Antivirals can save lives. But they only work if you take them right-and if the virus doesn’t fight back. Every missed dose, every skipped pill, every time you stop because you feel fine, gives the virus a chance to mutate. And once it does, your medication might not work anymore. This isn’t science fiction. It’s happening right now in people taking antivirals for HIV, hepatitis B, herpes, and even flu.
How Antivirals Lose Their Power
Viruses don’t sit still. They copy themselves over and over, and each time they make a mistake-a mutation-that mistake can sometimes make them invisible to the drug. This isn’t your body getting used to the medicine. It’s the virus evolving. The more the virus reproduces while the drug is around, the more chances it has to slip past the treatment. Take HIV. Back in the 90s, people took just one drug-zidovudine (AZT). Within a few years, most of them developed resistance. The virus changed just enough to ignore the drug. Today, we use combo pills with three or four drugs at once. That’s because it’s harder for a virus to mutate in four different ways at the same time. Still, resistance happens. The M184V mutation, for example, pops up in people who miss doses of drugs like lamivudine or emtricitabine. That one change knocks out those drugs completely. Hepatitis B is another story. Lamivudine, once a go-to, now fails in up to 70% of people after five years. Why? Low genetic barrier. That’s a fancy way of saying the virus only needs one tiny change to escape the drug. Adefovir, on the other hand, needs several changes. That’s why doctors now avoid single-drug treatments for chronic viruses. Combination therapy isn’t optional-it’s the baseline. For herpes, acyclovir resistance is rare in healthy people but common in those with weakened immune systems. Over 90% of resistant cases come from mutations in the virus’s thymidine kinase gene. That’s the enzyme the drug needs to activate. No enzyme, no drug effect. And once resistance shows up, your options shrink fast. Foscarnet or cidofovir might work-but they’re harder to take, and resistance to those can follow too.What You Might Feel While Taking Antivirals
Side effects aren’t the same for everyone. But some show up often enough to be predictable. For HIV meds, nausea, headaches, and fatigue are common in the first few weeks. Most fade. But some people get longer-term issues: weight gain, higher cholesterol, or bone thinning. Modern drugs like dolutegravir and bictegravir are better tolerated than older ones, but they’re not magic. A 2022 survey found 31% of HIV patients skipped doses because of side effects. Hepatitis C treatments today are a huge leap forward. Most are taken as one pill a day for 8 to 12 weeks. Side effects? Fatigue (23%), headache (18%), and mild nausea. Compared to the old interferon regimens-where people had fever, depression, and flu-like symptoms for a year-this is a win. But even these newer drugs aren’t side effect-free. And if you’re on multiple meds for other conditions, interactions can add to the burden. Herpes suppressive therapy with valacyclovir? Usually well-tolerated. Headache and stomach upset are the most common. But if you’re taking it daily for years, kidney function should be checked now and then. Antivirals like cidofovir can be harsh on kidneys. Even if you feel fine, lab work matters. The biggest mistake? Assuming side effects mean you should quit. Most are temporary. Talk to your doctor before stopping. There’s often a fix: switching meds, adjusting the dose, or adding something for nausea. Quitting? That’s how resistance starts.Why Missing a Dose Isn’t Just an Oops
You’re on vacation. You forget your pills. Or you’re tired, and you skip tonight’s dose because you’ll take two tomorrow. Sounds harmless, right? It’s not. When you miss a dose, drug levels in your blood drop. That’s when the virus gets a window to replicate. Every time it copies itself, it’s rolling the dice on a mutation. One mutation won’t kill the drug. But if it happens over and over, the virus builds up a shield. Data shows this clearly. In HIV, people who miss more than 5% of doses have a much higher chance of developing resistance. One study found that patients who took their meds 95% of the time had less than 5% resistance after five years. Those who took them 80% of the time? Over 40% developed resistance. And it’s not just HIV. For hepatitis B, even small gaps in dosing can trigger resistance. For herpes, skipping suppressive therapy can lead to more outbreaks-and more chances for the virus to adapt. It’s not about being perfect. It’s about staying close to perfect. If you miss one dose, take it as soon as you remember. If it’s almost time for the next, skip it. Don’t double up. But don’t treat it like a free pass.
Real Strategies to Stay on Track
You don’t need willpower. You need systems. Pill organizers are used by 63% of people who stick with their meds. A simple weekly box with morning and night compartments makes it obvious if you’ve missed one. No guessing. Phone reminders work for 57% of adherent patients. Set two: one for when to take it, one as a backup an hour later. Label the alarm: “Take HIV pill” or “Valacyclovir.” Don’t just say “Meds.” Link it to a habit. Take your pill after brushing your teeth. After your morning coffee. Right before bed. Anchor it to something you already do every day. Use apps. There are free ones designed for antivirals. They track doses, send alerts, and even let you share your progress with your doctor. Some sync with your pharmacy so refills auto-request. Ask for help. Pharmacist-led counseling cuts resistance rates by 28%. They don’t just hand out pills-they explain why adherence matters, help you pick the right tools, and adjust your plan if side effects are a problem. Carry extras. If you travel, pack two weeks’ worth. Keep a spare set at work or in your bag. If you’re out and forget, you won’t panic.What’s New-and What’s Next
The good news? Antivirals are getting smarter. Lenacapavir, approved in 2023, is a new HIV drug that blocks the virus’s outer shell. It’s taken just twice a year. And in trials, no one developed resistance. That’s unheard of. For hepatitis C, cure rates now exceed 95%. Resistance is rare because modern combos hit the virus in multiple places at once. You’re not just fighting one enemy-you’re overwhelming it. Doctors now recommend resistance testing before starting treatment for HIV and HBV. That wasn’t standard five years ago. Now, it’s routine. It tells your doctor which drugs will work from day one. And research is moving fast. CRISPR gene editing is being tested to cut HIV out of human DNA. Early results show a 60% drop in hidden virus reservoirs-without triggering resistance. It’s not ready yet, but it’s proof we’re not stuck.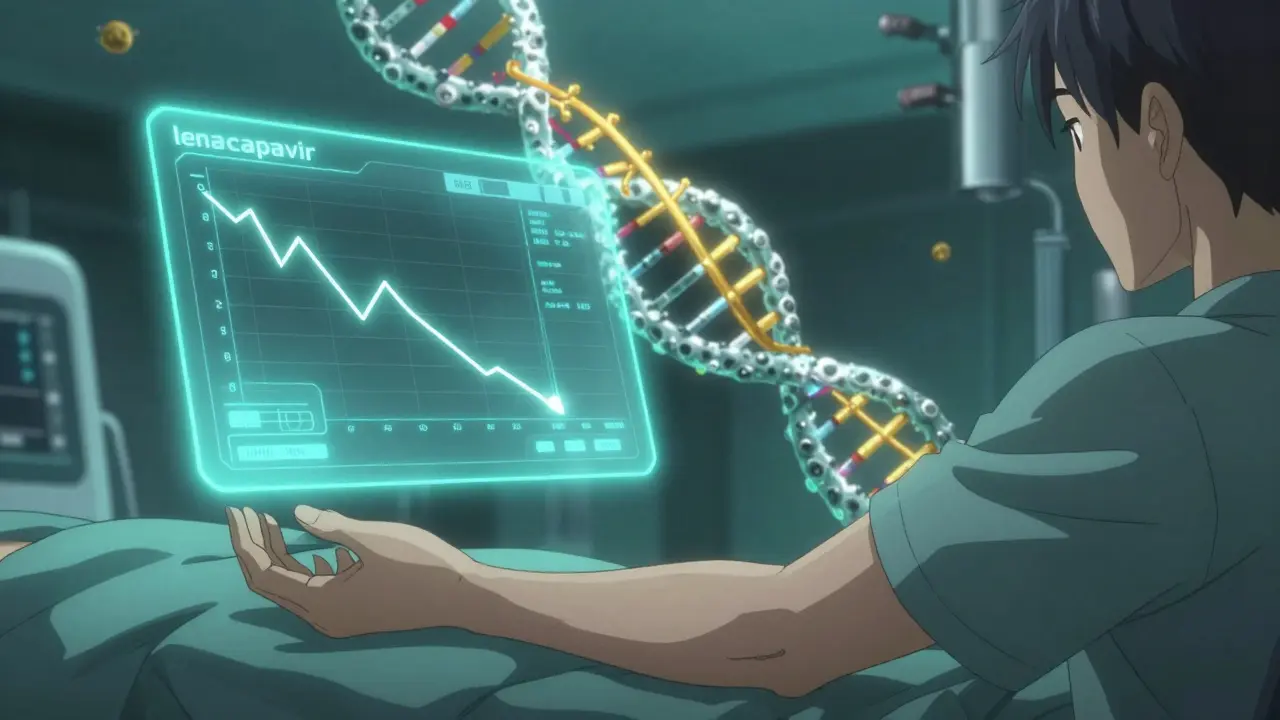
What to Do If You Think Resistance Has Happened
If your viral load suddenly rises, or you’re having more outbreaks than usual, don’t assume it’s stress or bad luck. Get tested. Resistance testing isn’t just for HIV. It’s available for HBV, HCV, HSV, and CMV. A simple blood or swab test can tell you which drugs the virus is still sensitive to. If resistance is confirmed, your doctor won’t just switch you to another drug. They’ll pick a combo that the virus hasn’t seen before-drugs from different classes with no cross-resistance. That’s why knowing your full history matters. Never start a new antiviral without knowing what you’ve taken before. That information saves lives.Bottom Line: Your Dose Is Your Defense
Antivirals are powerful. But they’re not magic bullets. They need you to be consistent. Every pill you take is a barrier against mutation. Every missed dose is a crack in that wall. Resistance isn’t inevitable. Side effects can be managed. Adherence isn’t about discipline-it’s about design. Build your system. Use the tools. Talk to your pharmacist. Ask questions. Don’t wait until something goes wrong. The goal isn’t just to survive. It’s to stay ahead of the virus. And that starts with the next pill you take.Can antivirals cause long-term damage?
Some antivirals can affect kidneys, bones, or metabolism over time-especially with years of use. But modern drugs are much safer than older ones. Regular blood tests and check-ups catch problems early. For most people, the risks of uncontrolled infection far outweigh the risks of the medication.
If I feel fine, do I still need to take my antiviral?
Yes. Many viruses, like HIV and hepatitis B, can be silent. You might feel great, but the virus is still there, quietly copying itself. Stopping treatment-even if you feel fine-gives it the chance to mutate and become resistant. Treatment isn’t about how you feel. It’s about keeping the virus suppressed.
Are generic antivirals as effective as brand-name ones?
Yes. Generic antivirals must meet the same FDA standards as brand-name drugs. They contain the same active ingredient, in the same amount, and work the same way. The only differences are in inactive ingredients (like fillers) or packaging. Most people switch to generics without issue-and save a lot of money.
Can I drink alcohol while taking antivirals?
It depends. For HIV meds, moderate alcohol is usually fine. But heavy drinking can worsen liver damage, especially if you have hepatitis B or C. For some antivirals like ganciclovir or foscarnet, alcohol can increase side effects. Always check with your doctor or pharmacist. When in doubt, skip it.
What should I do if I run out of my antiviral?
Don’t wait until you’re out. Set refill reminders. If you do run out, contact your pharmacy or doctor immediately. Going without-even for a few days-can trigger resistance. Some clinics offer emergency supplies. Never share your meds with someone else or try to stretch your supply by cutting doses.
Is resistance permanent?
Once a resistant strain develops, it stays in your body-even if you switch drugs. But it doesn’t always dominate. If you stop using the drug that caused the resistance, the original, non-resistant virus may come back over time. Still, the resistant version doesn’t disappear. That’s why future treatment options need to be chosen carefully based on your resistance history.
If you’re on antivirals, you’re not just treating a virus-you’re protecting your future health. Stay consistent. Stay informed. And don’t go it alone.




Ryan Riesterer
January 22, 2026 AT 11:53 AMAntiviral resistance is fundamentally a population dynamics problem. Viral replication error rates, selective pressure from suboptimal drug concentrations, and fitness trade-offs create a stochastic evolutionary landscape. The M184V mutation in HIV, for instance, confers high-level resistance to lamivudine but reduces viral replicative capacity by 30–50%. This is why adherence thresholds above 95% are non-negotiable - below that, the selective advantage of resistant variants outweighs their intrinsic fitness cost.
Combination therapy works not because it’s ‘harder’ for the virus to mutate, but because the probability of simultaneous, compensatory mutations across multiple targets is exponentially lower. Think of it as requiring a 4-digit PIN instead of a 1-digit one. The math is clear.
For HBV, the genetic barrier concept is critical. Lamivudine has a barrier of 1, adefovir ~2, tenofovir ~3. That’s why monotherapy is obsolete. Resistance isn’t failure - it’s predictable biology.
And yes, resistance testing before initiation is now standard of care. We’ve known this since 2010. The fact that it’s still not universal in primary care is a systemic failure, not a patient one.
Mike P
January 23, 2026 AT 16:53 PMMan, I’ve seen so many people just quit their HIV meds because they got a little bloated or had a headache. Like bro, you’re not trying to look hot at the beach - you’re trying to stop a virus from turning your immune system into a ghost town.
And yeah, generics? Same damn pills. I got my tenofovir for $5 a month at Walmart. Brand name was $1200. Don’t let the pharma ads fool you.
Also - don’t be that guy who skips doses because ‘I feel fine.’ You’re not the boss of the virus. It doesn’t care how you feel. It just wants to copy itself.
And if you’re on valacyclovir and think you can skip it when you’re not having an outbreak? You’re playing Russian roulette with your immune system.
Hilary Miller
January 24, 2026 AT 10:16 AMMy mom’s on HBV meds. She uses a pill box and sets a reminder labeled ‘Liver Savior.’ It’s simple, but it works.
Don’t overcomplicate it. Just take it.
Tatiana Bandurina
January 25, 2026 AT 19:13 PMIt’s interesting how this post frames adherence as a personal responsibility, but ignores the structural barriers: lack of insurance, unstable housing, food insecurity, mental health crises, and the fact that many people are prescribed antivirals without adequate counseling or follow-up.
Blaming patients for missing doses is convenient for clinicians who don’t want to address systemic failures. The 95% adherence threshold is meaningless if you can’t afford the pill, don’t have a fridge to store it, or are too depressed to get out of bed.
Also - why is there no mention of social determinants? Or the fact that 40% of HIV patients in rural America can’t access a pharmacy within 30 miles?
This reads like a brochure for a pharmaceutical conference, not a real-world guide.
Malik Ronquillo
January 25, 2026 AT 23:19 PMMy cousin skipped his herpes meds for a week because he was ‘feeling good’ - guess what? He had the worst outbreak of his life and now his doctor says he’s got a resistant strain.
Don’t be him.
Take your damn pills.
Margaret Khaemba
January 25, 2026 AT 23:47 PMI’m a nurse and I’ve seen this over and over. People think antivirals are like antibiotics - take them until you feel better. But viruses don’t work that way. Even when you feel fine, the virus is still hiding in your cells.
One of my patients stopped her HIV meds for two weeks during a family emergency. She came back with a viral load that had doubled. We had to switch her entire regimen.
It’s not about willpower. It’s about making it automatic. I tell my patients: tie it to brushing your teeth. Set two alarms. Use a pill box. Do whatever it takes.
And please - don’t be ashamed to ask for help. Pharmacies have adherence counselors now. They’re there to help, not judge.
Akriti Jain
January 26, 2026 AT 14:26 PMThey say resistance comes from skipping doses... but what if the pills are laced with something else? Why is there no talk about how Big Pharma profits from resistance?
They make the drugs, you get resistant, they sell you the next expensive one. It’s a loop.
And why are the new drugs like lenacapavir so expensive? $30,000 a year? Come on.
They want you dependent. Not cured.
Just saying. 🤔💊🌍
Kenji Gaerlan
January 27, 2026 AT 22:50 PMu/7036 is kinda right tho
why do these drugs cost so much?
my bro got his hiv meds covered by medicaid but the co-pay was still $80 a month
and he works two jobs
so yeah sometimes he skips
not because he’s lazy
but because he’s broke
and nobody talks about that
Brenda King
January 28, 2026 AT 01:30 AMThank you for sharing this. I’ve been on hepatitis C treatment and the side effects were brutal at first - but I kept going because I knew it was temporary.
My advice: keep a journal. Write down how you feel each day. Some days you’ll feel awful - but you’ll also see patterns. Like, ‘oh, I’m always tired after lunch’ - so I take my pill after breakfast instead.
Also - if you’re feeling overwhelmed, reach out. There are online communities where people share real tips. You’re not alone.
And yes - generics work. I saved $2000 switching to one. My doctor didn’t even blink.
You got this. 💪
Oren Prettyman
January 29, 2026 AT 04:56 AMIt is an incontestable and empirically verifiable fact that the narrative surrounding antiviral adherence is fundamentally misaligned with the principles of evolutionary biology and pharmacokinetic modeling. The notion that patient noncompliance is the primary driver of resistance is a reductive and ideologically convenient fallacy propagated by medical institutions seeking to absolve themselves of systemic accountability.
The true locus of resistance lies in the pharmacodynamic inadequacies of dosing regimens, the absence of therapeutic drug monitoring in routine practice, and the institutional failure to implement population-level adherence interventions. The 95% threshold is statistically arbitrary and lacks robust validation in real-world heterogeneous populations.
Furthermore, the promotion of pill organizers and smartphone reminders as primary solutions reflects a profound epistemological disconnect from the lived realities of marginalized communities. The burden of compliance is disproportionately externalized onto individuals who lack the material, cognitive, and social resources necessary for such behavioral interventions to be effective.
Until antiviral therapy is decoupled from neoliberal healthcare economics and restructured as a public health imperative - rather than a private responsibility - resistance will persist, not as a biological inevitability, but as a social catastrophe.
Daphne Mallari - Tolentino
January 29, 2026 AT 06:01 AMWhile the article presents a commendable overview of antiviral resistance mechanisms, it conspicuously omits any discussion of the ethical implications of pharmaceutical patent monopolies that render life-sustaining medications inaccessible to over 30% of the global population.
Moreover, the emphasis on individual behavioral modification - pill boxes, phone reminders - is not merely reductive, but morally suspect when contextualized within the broader landscape of global health inequity.
The assertion that resistance is ‘not inevitable’ is statistically true in high-income settings with universal healthcare, yet ethically bankrupt when applied universally without addressing structural determinants.
One cannot prescribe adherence to a person who cannot afford the prescription.
Sarvesh CK
January 29, 2026 AT 21:20 PMThere is a deeper philosophical question here that the article doesn’t touch on: what does it mean to be responsible for your own health in a world where health is commodified?
We are told to take our pills, to be disciplined, to follow the rules - but we are not given the tools, the time, the safety nets, or the dignity to do so consistently.
Antivirals are not magic. They are tools. But tools require context. A hammer is useless without a nail - and a pill is useless without access, stability, and care.
Perhaps the real breakthrough isn’t in new drugs, but in rethinking healthcare as a right - not a reward for compliance.
Resistance isn’t just viral. It’s systemic.
Alec Amiri
January 31, 2026 AT 14:31 PMLook. I’ve been on HIV meds for 12 years. I’ve missed doses. I’ve been sick. I’ve traveled. I’ve been depressed.
But I never stopped. Because I know what happens when you do.
My viral load was undetectable for 10 years straight. Then I skipped a week because I was in a bad place.
Three months later? Detectable.
They had to switch me. Took me 6 months to get back to undetectable.
Don’t be stupid.
Take your pills.
It’s not about being perfect.
It’s about not being a statistic.
Keith Helm
February 1, 2026 AT 07:06 AMAdherence thresholds are evidence-based. The 95% figure is derived from longitudinal cohort studies with viral load monitoring. To dismiss this as ‘arbitrary’ is to reject clinical epidemiology.
Structural barriers are real. But they do not invalidate biological reality.
Patients must be supported. But they must also be held accountable. The two are not mutually exclusive.
Recommendation: integrate adherence counseling into primary care. Not as an add-on - as a core component.
Philip House
February 2, 2026 AT 18:29 PMY’all are overthinking this.
Antivirals aren’t candy. They’re medicine.
Miss a dose? You’re giving the virus a free pass to evolve.
It’s not about being a good person. It’s about biology.
Viruses don’t care if you’re broke, tired, or depressed.
They just multiply.
So take the damn pill.
And if you can’t? Ask for help.
Not because you’re weak.
But because you’re smart.