When someone has type 2 diabetes and obesity, medicine alone often isn’t enough. Many people try diet, exercise, and pills for years-only to see their blood sugar creep higher and their weight keep climbing. That’s where metabolic surgery comes in. It’s not just about losing weight. For many, it’s the only treatment that can actually reverse diabetes.
How Much Weight Do People Really Lose?
People who undergo metabolic surgery lose far more weight than those who rely on diet and medication alone. In one major study, patients lost an average of 27.7% of their starting body weight after surgery. Compare that to the control group-people getting medical care only-who lost just 0.2%. That’s not a typo. Almost no weight loss at all.
Long-term data shows the difference holds up. Six years after surgery, patients with severe obesity (average BMI of 45.9) still carried 19.9% less weight than before. The medical therapy group? Just 8.3%. That’s more than double the weight loss.
And it’s not just about the number on the scale. Excess weight loss-meaning weight lost beyond what’s considered healthy for your height-averages around 55% after surgery. That’s a massive shift for someone who’s struggled with obesity for years.
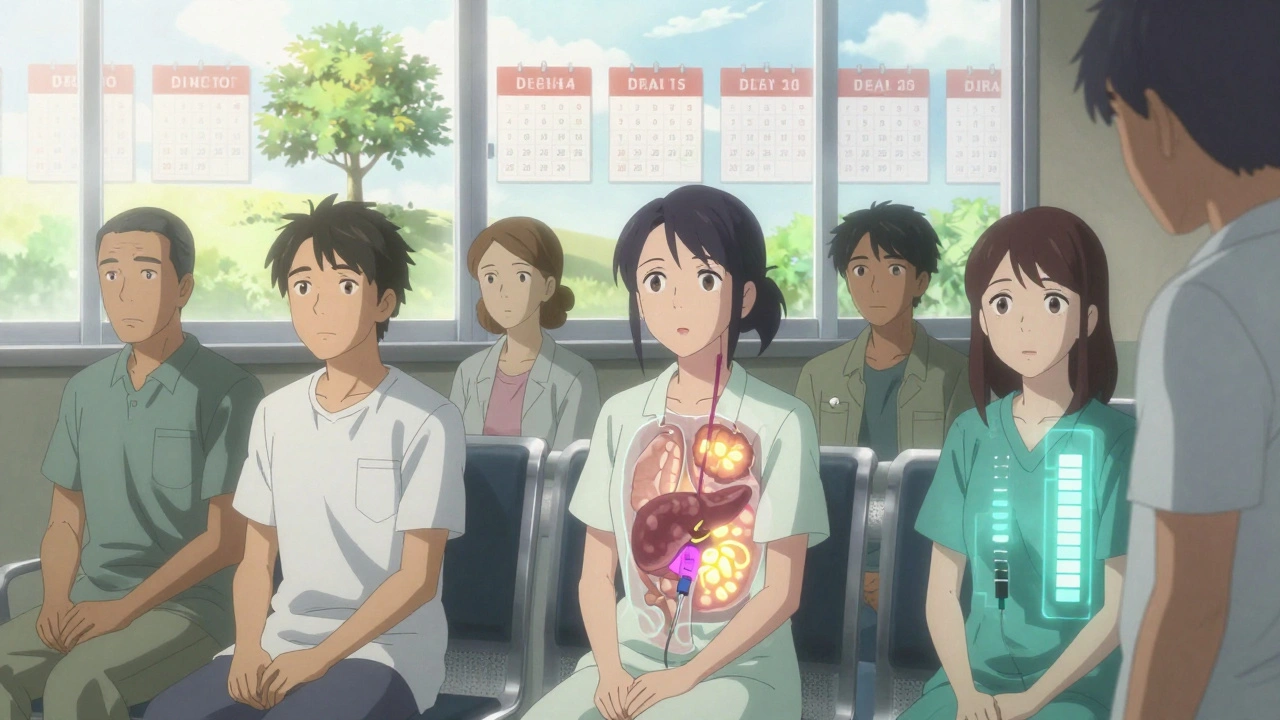
Diabetes Remission: The Real Game-Changer
What makes metabolic surgery stand out isn’t just weight loss-it’s how quickly and strongly it reverses type 2 diabetes. In many cases, blood sugar normalizes within days, even before significant weight is lost. That’s because the surgery changes how the gut talks to the pancreas, triggering hormones that improve insulin sensitivity.
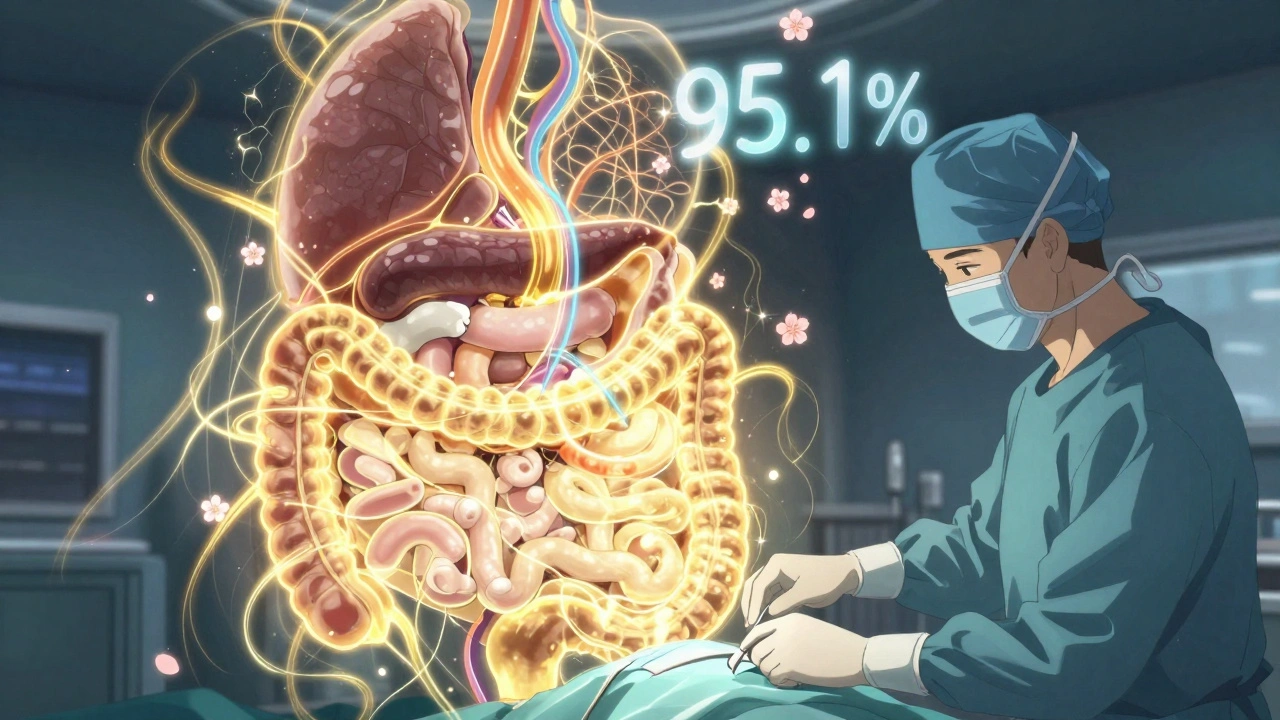
One-year remission rates vary by procedure:
- Gastric bypass (RYGB): 42%
- Sleeve gastrectomy: 37%
- Biliopancreatic diversion (duodenal switch): 95.1%
- Gastric banding: 56.7%
These aren’t theoretical numbers. They come from real patients in large, long-term studies. The duodenal switch has the highest success rate, but it’s also the most complex surgery. Gastric bypass strikes a strong balance between effectiveness and safety.
What Happens After Five Years?
Here’s the catch: remission doesn’t last forever for everyone. The longer you’re out from surgery, the more likely you are to see some return of diabetes.
At five years:
- Gastric bypass: 29% still in remission
- Sleeve gastrectomy: 23%
- Control group (medical therapy only): Under 5%
Even when diabetes comes back, it’s usually milder. People who had surgery need fewer medications, and their blood sugar stays lower than before. One study found that for every year a patient stayed in remission, their risk of kidney, eye, and nerve damage dropped by 19%.
The Swedish Obese Subjects study followed patients for 15 years. Those who had surgery were nearly five times more likely to still be in remission than those who didn’t. That’s not a cure-but it’s a long-term reprieve.
Who Benefits the Most?
Not everyone responds the same way. Your chances of remission depend on several key factors:
- BMI: Lower pre-surgery BMI = better results. Patients with BMI between 24 and 30 had a 93% remission rate after gastric bypass. That’s surprising-many think surgery is only for people with BMI over 40.
- Insulin use: If you’re already on insulin before surgery, your chances drop. Non-insulin users had a 53.8% remission rate 14 months after surgery. Insulin users? Much lower.
- Duration of diabetes: The longer you’ve had type 2 diabetes, the harder it is to reverse. Early intervention works best.
That’s why guidelines now recommend surgery for people with BMI 30-34.9 if their diabetes isn’t controlled with medication. It’s no longer just for the severely obese.
What Are the Risks?
Metabolic surgery is safe-but not risk-free. The biggest long-term concerns are nutritional:
- Anemia (low iron or B12)
- Bone fractures (due to calcium and vitamin D loss)
- Chronic diarrhea or dumping syndrome
These aren’t common right after surgery. They show up years later if you don’t take your vitamins or skip follow-ups. That’s why lifelong monitoring is non-negotiable. You can’t have surgery and then forget about your health.
Some people also experience weight regain. Studies show remission rates drop over time, partly because of regained weight, but also because the pancreas slowly loses its ability to make insulin-even if you’ve lost the weight.
Why Isn’t Everyone Getting This?
Despite strong evidence, fewer than 2% of eligible patients in the U.S. get metabolic surgery each year. Why?
- Insurance often won’t cover it unless your BMI is 35 or higher-even though studies prove it works for people with BMI 30-34.
- Many doctors don’t bring it up. They assume patients won’t want surgery, or they don’t know the latest data.
- Patients fear complications. The truth? The risk of death from surgery is lower than the risk from uncontrolled diabetes.
Big health organizations like the American Diabetes Association and the International Diabetes Federation have endorsed metabolic surgery since 2016. But adoption lags behind science.
What’s Next?
New, less invasive options are emerging. Endoscopic procedures like intragastric balloons and aspiration systems offer middle-ground solutions-less effective than surgery, but safer than open operations.
Meanwhile, studies are testing whether metabolic surgery should be offered to people with BMI as low as 27. Early results are promising. One study looked at 103 patients with average BMI 25.9-and still saw major improvements in blood sugar.
But here’s the bottom line: metabolic surgery isn’t a magic fix. It’s a tool. It works best when paired with lifelong changes in diet, movement, and medical follow-up. For the right person-someone with type 2 diabetes, excess weight, and failed medication attempts-it’s the most powerful option we have.
It’s not about being "fat." It’s about being sick. And for many, surgery is the path back to health.
Can metabolic surgery cure type 2 diabetes?
Metabolic surgery doesn’t guarantee a permanent cure, but it can lead to long-term remission-meaning blood sugar returns to normal without medication. About 30% of patients stay in remission 15 years after surgery. For many, diabetes symptoms disappear for years, and the risk of complications drops significantly. But remission can fade over time, especially if weight is regained or pancreatic function declines.
Which weight loss surgery works best for diabetes?
Biliopancreatic diversion with duodenal switch has the highest remission rate-nearly 95% in the first year. But it’s the most complex and carries the highest risk of nutritional deficiencies. Gastric bypass is the most balanced option: strong remission rates (around 42% at one year), good long-term results, and manageable risks. Sleeve gastrectomy is simpler and popular, but remission rates drop more over time. The best choice depends on your health, BMI, and willingness to follow lifelong nutrition rules.
Do I need to be severely obese to qualify?
No. While surgery was originally for people with BMI 40+, guidelines now support it for those with BMI 30-34.9 if diabetes isn’t controlled with medication. Studies show people in this group still get strong remission rates-up to 36% complete remission at five years. The key isn’t just weight-it’s how well your diabetes is managed and whether you’ve tried other treatments first.
Will I still need diabetes meds after surgery?
Many people stop all diabetes medications within weeks or months after surgery. Even those who don’t achieve full remission often need far fewer drugs. Some only need metformin or none at all. Insulin users are less likely to stop completely, but even they usually reduce their doses significantly. The goal isn’t always to stop meds-it’s to reduce them safely and improve overall health.
What are the biggest risks after surgery?
The biggest long-term risks are nutritional: low iron, vitamin B12, calcium, and vitamin D. These can lead to anemia, bone fractures, and nerve problems if not monitored. You’ll need blood tests every 6-12 months for life and daily supplements. Other risks include dumping syndrome (rapid stomach emptying), gallstones, and occasional bowel issues. The risk of death from surgery is less than 0.5%-lower than the risk of heart attack or stroke from uncontrolled diabetes.
Is metabolic surgery worth it if I’m not severely overweight?
Yes-if you have type 2 diabetes that’s not under control. Studies show people with BMI 25-30 still get major benefits. One study of patients with average BMI 25.9 found 78% had improved blood sugar control, and 56% achieved remission. The surgery changes how your body handles sugar, not just how much you eat. If you’ve tried everything else and your A1C is still high, surgery may be your best shot at long-term health.






Robert Webb
December 11, 2025 AT 22:50 PMLet me tell you, I’ve seen this play out in my clinic for over a decade. People come in with HbA1c in the 9s, on three meds, still gaining weight-then they get gastric bypass, and six months later, they’re off everything, walking their kids to school, and actually sleeping through the night. It’s not magic. It’s physiology. The gut-brain axis flips a switch. Insulin sensitivity doesn’t just improve-it resets. And yes, some regain weight later, but even then, their A1c stays 2 points lower than before surgery. That’s not a win-it’s a revolution. We’re treating a metabolic disease, not just obesity. The data’s been clear since 2009. Why are we still arguing about this?
Adam Everitt
December 13, 2025 AT 07:37 AMso i read this and im like… wait… so surgery fixes diabetes? like… for real? not just ‘oh i lost weight so now im better’? i mean, i get the numbers but it still feels like sci-fi. like, my uncle had the sleeve and he still eats pizza every sunday and his sugar’s normal? weird. also, why do they call it ‘metabolic’? sounds like a buzzword. but… yeah. kinda makes sense. kinda.
wendy b
December 13, 2025 AT 11:34 AMWhile I appreciate the anecdotal evidence presented here, I must emphasize that the methodological rigor of the cited studies is questionable at best. The Swedish Obese Subjects trial, for instance, was not randomized in the modern sense, and the control group’s adherence to medical therapy was likely suboptimal. Furthermore, the definition of ‘remission’ varies across studies-some use fasting glucose, others HbA1c, and none consistently account for post-surgical nutritional supplementation. Until we have double-blind, placebo-controlled trials-which, frankly, would be unethical-we are merely observing correlation, not causation. This is not medicine. It’s marketing dressed in peer-reviewed clothing.
Rob Purvis
December 14, 2025 AT 01:17 AMJust want to add-this is one of those rare cases where the science is SO clear, and the public perception is SO far behind. I’ve had patients who were told by their PCPs, ‘You’re not obese enough,’ even though their A1c was 9.5 and they were on insulin. And then they went to a bariatric center, got the bypass, and now they’re hiking in Colorado. The real tragedy? The insurance denials. The 2% stat? That’s criminal. We’re letting people suffer, lose limbs, go blind-because someone in an insurance office thinks BMI 32 isn’t ‘severe enough.’ The ADA, IDF, NIH-they all say it’s appropriate. So why are we still stuck in the 1990s?
Also, if you’re reading this and you’re on insulin and thinking, ‘I’m too far gone’-you’re not. The data shows even insulin users get better. Just… not as dramatically. But better is still better.
Laura Weemering
December 15, 2025 AT 04:11 AMThey never tell you about the depression after. You lose 100 pounds, your diabetes is ‘in remission,’ everyone’s proud of you… but then you realize you’re still the same person. The food wasn’t the problem. The trauma was. And now you have a scar, a vitamin regimen, and no one talks about the grief of losing your comfort. I’m not saying don’t do it-I did it. But don’t pretend it’s a happy ending. It’s a new beginning with a lot of ghosts.
Audrey Crothers
December 16, 2025 AT 22:04 PMOMG YES. My sister had the sleeve last year and she’s been off metformin since month 2. She cried the first time her glucose meter read 89. 😭 I’ve never seen someone so alive. She’s dancing again. Cooking. Traveling. And she takes her vitamins like a boss. Yes, it’s hard. Yes, you have to change everything. But if you’re tired of being sick-this is your sign. You’re not weak for wanting this. You’re brave. 💪❤️
Stacy Foster
December 17, 2025 AT 08:27 AMTHIS IS A PHARMA COVER-UP. They don’t want you to know you can cure diabetes with surgery because pills and insulin make them TRILLIONS. The ‘nutritional deficiencies’? That’s just the side effect they want you to blame so you keep buying their supplements. And ‘weight regain’? That’s because they’re slowly poisoning your metabolism with synthetic vitamins and pushing you back into the system. The real cure is fasting, clean eating, and avoiding hospitals. They don’t want you to know surgery works because it’s too cheap. Too simple. Too real.
Reshma Sinha
December 18, 2025 AT 09:30 AMAs a diabetologist in Mumbai, I see this daily. Patients with BMI 28, HbA1c 8.5, on metformin + sitagliptin, still progressing. We offer sleeve gastrectomy-it’s affordable here, and outcomes mirror the U.S. data. One patient, a schoolteacher, went from 180 lbs to 120 lbs. Now she runs 5Ks. Her daughter’s teacher said, ‘Your mom looks so happy!’ That’s not just weight loss. That’s dignity restored. We need global access. This isn’t a luxury. It’s a right.
Lawrence Armstrong
December 18, 2025 AT 10:40 AMMy cousin had the duodenal switch. Lost 140 lbs. No diabetes. But then she had a stroke at 42. Turns out her B12 was 120. They didn’t monitor her. She’s on a feeding tube now. So yeah, ‘remission’ sounds great… until your body starts falling apart because no one taught you how to survive after surgery. This isn’t a solution. It’s a gamble with your future. And the docs? They just smile and say, ‘Take your vitamins.’ Like that’s enough.