What Is Myxedema Coma?
Myxedema coma isn’t just a bad case of hypothyroidism-it’s a full-body shutdown. It happens when your thyroid hormone levels drop so low that your brain, heart, lungs, and metabolism start failing. Once called "myxedema coma" because patients often lost consciousness, the term has evolved. Now, doctors call it myxedema crisis because you don’t need to be comatose to be in danger. Even severe confusion, extreme fatigue, or unresponsiveness can signal this emergency.
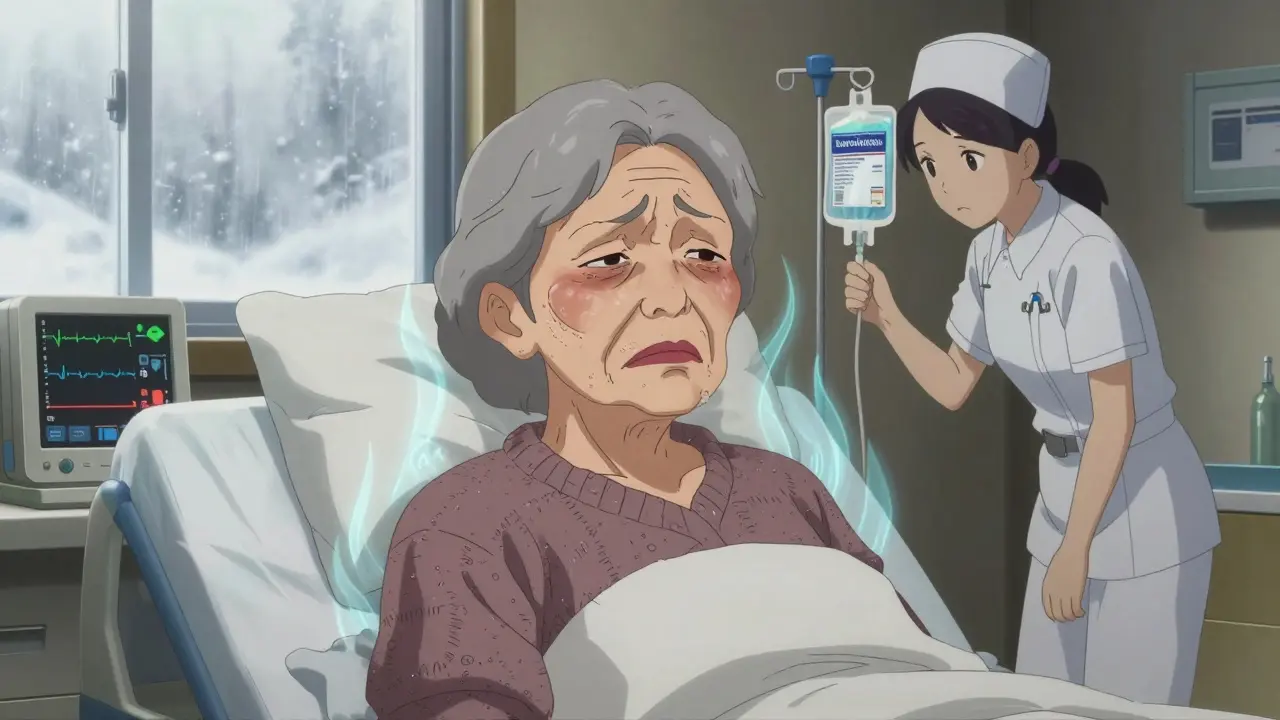
This condition doesn’t come out of nowhere. It usually builds over months or years in people with untreated or poorly managed hypothyroidism. Most patients are women over 60, and it’s far more common in winter. Cold weather alone can push a fragile system over the edge. One patient in Seattle described wearing three layers inside a heated home because she felt like she was freezing-even in 75°F weather. That’s not just being cold. That’s your body losing its ability to regulate temperature.
How Do You Know It’s Happening?
The signs aren’t subtle. If someone has severe hypothyroidism and suddenly seems "off," watch for these red flags:
- Altered mental status: Slurred speech, confusion, lethargy, or unresponsiveness. In older adults, it often looks like depression or dementia.
- Hypothermia: Core body temperature below 95°F (35°C). This isn’t just feeling chilly-your body can’t generate heat anymore.
- Slow heart rate: Heartbeats under 60 per minute, sometimes as low as 30.
- Shallow breathing: Fewer than 12 breaths per minute. Carbon dioxide builds up because your lungs aren’t working hard enough.
- Swelling: Puffy face, droopy eyelids, thickened lips, swollen legs. This isn’t water retention you can press and leave a dent-it’s non-pitting edema, a hallmark of long-term thyroid failure.
- Low blood pressure and weak pulse: Your heart can’t pump effectively without thyroid hormone.
Lab tests back this up: sodium levels drop below 135, TSH soars past 100 mIU/L, and free T4 plummets under 0.9 ng/dL. But here’s the catch-you can’t wait for labs. If you see these symptoms, treat immediately.
Why Is This So Dangerous?
Myxedema coma kills. Between 25% and 60% of patients die, even with modern care. Why? Because it’s often missed. Doctors mistake it for infection, stroke, drug overdose, or psychiatric illness. A 68-year-old woman in Texas spent 18 months being treated for depression before she collapsed. Her thyroid medication had been stopped during a hospital stay for pneumonia. That’s not rare.
Unlike diabetic ketoacidosis or adrenal crisis, there’s no single lab number that confirms myxedema coma. It’s a clinical diagnosis. That means if you suspect it, you treat it-no waiting. Delaying treatment by even one hour increases the chance of death by 10%. In rural areas or places with limited lab access, patients wait 6 to 12 hours for results. In hospitals with protocols, treatment starts in under two hours-and survival rates jump.

Emergency Protocol: What to Do Right Now
There’s a clear, step-by-step plan for handling myxedema coma. Follow it exactly.
- Secure the airway: Half to 70% of patients need intubation. Their breathing is too slow to keep oxygen up and carbon dioxide down. Don’t wait for them to stop breathing-act before it’s too late.
- Give thyroid hormone immediately: Intravenous levothyroxine (T4) at 300-500 mcg as a loading dose. Then 50-100 mcg daily. In severe cases, especially with heart problems, add liothyronine (T3) at 10-20 mcg every 8 hours. New guidelines from 2022 show T3 reduces 30-day mortality by 15%. Don’t delay because you’re waiting for a test result.
- Warm the patient-gently: Use blankets. Turn up the room temperature. Do NOT use heating pads, warm baths, or heat lamps. Your body can’t handle sudden metabolic demands. Passive rewarming is the only safe way.
- Treat the trigger: Infection causes 30-50% of cases. Start broad-spectrum antibiotics right away. Common culprits: pneumonia, UTI, sepsis. Don’t wait for cultures. Use the DIMES checklist: Drugs, Infection, Myocardial infarction, Exposure to cold, Stroke.
- Fix electrolytes slowly: Hyponatremia (low sodium) is common. But correcting it too fast can cause brain damage. Limit sodium correction to 4-6 mmol/L in the first 24 hours.
These steps aren’t optional. They’re survival steps. A 2023 study showed patients who got full protocol care within 90 minutes had a 78% survival rate. Those who waited over 4 hours? Only 31% made it.
What Happens After the Emergency?
Once stabilized, patients need lifelong thyroid hormone replacement. Most will take levothyroxine daily. But recovery isn’t instant. It takes days to weeks for mental clarity to return. Some patients report feeling like they’re "coming out of fog" after 48 hours of treatment. Others take weeks to fully recover.
Long-term, the goal is prevention. Patients who survive myxedema coma often had been non-adherent to medication. Common reasons: forgetting doses, thinking they felt fine, or stopping meds during hospital stays. A 2022 survey found 18% of hypothyroid patients had a near-miss event-usually because of infection, hospitalization, or cold exposure.
Education is key. Tell patients: Never stop your thyroid meds without talking to your doctor. Even if you’re sick with the flu or in the hospital, your thyroid dose may need adjustment-but never skip it.

Who’s at Risk-and Why It’s Often Missed
Women over 60 are most at risk, but men aren’t immune. In fact, men are 40% more likely to be misdiagnosed because doctors don’t expect hypothyroidism in them. Younger patients get dismissed too. "You’re too young to have this." That’s a dangerous myth.
Atypical presentations are the biggest trap. Elderly patients often show "apathetic hypothyroidism"-no weight gain, no dry skin, no constipation. Just confusion, falls, or low energy. In the ER, that looks like dementia. A 2020 study found that 30% of elderly patients with myxedema coma had no classic symptoms at all.
Health disparities are real. Uninsured patients wait 35% longer for treatment and have 22% higher death rates. In rural clinics, thyroid tests aren’t always available. In developing countries, testing is rare. The Global Burden of Disease Study predicts a 20% rise in myxedema coma cases by 2030, mostly because the elderly population is growing-and many never got diagnosed in the first place.
What’s New in Treatment?
Things are changing fast. In January 2023, the FDA approved a new IV thyroid hormone called Thyrogen® with faster absorption. That means quicker recovery. Research is also moving toward point-of-care testing-devices that can check TSH and T4 levels in 15 minutes, right at the bedside. Several are in phase 3 trials with 92% accuracy.
A 2023 Lancet study found that elevated thyrotropin receptor antibodies can predict who’s likely to crash. That could help catch high-risk patients before they collapse.
Hospitals in the U.S. are required to have emergency protocols for endocrine crises. As of 2022, 87% of hospitals have formal myxedema coma guidelines. But knowing the protocol isn’t enough. Staff need to be trained to recognize the subtle signs.
Final Takeaway: Don’t Wait for the Lab
Myxedema coma is rare, but deadly. It doesn’t care if you’re young, male, or "too healthy-looking." If someone with known or suspected hypothyroidism becomes lethargic, cold, confused, or slow-breathing-act. Give thyroid hormone. Start antibiotics. Warm gently. Don’t wait. Your quick action could be the difference between life and death.
And if you or someone you know takes thyroid medication: never skip a dose. Even during illness. Even during hospital stays. Always check with your doctor before changing anything. That simple habit saves lives.










Jake Kelly
January 11, 2026 AT 07:30 AMThis is one of those posts that makes you realize how much we take basic physiology for granted. I had a grandma who went undiagnosed for years-just thought she was 'getting old.' Turns out she was slowly shutting down. Scary stuff.
Ashlee Montgomery
January 12, 2026 AT 23:23 PMThe part about passive rewarming is critical. I saw a case where a nurse used a heating blanket and the patient went into cardiac arrest. Thyroid failure isn't just low metabolism-it's a fragile balance. One wrong move and the system collapses.
neeraj maor
January 14, 2026 AT 09:22 AMLet me guess-Big Pharma pushed this protocol because levothyroxine is a cash cow. They don't want you to know about natural desiccated thyroid or iodine protocols. The real cause? Fluoride in the water. It blocks thyroid receptors. Look up the CDC’s 1999 report on fluoride and hypothyroidism. They buried it.
Ritwik Bose
January 16, 2026 AT 01:47 AMThank you for this comprehensive breakdown. 🙏 In India, many elderly patients are misdiagnosed as having dementia or depression. Access to TSH tests is still a luxury in rural clinics. This should be mandatory training for all primary care providers.
Paul Bear
January 16, 2026 AT 21:20 PMYou mentioned TSH >100 mIU/L. That’s correct, but let’s be precise: the reference range is 0.4–4.0 mIU/L. A value above 100 is not just elevated-it’s astronomically abnormal. And the 300–500 mcg IV T4 loading dose? That’s based on 2022 ATA guidelines, not anecdotal practice. Don’t confuse clinical rigor with speculation.
lisa Bajram
January 17, 2026 AT 04:40 AMI work in ER and this? This is THE checklist I print and tape to my station. Last month, a 72-year-old woman came in looking like she’d been hit by a truck-slurred, cold, barely breathing. We didn’t wait for labs. Gave T4, started abx, warmed her gently. She woke up 36 hours later and asked if we had any coffee. Best. Day. Ever. 🤘
Jaqueline santos bau
January 19, 2026 AT 00:00 AMI just found out my neighbor’s sister died from this and no one saw it coming. She was ‘just tired’ for months. Her doctor told her to ‘get more sleep.’ I’m crying right now. Why is this not on every medical show? Why isn’t everyone taught this? It’s not fair. It’s not right. It’s a tragedy waiting to happen to someone you love.
Kunal Majumder
January 20, 2026 AT 01:37 AMIn my village, people use ashwagandha and guggul for thyroid. Sometimes it helps. But when someone starts slipping into confusion? No herb fixes that. You need the real stuff. This post saved lives.
Aurora Memo
January 20, 2026 AT 19:38 PMI’m a nurse who’s seen this twice. The biggest tragedy isn’t the misdiagnosis-it’s the guilt families carry. ‘We should’ve noticed.’ You didn’t know. Now you do. That’s how change starts.
McCarthy Halverson
January 21, 2026 AT 10:18 AMT3 added in severe cases reduces mortality. That’s the key. Many docs still only give T4. Big mistake.
chandra tan
January 23, 2026 AT 00:00 AMIn India, we call this ‘slow death’-people just fade away. No one connects it to thyroid. I told my uncle to get tested after he stopped cooking and started sitting all day. Turned out his TSH was 180. He’s alive now. Thanks for the clarity.
Dwayne Dickson
January 24, 2026 AT 13:59 PMAh yes, the classic ‘it’s just depression’ misdiagnosis. How quaint. In a world where algorithms recommend antidepressants before labs, it’s no wonder this kills. The real crisis isn’t hypothyroidism-it’s the systemic devaluation of endocrine medicine.
Ted Conerly
January 25, 2026 AT 02:09 AMIf you’re on thyroid meds and get sick, don’t stop. I learned this the hard way. Missed one dose during a cold and spent three days in bed like a zombie. Docs don’t tell you this. You have to learn it the hard way.
Faith Edwards
January 26, 2026 AT 05:35 AMIt’s appalling that this isn’t standard curriculum in med school. I’m a physician, and I didn’t learn about myxedema crisis until my third year of residency. We’re training doctors to miss this. That’s not negligence-it’s malpractice by omission.
Jay Amparo
January 27, 2026 AT 10:59 AMThis post is a gift. I shared it with my entire family. My aunt is 78, takes levothyroxine, and lives alone. Now she has a printed copy taped to her fridge. I cried reading it. Not because it’s sad-but because it’s the kind of knowledge that turns helplessness into power. Thank you.