Exemestane Blood Clot Risk Calculator
Risk Assessment Tool
This tool estimates your personalized risk of developing blood clots while taking exemestane based on key factors discussed in the article. Remember, this is for informational purposes only - always consult your doctor for medical advice.
Personalized Risk Assessment
Your estimated blood clot risk while taking exemestane:
This calculation is based on data from clinical studies mentioned in the article, including the MA.27 trial showing a 1.3% VTE rate for exemestane.
Recommendations
When you hear the word exemestane, you probably think of a medication that helps fight breast cancer. But many patients also worry about a less talked‑about side effect: blood clots. This guide breaks down what the research says, who’s most at risk, and how to stay safe while on therapy.
What is Exemestane?
Exemestane is a third‑generation aromatase inhibitor that blocks the enzyme aromatase, dramatically lowering estrogen levels in post‑menopausal women. Lower estrogen slows the growth of hormone‑sensitive breast tumors, making exemetane a cornerstone of adjuvant therapy after surgery or radiation.
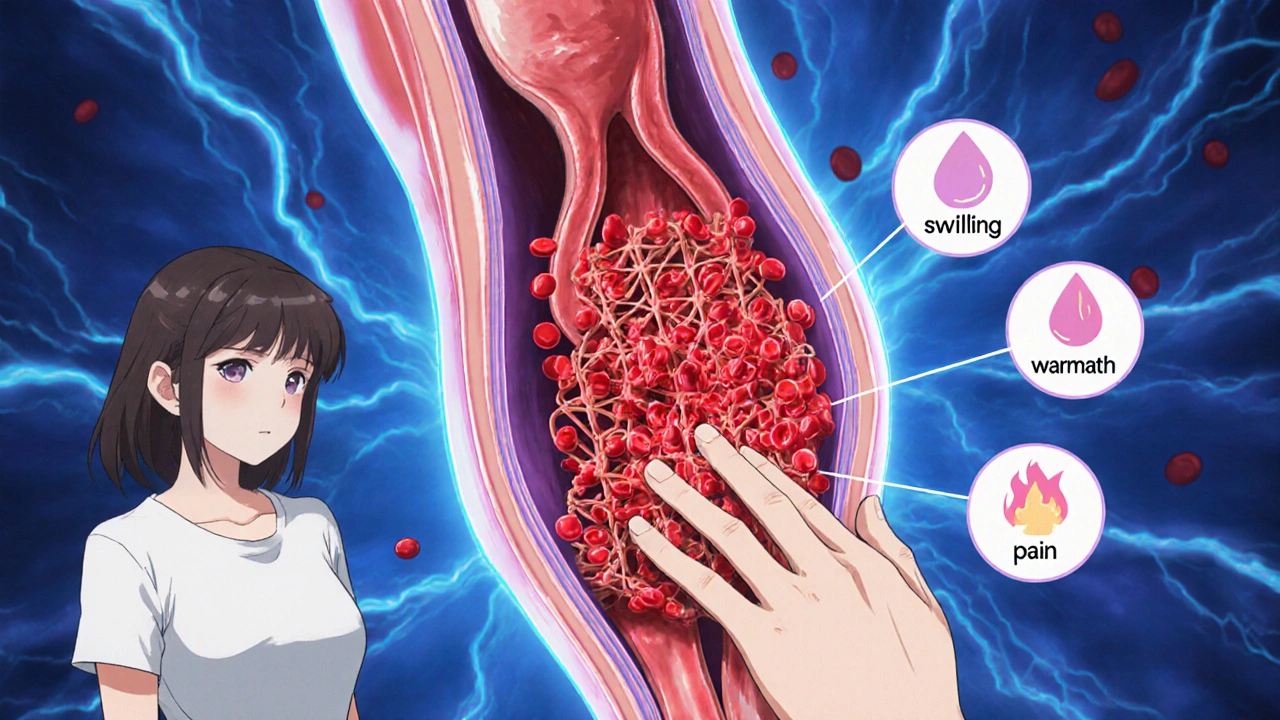
How Blood Clots Form
Blood clotting, or thrombosis, is the body's natural response to vessel injury. Platelets stick together, fibrin strands form a mesh, and the clot seals the wound. Problems arise when clots develop inside veins without an obvious injury, traveling to the lungs (pulmonary embolism, Pulmonary embolism) or blocking leg veins (deep vein thrombosis, Deep vein thrombosis).
Why Exemestane Might Increase Clot Risk
Estrogen has a protective effect on the blood‑vessel lining, partly by promoting a balanced coagulation cascade. By sharply reducing estrogen, exemestane can tip the balance toward clot formation. Clinical trials have shown a modest rise in venous thromboembolism (VTE) rates for aromatase inhibitors compared with placebo, though the increase is usually lower than with older hormone‑blocking drugs like tamoxifen.
What the Numbers Say
Large studies give a clearer picture:
- The ATAC trial (Anastrozole, Tamoxifen, and the Combo) reported a VTE incidence of 1.4% for anastrozole versus 2.1% for tamoxifen over five years.
- The MA.27 trial, which compared exemestane to letrozole in over 7,500 patients, found VTE rates of 1.3% for exemestane and 1.5% for letrozole-a statistically insignificant difference.
- A 2023 meta‑analysis of 12 randomized studies (totaling 13,800 women) concluded that aromatase inhibitors, as a class, raise VTE risk by about 0.5% compared with no hormonal therapy.
In plain terms, the absolute increase is small, but for someone with other risk factors, it can be meaningful.
Who Is Most at Risk?
Understanding personal risk helps you and your doctor make better decisions. The following factors stack the odds:
- Age over 65 - blood vessels become less flexible.
- Obesity (BMI ≥ 30) - excess fat releases pro‑coagulant hormones.
- Current smoking - damages the endothelium.
- Previous VTE episode - scar tissue can trap clots.
- Concurrent hormone replacement therapy or tamoxifen use - additive estrogen‑modulating effects.
If you tick more than one box, ask your oncologist for a deeper risk assessment.
Spotting the Warning Signs
Early detection saves lives. Keep an eye out for these symptoms:
- Sudden swelling, warmth, or pain in one leg - classic DVT cue.
- Shortness of breath, chest tightness, or rapid heartbeat - possible pulmonary embolism.
- Unexplained fatigue or calf tenderness - may indicate a clot forming.
Any of these signs warrant immediate medical attention, especially while on exemestane.
Managing a Blood Clot Event
If a clot is diagnosed, the usual steps are:
- Pause exemestane - the drug’s estrogen‑lowering effect can worsen clotting.
- Start anticoagulation therapy (e.g., low‑molecular‑weight heparin, then a direct oral anticoagulant) for at least three‑to‑six months.
- Discuss alternative breast‑cancer treatments - options include switching to another aromatase inhibitor with a slightly different safety profile or moving to ovarian suppression plus an alternate endocrine agent.
Most patients resume cancer therapy after the clot stabilizes, but the timeline varies.

Comparing Aromatase Inhibitors: Clot Risk at a Glance
| Drug | Mechanism | VTE Incidence (5‑yr) | Notes |
|---|---|---|---|
| Exemestane | Irreversible steroidal inhibitor | ~1.3% | Lowest VTE among AIs in MA.27 |
| Letrozole | Non‑steroidal reversible inhibitor | ~1.5% | Similar to exemestane, slight rise in older patients |
| Anastrozole | Non‑steroidal reversible inhibitor | ~1.4% | Comparable to exemestane in most trials |
While differences are modest, patients with high baseline VTE risk may prefer exemestane, which appears slightly safer in head‑to‑head data.
Practical Tips to Lower Your Clot Risk While on Exemestane
- Stay active - short walks or gentle stretching keep blood flowing.
- Maintain a healthy weight - aim for BMI under 30 if possible.
- Avoid long‑haul flights without moving - stand up and stretch every hour.
- Quit smoking - nicotine damages vessel walls and raises clot chances.
- Discuss any hormone therapy - combining exemestane with HRT can amplify risks.
These lifestyle moves won’t eliminate risk, but they give your circulatory system a solid boost.
When to Talk to Your Doctor
Good communication can catch problems early. Schedule a check‑in if you notice any of the warning signs, if you start a new medication that might interact with anticoagulants, or if you develop chronic health issues like diabetes or high blood pressure that could affect clotting.
Bottom Line
Exemestane remains a highly effective option for hormone‑sensitive breast cancer, and its absolute increase in blood‑clot risk is modest. Knowing your personal risk factors, watching for symptoms, and adopting a clot‑friendly lifestyle can keep you safe while you benefit from the drug’s cancer‑fighting power.
Does exemestane cause blood clots more often than other aromatase inhibitors?
Large trials such as MA.27 show a VTE rate of about 1.3% for exemestane, which is slightly lower than the 1.5% seen with letrozole and comparable to anastrozole. The overall difference is small, but individual risk factors matter.
What are the early signs of a deep vein thrombosis?
Look for unexplained swelling, warmth, or tenderness in one leg, especially if the calf feels tight or painful when you walk.
If I develop a clot, can I stay on exemestane?
Usually the drug is paused while you receive anticoagulation therapy. After the clot stabilizes, your oncologist may restart exemestane or switch to another endocrine agent, depending on your overall risk profile.
Are there lifestyle changes that reduce clot risk while on exemestane?
Yes. Regular movement, maintaining a healthy weight, staying hydrated, avoiding prolonged immobility, and quitting smoking all help keep blood flowing smoothly.
Should I get routine blood tests to monitor clot risk?
Standard practice does not require regular clot‑specific labs unless you have a history of VTE or other risk factors. Your doctor may check D‑dimer levels or platelet counts if concerns arise.











barnabas jacob
October 20, 2025 AT 19:58 PMYo, this whole exemestane VTE spiel reads like a buzzword‑laden “big pharma” brochure, slapping around terms like ‘coagulation cascade’ without even addressing the real patient‑level ramifications – like why the average Jane should care about a 0.5% stat while juggling chemo side‑effects.
jessie cole
November 2, 2025 AT 07:03 AMDear fellow reader, I truly appreciate the fervor expressed, yet allow me to elucidate in a measured yet heartfelt manner: while the statistical increment appears modest, the gravity of a potential thrombotic event cannot be dismissed. It is incumbent upon us to balance clinical efficacy with vigilant monitoring, thereby safeguarding both oncologic outcomes and vascular integrity.
Deja Scott
November 14, 2025 AT 19:08 PMIndeed, the discourse surrounding aromatase inhibitors often omits the broader sociocultural backdrop that shapes patient experiences. In many communities, access to regular follow‑up imaging or laboratory monitoring remains limited, which can exacerbate anxiety over even marginal risk percentages. Moreover, the language used in clinical trials frequently presumes a level of health literacy that is not universally held, creating barriers to informed consent. When we consider the elderly population, who already contend with comorbidities such as hypertension and diabetes, the cumulative risk profile becomes more nuanced. A 65‑year‑old patient with a BMI of 32, for instance, may perceive a 1.3% VTE rate as substantially higher than a younger, lean counterpart. Cultural beliefs about medication adherence also play a pivotal role; some patients may prioritize traditional remedies over prescribed endocrine therapy, inadvertently altering their risk landscape. It is essential, therefore, for clinicians to tailor counseling sessions that integrate these sociocultural determinants, rather than relying solely on generic risk equations. Education materials should be translated into multiple languages and delivered in formats that respect varying literacy levels. Additionally, incorporating family members into the discussion can provide a support network that reinforces adherence and vigilance for early signs of thrombosis. While the absolute increase in clot risk is statistically modest, the psychological impact of fearing a life‑threatening event can be profound, sometimes influencing treatment decisions more than the numbers themselves. Hence, a multidisciplinary approach that includes oncology, primary care, and mental health professionals is advisable. Patient‑reported outcome measures can further illuminate the lived experience of those on exemestane, guiding adjustments in dosage or regimen when appropriate. In summary, the intersection of biomedical data with cultural context dictates that we move beyond a one‑size‑fits‑all paradigm, embracing a patient‑centered model that truly reflects the diversity of our societies.
Natalie Morgan
November 27, 2025 AT 07:13 AMInteresting points but notice how obesity and smoking compound the VTE odds leading to a layered risk profile
Mahesh Upadhyay
December 9, 2025 AT 19:18 PMLet’s cut the fluff – the data screams that exemestane’s clot numbers are barely a blip, yet the media loves drama over nuance.
Rajesh Myadam
December 22, 2025 AT 07:23 AMI hear your frustration, and I think it’s important we acknowledge both the statistical reassurance and the genuine worries patients may feel, especially when they’ve been through so much already.
Andrew Hernandez
January 3, 2026 AT 19:28 PMFrom a public health angle, encouraging regular movement and weight management can offset many of the modest risks outlined.
Alex Pegg
January 16, 2026 AT 07:33 AMWhile you champion lifestyle tweaks, it’s worth remembering that Western guidelines often ignore genetic predispositions common in our own population, making blanket advice problematic.
laura wood
January 28, 2026 AT 19:38 PMStay active and hydrate.
Kate McKay
February 10, 2026 AT 07:43 AMGreat reminder! Regular walks, especially after long flights, can keep circulation flowing, and sipping water throughout the day helps maintain blood viscosity at healthy levels.