When your joints are swollen, your breathing is tight, or your skin is burning with inflammation, corticosteroids can feel like a miracle. Within days, pain fades, swelling drops, and you can breathe again. But here’s the catch: that relief comes with a price tag you might not see until months or years later.
How Corticosteroids Work - and Why They’re So Fast
Corticosteroids, like prednisone and hydrocortisone, are synthetic versions of cortisol - the stress hormone your body naturally makes. They don’t just mask pain. They shut down inflammation at the source. That’s why they work faster than anything else. While a DMARD like methotrexate takes weeks to kick in, corticosteroids often bring relief in 24 to 48 hours. For someone in a lupus flare or having a severe asthma attack, that speed is life-saving.
They’re used in all forms: pills, shots, inhalers, creams. A cortisone injection into a painful knee can give relief for weeks. A short oral course for a bad sinus infection might clear up symptoms in days. The American College of Rheumatology calls them the “fastest and most efficient way to control inflammation.” And for acute flare-ups, that’s true.
The Hidden Cost: What Happens After the Relief
But here’s what most people don’t realize: even a 5-day course of prednisone can trigger serious side effects. A 2021 study tracking 1.5 million patients found that within just 30 days of starting corticosteroids, the risk of sepsis jumped by 430%. Venous blood clots went up by 230%. Fractures increased by 90%. These aren’t rare outliers. These are measurable, documented dangers.
And it’s not just emergencies. In the U.S., nearly one in five adults gets a corticosteroid prescription each year. About half of those are for conditions where they don’t belong - like a common cold, a mild sinus infection, or even back pain. The American Academy of Family Physicians says this is a quality-of-care failure. You’re not helping. You’re risking.
Patients report side effects fast. Weight gain - often 10 to 15 pounds in under two months. Moon face. Insomnia. Blood sugar spikes that turn prediabetics into full-blown diabetics. One patient on Reddit wrote, “I started 20mg of prednisone for a lupus flare. In 10 days, I looked like I’d gained 20 pounds. I couldn’t sleep. My feet swelled. But my joints? Barely aching. I felt like a different person.”
Long-Term Use: The Silent Damage
Short-term use is risky. Long-term use is dangerous. And yet, many patients stay on corticosteroids for months - sometimes years - because their doctors don’t have better options. That’s where the real damage builds.
Every month on steroids, you lose 3% to 5% of your bone density. After six months, your risk of spinal fractures doubles. The American College of Rheumatology says anyone on more than 7.5mg of prednisone daily for over three months needs a bone scan. Yet, only 42% of primary care providers actually order them.
Eye damage is another silent threat. Cataracts develop faster. Glaucoma risk climbs. One study found 12% of long-term users developed cataracts - even after stopping the drug. And once they’re there, they don’t go away.
Then there’s adrenal suppression. Your body stops making its own cortisol because the pills are doing the job. If you stop cold turkey, your body can’t respond to stress. You could go into adrenal crisis - low blood pressure, vomiting, coma. That’s why you can’t just quit. You have to taper. Slowly. Under supervision.
Who’s Most at Risk - and Why
Older adults are hit hardest. People over 65 get corticosteroid prescriptions 2.3 times more often than those under 45. Why? Because they’re more likely to have arthritis, COPD, or other chronic conditions. But they’re also more vulnerable to bone loss, infections, and blood sugar spikes.
People in rural areas are 1.7 times more likely to get inappropriate prescriptions. Why? Fewer specialists. Less follow-up. More reliance on quick fixes.
And it’s not just patients. Doctors face pressure too. A patient comes in with a bad cough. They want something fast. Antibiotics won’t help - it’s viral. But a steroid? That might make them feel better in a day. So it gets written. Even though the evidence says: no benefit. Only risk.
What’s Being Done - And What You Can Do
Change is coming. In December 2023, the FDA approved a new drug called fosdagrocorat. It’s the first selective glucocorticoid receptor modulator - designed to fight inflammation without wrecking your metabolism. Early trials show 63% less blood sugar trouble than prednisone. It’s not a magic bullet, but it’s a step forward.
Hospitals are also waking up. Electronic health records now flag inappropriate steroid prescriptions in 87% of U.S. hospitals. Medicare Advantage plans now require pre-authorization for any course longer than 10 days. The goal? Cut down on misuse by 50% in five years.
But you don’t have to wait for policy changes. Here’s what you can do:
- If you’re prescribed corticosteroids, ask: “Is this truly necessary? Are there alternatives?”
- Never take steroids for a cold, flu, or mild bronchitis. They don’t work - and they hurt.
- Ask for the lowest dose for the shortest time possible. Five days is better than 14. Ten milligrams is better than 20.
- If you’re on it for more than two weeks, insist on a taper plan. Don’t just stop.
- Ask for bone density scans, eye exams, and blood sugar checks if you’re on it longer than three months.
- Take calcium and vitamin D daily if you’re on long-term therapy. It’s not optional - it’s protection.
The Bottom Line: A Tool, Not a Cure
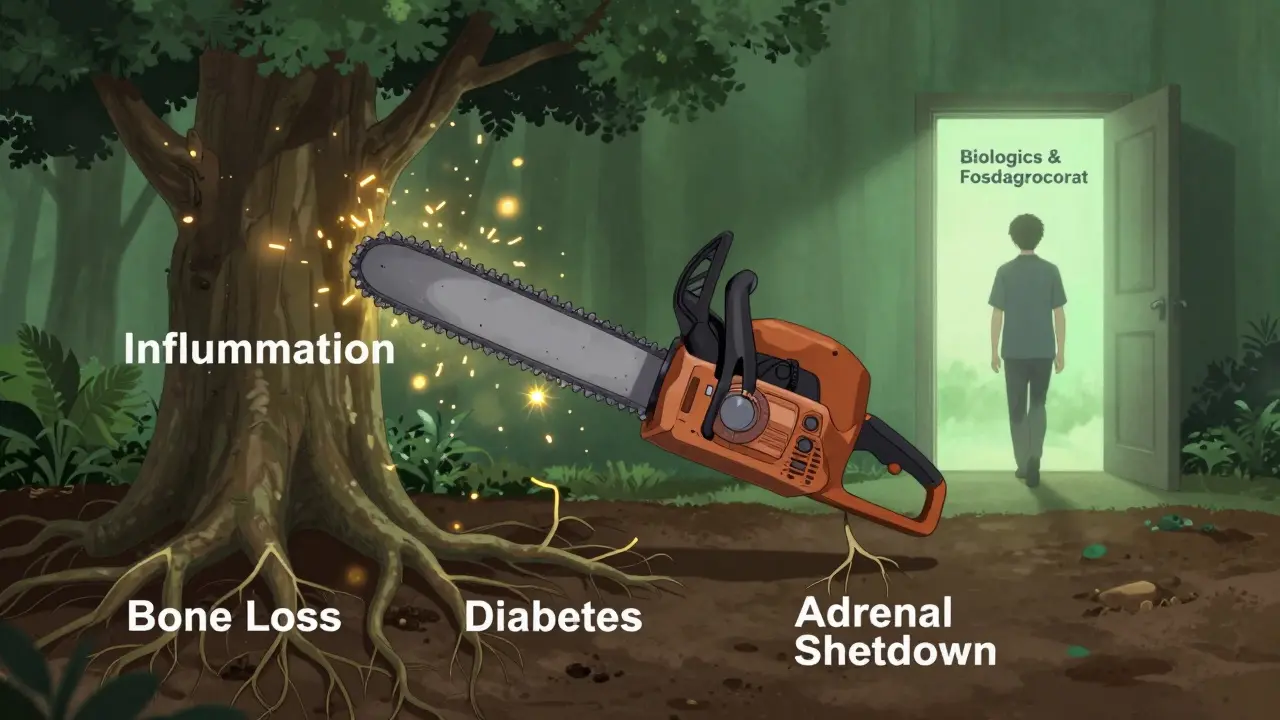
Corticosteroids are not evil. They’re powerful. Like a chainsaw - brilliant for cutting down a tree, terrible for trimming hedges. They’re not meant for daily, long-term use. They’re emergency tools.
For a severe asthma attack? They save lives. For a rheumatoid arthritis flare? They buy time until the real disease-modifying drugs kick in. For a sudden flare of lupus or vasculitis? They’re often the only thing that keeps you alive long enough to get to the next step.
But if you’re on them for months because nothing else worked - that’s a sign your treatment plan needs a rethink. Talk to a specialist. Explore biologics. Try DMARDs. Ask about new options like fosdagrocorat.
The truth? Most people don’t realize how much damage these drugs can do - until it’s too late. The relief is real. But so are the risks. The goal isn’t to avoid them entirely. It’s to use them wisely - and never, ever, casually.
Can I stop taking corticosteroids if I feel better?
No - not without talking to your doctor. Even if your symptoms are gone, your body may still be dependent on the drug. Stopping suddenly can cause adrenal crisis, which is life-threatening. You must taper off slowly under medical supervision. The length of the taper depends on how long you’ve been on the drug and your dose. A 14-day course might need a 7-day taper. A 6-month course could take months to safely reduce.
Are corticosteroid injections safer than pills?
Injections deliver the drug directly to the problem area - like a joint or tendon - so less of it enters your bloodstream. That means fewer systemic side effects. But they’re not risk-free. Repeated injections can damage cartilage and weaken tendons. One study found that more than three injections in the same joint within a year increases the risk of joint deterioration. They’re great for short-term relief, but not a long-term solution.
Do corticosteroids cause weight gain even with a healthy diet?
Yes. Corticosteroids change how your body stores fat and retains fluids. They increase appetite and shift fat to your face, neck, and abdomen - even if you eat the same amount. Weight gain isn’t about willpower. It’s biology. On average, people gain 12.4 pounds in just eight weeks on a standard dose. The good news? Most of the weight comes off after stopping, but it can take months. Managing diet and sodium intake helps, but won’t prevent it entirely.
Can corticosteroids cause diabetes?
Absolutely. Corticosteroids make your liver release more glucose and reduce your body’s sensitivity to insulin. This can trigger new-onset diabetes in people with no prior history. Studies show 7% of long-term users develop steroid-induced diabetes - and for some, it never goes away. If you’re on more than 7.5mg of prednisone daily for over three months, monthly blood sugar checks are critical. Early detection can prevent permanent damage.
Are there natural alternatives to corticosteroids?
There are no natural remedies that match the power of corticosteroids for acute inflammation. Turmeric, omega-3s, and CBD may help with mild joint pain or low-grade inflammation, but they won’t stop a lupus flare or severe asthma attack. They’re supportive, not substitutes. For chronic conditions, disease-modifying drugs like methotrexate or biologics like adalimumab are the proven alternatives. Don’t trade a proven treatment for an unproven supplement - especially when your health is at stake.
How do I know if my corticosteroid use is appropriate?
Ask yourself three things: 1) Is this for a condition with strong evidence (like rheumatoid arthritis, asthma flare, or vasculitis)? 2) Is the dose the lowest possible for the shortest time? 3) Am I being monitored for side effects (bone density, blood sugar, eye exams)? If you can’t answer yes to all three, talk to a specialist. Your primary care doctor may not have the training to manage long-term steroid use safely. Rheumatologists, pulmonologists, and immunologists do.










Nupur Vimal
December 15, 2025 AT 19:39 PMCorticosteroids are a godsend for my RA flare-ups I dont care what the stats say I lived on them for 5 years and I m still standing
Benjamin Glover
December 17, 2025 AT 02:06 AMOf course you did. You re one of those people who think science is optional if it doesn t match your anecdote. The data is clear. You re not a hero. You re a walking side effect.
John Brown
December 17, 2025 AT 05:49 AMBenjamin I get where you re coming from but Nupur isn t wrong for surviving. The system failed her by not offering alternatives sooner. That s the real issue not that she used the tool.
Michelle M
December 17, 2025 AT 09:53 AMIt s so hard to balance fear and hope when you re the one living it. I was on prednisone for 18 months after my vasculitis diagnosis. I gained 30 pounds lost bone density and nearly lost my mind. But I also lived. And now I m on biologics and slowly healing. The drug saved me. But it also broke me. I wish someone had told me that both could be true.
Lisa Davies
December 18, 2025 AT 02:04 AMThank you for sharing this 🙏 I was terrified to even ask my doctor about tapering. Hearing you say it s possible to heal after gives me so much hope.
Cassie Henriques
December 19, 2025 AT 08:12 AMPer the 2021 Lancet cohort study n=1.5M the OR for sepsis was 4.3 (95% CI 3.9-4.7) and for VTE 2.3 (1.9-2.8) - statistically significant even after adjusting for age comorbidity and indication. But the real kicker? The risk persists for 90 days post-discontinuation. Most GPs don t even track that.
Jake Sinatra
December 20, 2025 AT 07:53 AMThat s precisely why we need standardized protocols. The fact that 58% of primary care providers don t order bone scans for patients on long-term steroids is not just negligent - it s indefensible. This is preventable harm.
RONALD Randolph
December 21, 2025 AT 23:43 PMWho authorized this? Who let this happen? We re giving steroids like candy. And now people are dying from preventable infections because doctors are lazy and patients are dumb. This is a national disgrace.
Sai Nguyen
December 22, 2025 AT 11:47 AMIndia has 10x more steroid abuse than the U.S. and no one talks about it. Our doctors prescribe prednisone for fever. It s criminal.
Raj Kumar
December 24, 2025 AT 00:24 AMMy uncle got a steroid shot for his knee and now he can t walk without a cane. The doc said it was fine. He didn t warn him about tendon damage. I wish someone had told us earlier. We re not mad just confused.
Melissa Taylor
December 25, 2025 AT 11:30 AMThank you for writing this. It s not about fear. It s about awareness. I used to think steroids were magic. Now I know they re a temporary bridge. And bridges need engineers - not just a push of a button.