Every year, millions of pills, syrups, and injections sit in medicine cabinets, hospital shelves, and ambulances past their expiration dates. Some are harmless. Others can be dangerous. Expired antibiotics lose potency. Insulin can fail. Epinephrine auto-injectors might not work in an emergency. The problem isn’t just about waste-it’s about safety. And technology is finally stepping in to fix it.
Why Tracking Expiration Dates Matters
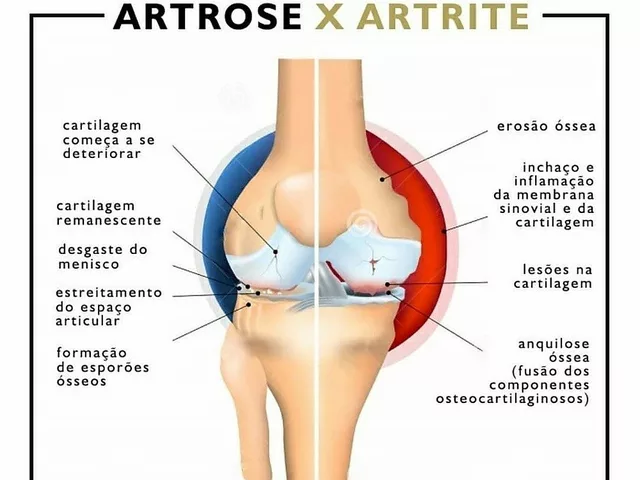
Expiration dates aren’t arbitrary. They’re based on real science: how long a drug stays stable, potent, and safe under normal storage conditions. The FDA allows a small margin of safety, but that doesn’t mean expired meds are fine to use. In hospitals, giving someone an expired drug can lead to treatment failure, allergic reactions, or even death. At home, people often forget when they bought that cough syrup or painkiller-and they take it anyway.
According to the American Hospital Association, over 10% of medications in hospital inventory are expired or near expiration at any given time. That’s not just a financial loss-it’s a patient risk. Technology doesn’t just help you remember-it prevents mistakes before they happen.
RFID: The Game-Changer in Hospitals
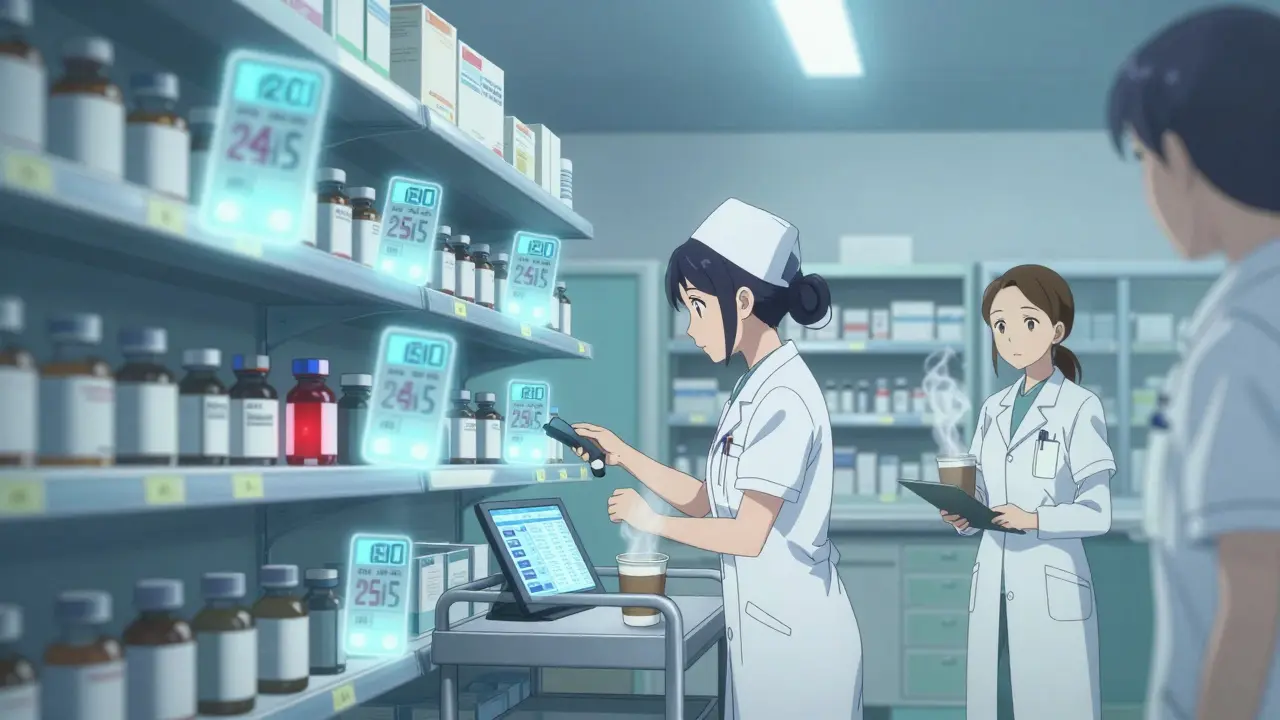
Radio Frequency Identification (RFID) is no longer science fiction. It’s in use at over 900 U.S. hospitals, including major names like Texas Children’s Hospital and UF Health Shands. Each medication bottle or blister pack gets a tiny RFID tag-smaller than a grain of rice. When you scan a drawer, cabinet, or crash cart, the system reads all items at once, in under 30 seconds.
Unlike barcode scanners that need one item at a time, RFID sees everything. It doesn’t just tell you what’s there-it tells you when it expires. Systems like KitCheck automatically flag anything within two days of expiration. If a nurse pulls a vial of insulin that’s expired, the system blocks the transaction and alerts the pharmacy. No more guessing. No more manual logs.
At Texas Children’s, pharmacists used to spend hours manually checking 784 high-value drugs-each costing over $100. With RFID, that task dropped from 8 hours to 15 minutes. And accuracy jumped from 65-75% to 100%. That’s not efficiency. That’s life-saving.
eMAR Systems: For Long-Term Care and Clinics
If you’re not in a big hospital, RFID might be overkill. That’s where eMAR (Electronic Medication Administration Record) systems come in. These are software platforms used by nursing homes, home care agencies, and clinics. They sync with pharmacy orders, track when meds are given, and flag expirations automatically.
eVero’s system, for example, integrates directly with pharmacy databases. When a new prescription arrives, the system logs the expiration date. Then, every time a caregiver administers a dose, they scan the patient’s wristband and the medication. The system checks: Is this still good? Has it been given on time? Is there a recall? If the answer is no, it won’t let them proceed.
These systems are especially powerful for patients with intellectual and developmental disabilities (IDD), where routines matter and memory can be unreliable. Staff don’t have to rely on sticky notes or paper charts. Everything is digital, auditable, and real-time.

Automated Dispensing Cabinets: Smart Storage for Pharmacies
Many hospitals and pharmacies use Automated Dispensing Cabinets (ADCs)-locked drawers that only open when authorized. But modern ADCs do more than store meds. They track every single item inside: lot number, expiration date, who took it, and when.
TouchPoint Medical’s systems, for example, log every interaction. If a drug expires while sitting in the cabinet, the system locks it out. It won’t unlock until someone replaces it. This prevents accidental use and ensures compliance with DEA and FDA rules, especially for controlled substances like opioids.
These cabinets also reduce waste. One study showed hospitals using smart ADCs cut expired medication disposal by 18% in just six months. That’s not just saving money-it’s reducing environmental impact.
Mobile Apps for First Responders and Home Use
Not everyone works in a hospital. Emergency medical teams, home care nurses, and even families need simple solutions. That’s where apps like LogRx come in.
LogRx runs on any iPhone or Android phone. Paramedics scan medication barcodes with their phone’s camera. The app checks the expiration date against the current date. If it’s expired, the app flashes red and blocks the record. No extra hardware. No training required. Portland Fire & Rescue started using it in 2023 and said their DEA compliance paperwork dropped by 70%.
At home, apps like Medisafe and MyTherapy let you enter your pills manually. They send push notifications: “Your blood pressure pill expires in 3 days.” You can even scan the barcode off the box. It’s not hospital-grade, but for someone managing 10+ medications, it’s a game-changer.
What You Need to Get Started
Getting technology to track expiration dates isn’t plug-and-play. It takes planning.
- For hospitals: Start with a pilot-maybe just your crash carts or operating room meds. Budget $50,000-$200,000 for RFID setup. Include staff training. Expect a 3-6 month ramp-up.
- For clinics or nursing homes: Choose an eMAR system with pharmacy integration. Make sure it works with your existing EHR (electronic health record). Training usually takes 2-4 weeks.
- For EMS or home use: Download a trusted app. Test it with one medication first. Make sure it works offline-some areas have spotty internet.
One big mistake? Trying to do everything at once. Start small. Fix one problem. Then expand.

What Doesn’t Work
Not all tech solutions are equal. Some systems require you to manually enter expiration dates. That’s just replacing paper with a screen. It’s slower and more error-prone.
Also, avoid systems that don’t integrate with your existing tools. If your pharmacy uses one system and your nurses use another, data gets lost. Look for interoperability-systems that talk to each other.
And don’t ignore staff buy-in. In one Midwest hospital, RFID failed in the first quarter because nurses didn’t trust the system. They kept overriding alerts. Only after 12 weeks of training and real-time feedback did adoption hit 90%.
The Future Is Already Here
By 2027, Gartner predicts 45% of U.S. hospitals will use RFID for medication tracking. That’s up from just 25% today. Why? Because the ROI is clear.
Hospitals report saving $120,000 to $300,000 a year by cutting expired drug waste. One hospital reduced its pharmacy inventory by 22% because they finally knew what they had. Another cut medication errors by 40%.
Next up: AI that predicts when a drug is likely to expire based on usage patterns. Blockchain to track meds from factory to patient. Manufacturer-pre-tagged drugs that come ready to scan-no extra work for the pharmacy.
This isn’t about tech for tech’s sake. It’s about making sure the right medicine, at the right dose, is given at the right time. And that it hasn’t gone bad.
What You Can Do Today
You don’t need a hospital budget to start.
- Take out your medicine cabinet. Check expiration dates. Toss anything old.
- Download a free app like Medisafe. Add your top 3 meds. Set alerts.
- If you’re a caregiver or nurse, talk to your manager about eMAR or RFID. Show them the data: 15-20% less waste, 75% faster inventory checks.
Technology won’t replace your memory. But it will protect you when your memory fails.
Can I just use a spreadsheet to track medication expiration dates?
You can, but it’s risky. Spreadsheets require manual entry, which leads to mistakes. If someone forgets to update a date, or types it wrong, you won’t know until it’s too late. Technology like RFID or eMAR systems auto-update based on real data from the pharmacy. A spreadsheet might work for one person with three pills-but not for a clinic, hospital, or home with dozens of meds.
Are expired medications dangerous to take?
Some are, some aren’t. Antibiotics, insulin, epinephrine, and nitroglycerin can lose potency and become ineffective or even harmful. A 2012 FDA study found that many solid medications remain stable past their expiration date-but that’s not guaranteed. For critical drugs, you can’t risk it. Always replace anything expired.
Do insurance companies cover medication tracking tech?
Not directly. Insurance doesn’t pay for RFID tags or apps. But hospitals and long-term care facilities can get funding through grants, CMS incentives for reducing medication errors, or state safety programs. For individuals, apps are usually free or low-cost-under $5/month. The real savings come from avoiding hospitalizations caused by expired meds.
What’s the difference between RFID and barcode systems?
Barcodes need to be scanned one at a time, line of sight, and require manual entry of lot numbers. RFID tags can be read through containers, in bulk, and automatically pull expiration data from a database. RFID is faster, more accurate, and reduces human error. But it costs more upfront because each item needs a tag. Barcodes are cheaper but slower.
Can I use my phone to scan medication expiration dates?
Yes, if the medication has a barcode and you use a trusted app like LogRx, Medisafe, or MyTherapy. Simply open the app, point your camera at the barcode, and it reads the expiration date automatically. Some apps even let you take a photo of the label if the barcode is faded. It’s not as robust as hospital systems, but it’s far better than guessing.
How often should I check my home medication expiration dates?
Every 3 to 6 months. Seasonal checkups work well-like when you change your clocks in spring and fall. Toss expired meds safely (don’t flush them). Use a drug take-back program if available. Apps can remind you, but manual checks are still important for pills without barcodes.





Paul Ong
January 3, 2026 AT 00:07 AMRFID in hospitals is a no-brainer. I’ve seen nurses waste hours just checking vials. Now they get alerts before a drug even hits the cart. No more guessing. No more panic. Just clean, fast, safe. This is healthcare finally catching up.
Donna Peplinskie
January 3, 2026 AT 09:51 AMI love that apps like Medisafe are making this accessible to regular people-especially seniors and caregivers. My mom has six different pills, and she forgets everything. Now she gets a little ping on her phone: ‘Don’t take the blue one-it expired last week.’ It’s simple, but it saves lives. Thank you for writing this.
Heather Josey
January 4, 2026 AT 21:12 PMTechnology doesn’t replace human care-it amplifies it. When a nurse isn’t scrambling to check expiration dates manually, they have more time to sit with a patient, explain the treatment, hold their hand. That’s the real ROI. The systems you mentioned? They’re not just tools. They’re enablers of compassion.
Andy Heinlein
January 6, 2026 AT 20:17 PMjust downloaded logrx on my phone. scanned my epi pen. it said expired 3 months ago. i had no idea. thanks for the wake up call. now im checking everything. also i think my cough syrup is from 2019. yikes.
gerard najera
January 8, 2026 AT 15:09 PMExpiration dates are a social contract. Not science. Pharma sets them for liability, not efficacy. The real issue is trust. Do we trust corporations to decide when our medicine dies? Or do we trust data, testing, and transparency?
Stephen Gikuma
January 10, 2026 AT 05:08 AMRFID tags? That’s the government and Big Pharma tracking your meds. Next they’ll implant chips in your arm so they know when you take your insulin. This isn’t safety-it’s control. And who’s really benefiting? Not you. Not me. The corporations.
Bobby Collins
January 11, 2026 AT 06:14 AMmy cousin works at a hospital and says they use these systems but the alarms keep going off and no one listens anymore. its like crying wolf. also i heard the tags can be hacked. you think they’re safe but they’re just another backdoor for the feds.
Layla Anna
January 11, 2026 AT 15:22 PMso cool how this tech is helping in rural clinics too 😊 i saw a video of a nurse in rural Alabama using an app to scan meds for a diabetic patient-no internet, but it worked offline. tech for the people, not just the rich. love this!
Olukayode Oguntulu
January 12, 2026 AT 13:38 PMThe entire paradigm of medication tracking is predicated on a neo-liberal epistemology of quantifiable efficiency, wherein human fallibility is pathologized and outsourced to algorithmic governance. The RFID tag is not a tool-it is a symptom of late-stage pharmaceutical capitalism’s colonization of bodily autonomy. One must ask: who owns the data? Who profits from the expiration event? And why are we not interrogating the ontological violence of the expiration date itself?
jaspreet sandhu
January 13, 2026 AT 20:10 PMYou say technology fixes this but you ignore the real problem-people don’t take care of their meds. In India we don’t have RFID or apps but people still manage their pills because they pay attention. You make it sound like you need a $200,000 system when all you need is a calendar and a little discipline. Technology is a crutch for lazy people who can’t remember to check a date. Also why do you think hospitals waste so much? Because they buy too much. Not because the system is bad. Because they are greedy.