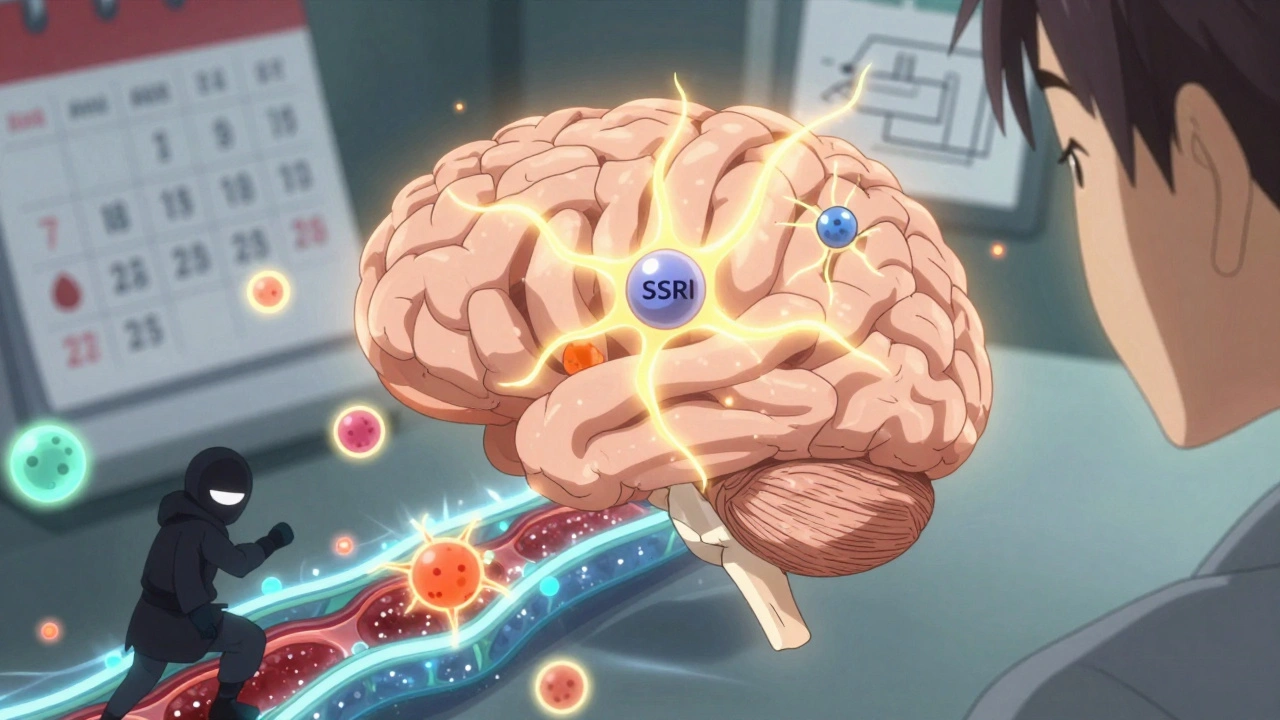
Other drugs are more precise. Take SSRIs like fluoxetine (Prozac). They don’t just boost your mood randomly. They block the serotonin transporter - the molecular vacuum cleaner that pulls serotonin back into nerve cells after it’s released. By clogging that vacuum, more serotonin stays in the space between nerves, helping signals that regulate mood get through. It’s not a quick fix. It takes weeks because your brain needs time to adapt to the change.
Some medicines need help getting where they’re supposed to go. The brain is protected by the blood-brain barrier - a tight filter that keeps most substances out. That’s why Parkinson’s patients take levodopa, not dopamine. Dopamine can’t cross the barrier. Levodopa can. Once inside, the body converts it into dopamine. This isn’t luck. It was engineered.
Why Understanding Mechanism Matters for Safety
Knowing how a drug works isn’t just for doctors. It’s your best defense against dangerous side effects.
Take warfarin, a blood thinner. It works by blocking vitamin K, which your body needs to make clotting factors. But vitamin K is also in spinach, kale, broccoli - all the healthy greens you’re told to eat. If you suddenly eat a big salad every day, your blood thins too much. If you stop eating greens, you risk clots. Patients who understand this link are 3 times more likely to keep their INR levels stable and avoid emergency bleeding.
Or consider statins. They block HMG-CoA reductase, the enzyme your liver uses to make cholesterol. That’s why they work. But that same enzyme is also involved in muscle cell function. So muscle pain isn’t just a coincidence - it’s a direct signal that the drug is affecting something it shouldn’t. Patients who know this report muscle aches early. That’s how you catch rhabdomyolysis - a rare but life-threatening muscle breakdown - before it’s too late.
Then there’s lithium, used for bipolar disorder. It’s one of the oldest psychiatric drugs, but we still don’t fully understand how it works. It affects multiple systems in the brain. That’s why its safety window is so narrow. Too little, and it doesn’t help. Too much, and it causes tremors, confusion, even kidney damage. Blood levels must be kept between 0.6 and 1.2 mmol/L. That’s why you get regular blood tests. If you don’t know why, you might skip them - and risk poisoning yourself.

When Medications Are Safe to Use
Safety isn’t just about taking the right dose. It’s about timing, context, and awareness.
Some drugs are safe only under strict conditions. Natalizumab (Tysabri), used for multiple sclerosis, blocks immune cells from entering the brain. That’s good - it reduces flare-ups. But it also stops your body from fighting a rare brain virus called PML. That’s why doctors require you to get tested for the virus before starting and monitor you closely during treatment. This isn’t guesswork. It’s built into the drug’s mechanism.
Antibiotics like penicillin kill bacteria by breaking down their cell walls. That’s why they don’t hurt your human cells. But if you take them when you don’t need them - say, for a cold - you’re not helping yourself. You’re just giving bacteria a chance to evolve resistance. That’s why antibiotics are only safe when prescribed for confirmed bacterial infections.
MAO inhibitors, used for depression, are another example. They block enzymes that break down neurotransmitters like serotonin and dopamine. But they also let tyramine - found in aged cheese, cured meats, and fermented foods - build up in your blood. Too much tyramine can spike your blood pressure to dangerous levels. One ounce of blue cheese can have up to 5 mg of tyramine. A single bite, with the wrong drug, can send you to the ER.
Even over-the-counter drugs aren’t risk-free. Acetaminophen (Tylenol) is safe at 3,250 mg per day. But if you drink alcohol regularly, your liver processes it differently. That tiny extra dose can cause liver failure without warning. You don’t need a prescription to overdose - just ignorance.
What Happens When You Don’t Understand How a Drug Works
In 2022, the FDA reported that 32% of all adverse drug events came from patients who didn’t understand the mechanism behind their medication. That’s not a small number. That’s nearly one in three people getting hurt because they didn’t know what their pill was actually doing.
One patient took Dimebon, an antihistamine sold in Russia, thinking it might help with memory loss. It showed promise in early trials - until researchers realized its mechanism was unclear. It didn’t target Alzheimer’s pathways the way scientists thought. The trial failed. The drug was pulled. The patients? They lost time, money, and hope.
On the flip side, patients on trastuzumab (Herceptin) for HER2-positive breast cancer were told: “This drug targets the HER2 protein on your cancer cells.” That simple explanation made them more likely to recognize heart problems - a known side effect - and report them early. Those who understood the mechanism were 2.7 times more likely to spot warning signs before serious damage occurred.
It’s not about memorizing biochemistry. It’s about connecting the dots: “This drug does X, so if I feel Y, it might be related.” That’s the difference between fear and informed caution.
How to Learn Your Medication’s Mechanism - Without a Medical Degree
You don’t need to be a scientist to understand how your medicine works. Here’s how to get the facts without the jargon:
- Ask your pharmacist: “How does this drug actually work in my body?” They’re trained to explain it in plain language.
- Look up the drug on Drugs.com or MedlinePlus. Search for “mechanism of action” in the description.
- Ask for a visual. Many clinics now use diagrams showing drug-receptor interactions. A simple sketch of a lock and key can make more sense than a paragraph of text.
- Connect it to symptoms: “If this drug blocks serotonin reuptake, why do I feel nauseous at first?” That’s because your gut has serotonin receptors too. The side effect makes sense.
- Track your diet and habits. If you’re on warfarin, keep a log of leafy greens. If you’re on an MAOI, avoid aged cheeses. Knowledge turns risk into control.
Community pharmacists spend an average of 9 minutes per patient explaining this stuff. That’s time you can use. Don’t be shy. Ask. Repeat it back. “So if I stop this suddenly, the serotonin vacuum opens up and I feel dizzy - is that right?” That’s how you build safety into your routine.
The Bigger Picture: Why This Matters Now
More than 1.3 million people in the U.S. end up in emergency rooms every year because of adverse drug reactions. About 30% of those involve drugs with poorly understood mechanisms. That’s not just bad luck. It’s a failure of communication.
Drug companies now spend 87% of their new applications detailing mechanism of action - up from 62% in 2015. Regulators are forcing them to be clearer. That’s progress. But it only helps if patients are listening.
The future is personal. The NIH’s All of Us program is collecting genetic data from a million people to predict who will react badly to which drug. By 2028, we might have digital twins - computer models of your body that simulate how a drug will affect you before you even take it.
But that future won’t help you today if you don’t know what’s in your medicine cabinet - or why it’s there.
Medicines are powerful tools. They save lives. But they can also hurt you - not because they’re bad, but because you don’t know how they work. Understanding mechanism isn’t academic. It’s survival.
Know your drug. Know why it’s prescribed. Know what to watch for. That’s the only real safety net you have.








Karen Mccullouch
December 12, 2025 AT 17:28 PMI don't care how it works, I just want it to stop my anxiety. Why do you people make everything so complicated? 🤦♀️
Michael Gardner
December 14, 2025 AT 09:28 AMActually, the whole 'lock and key' metaphor is outdated. Most drugs don't fit neatly like that - they're more like sticky magnets with unpredictable drift. This post is oversimplifying pharmacology for clicks.
Willie Onst
December 15, 2025 AT 21:33 PMI love this. Seriously. I used to take meds like candy until I learned how they actually worked. Now I know why my SSRIs made me feel like a zombie at first - my gut was screaming. It’s wild how your body talks back if you listen. 🙏
Jennifer Taylor
December 17, 2025 AT 18:13 PMTHEY KNOW. THEY KNOW WHAT THEY’RE DOING. THE PHARMA COMPANIES PLANTED THIS ‘MECHANISM OF ACTION’ BS TO MAKE US THINK WE’RE IN CONTROL. IT’S ALL A DISTRACTION FROM THE REAL AGENDA - YOUR DNA IS BEING TRACKED THROUGH YOUR LIVER METABOLISM. THEY’RE BUILDING A DATABASE. I SAW IT ON A FORUM. DON’T TRUST THE LOCK AND KEY. IT’S A TRAP. 🕵️♀️
Shelby Ume
December 18, 2025 AT 23:15 PMI appreciate the clarity here. For those who feel overwhelmed, remember: you don’t need to become a biochemist. Just ask your pharmacist one question: 'What’s the one thing this drug changes in my body?' That’s enough to start being safe. And if they give you a textbook answer, ask again. You deserve plain language.
Jade Hovet
December 19, 2025 AT 20:47 PMomg YES!! I was on warfarin and totally forgot about the spinach thing 😅 then I ate a kale smoothie and my finger started bleeding for 10 mins 😱 now i keep a little notepad on my fridge. ‘no blue cheese, no kale, no natto’ lol. this post saved my life. 🙌
nina nakamura
December 21, 2025 AT 12:05 PMYou think this is comprehensive? You missed the fact that 70% of drug mechanisms are based on animal studies that don’t translate to humans. You’re promoting pseudoscience wrapped in jargon. If you don’t know the real data, stop giving advice.
Rawlson King
December 22, 2025 AT 08:54 AMThis is why America is falling apart. People think they can self-diagnose with Google and then act like they’re doctors. You don’t need to know the mechanism. You need to take the pill and shut up.
Constantine Vigderman
December 23, 2025 AT 06:06 AMI was skeptical too but after reading this I went to my doc and asked how my blood pressure med works - turns out it blocks a receptor in my kidneys that I didn’t even know existed. Now I get why I get dizzy when I skip a dose 😅 thanks for making me curious again! 💪
Tom Zerkoff
December 24, 2025 AT 01:42 AMThe data presented here is statistically significant and methodologically sound. I commend the author for emphasizing patient agency through mechanistic literacy. However, I would suggest expanding the discussion on pharmacogenomics as a natural extension of this framework, particularly in light of the All of Us initiative. Knowledge is not merely power - it is the foundation of autonomous healthcare.
Yatendra S
December 25, 2025 AT 07:43 AMIf we understand how drugs work... then why do we still have so many people suffering? Maybe the real question is not how they work... but why we need them at all. 🌿