When your doctor suspects liver damage from fatty liver disease, alcohol, or hepatitis, they don’t always need to stick a needle in your liver to find out. In fact, most of the time, they won’t. The old gold standard-liver biopsy-is risky, painful, and often unnecessary. Today, two powerful noninvasive tools are changing how liver fibrosis is assessed: FibroScan and serum-based scores like FIB-4, APRI, and ELF. These tests give doctors real insight into how much scarring has built up in your liver, without surgery.
What Is Liver Fibrosis, and Why Does It Matter?
Liver fibrosis isn’t a disease itself-it’s the result of long-term damage. When your liver is constantly under stress from fat buildup, alcohol, viruses, or toxins, it tries to heal itself. But instead of repairing perfectly, it lays down scar tissue. Over time, this scarring builds up, stiffens the liver, and blocks its ability to function. If left unchecked, fibrosis can turn into cirrhosis, liver failure, or even liver cancer.
Right now, about 1 in 4 people worldwide have non-alcoholic fatty liver disease (NAFLD). That’s more than 1.9 billion people. Of those, roughly 1 in 5 will develop the more serious form, NASH, which carries a higher risk of fibrosis. The problem? Most people feel fine until it’s too late. That’s why noninvasive tests are so important-they catch problems early, before symptoms show up.
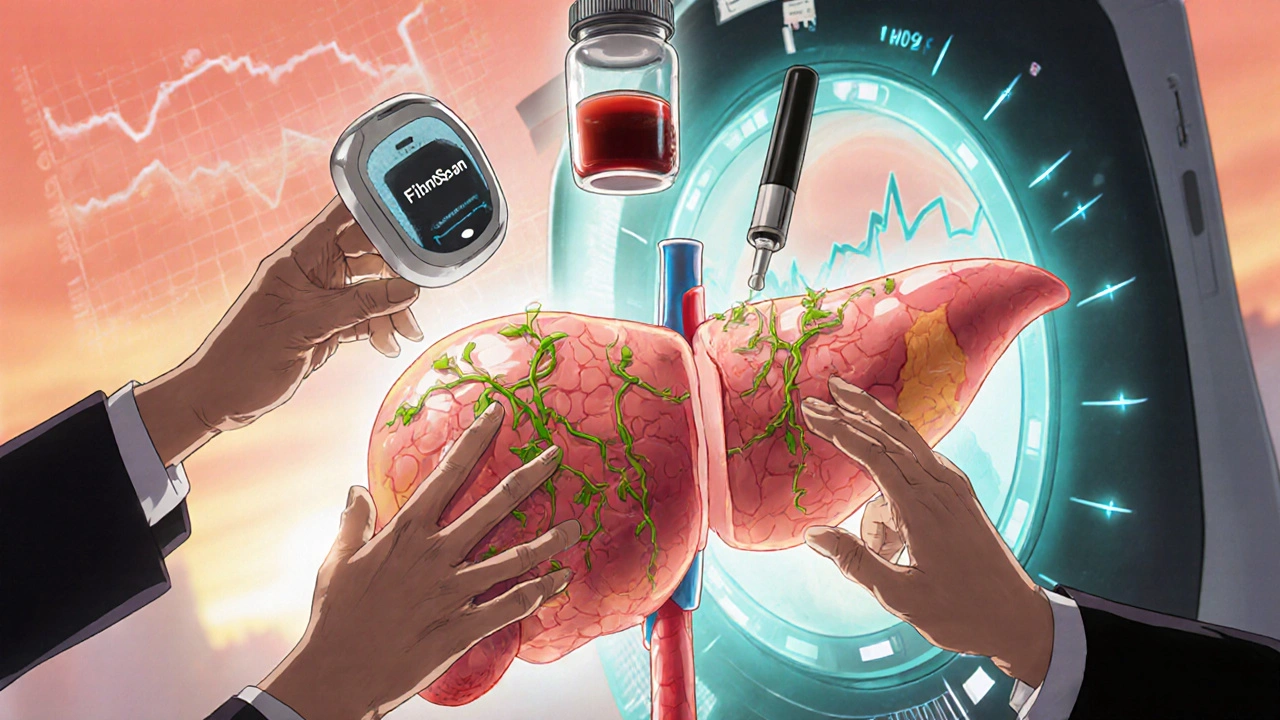
FibroScan: The Ultrasound That Measures Stiffness
FibroScan is a handheld device that looks like an ultrasound machine but works differently. Instead of imaging the liver, it sends a gentle pulse of low-frequency sound waves through your skin and into your liver. These waves travel faster through stiff, scarred tissue than through healthy, soft tissue. The machine measures how fast the waves move and converts that speed into a number: liver stiffness, measured in kilopascals (kPa).
Normal liver stiffness? Between 2 and 7 kPa. Anything above 7.1 kPa suggests early fibrosis. Above 9.5 kPa? Likely moderate fibrosis. Above 12 kPa? That’s advanced fibrosis or early cirrhosis. The device also measures fat in the liver using something called CAP (Controlled Attenuation Parameter), which gives a score from 100 to 400 dB/m. A CAP score over 260 means you have more than 33% fat in your liver-clearly indicating fatty liver disease.
FibroScan is fast. The whole test takes less than five minutes. No fasting is required, though you’re asked to avoid eating for two hours beforehand. You lie on your back, the technician places the probe on your right side, and it does its job. No needles. No sedation. No recovery time.
But FibroScan isn’t perfect. In obese patients (BMI over 28), the device sometimes can’t get a good signal. That’s why newer models like the FibroScan 630 come with an XL probe designed for larger bodies. Even then, about 1 in 10 tests fail to give reliable results. And if you’ve had a recent infection, heavy drinking, or heart failure, your liver might be inflamed-which can make stiffness readings falsely high. That’s why doctors don’t rely on FibroScan alone.
Serum Scores: Blood Tests That Predict Scarring
If FibroScan uses sound waves, serum scores use your blood. These are not fancy lab tests. They’re calculations based on routine blood work you’ve probably already had: AST, ALT, platelet count, age, and sometimes glucose levels. The most common ones are FIB-4, APRI, and ELF.
FIB-4 is the most widely used. It combines your age, AST, ALT, and platelet count. If your FIB-4 score is below 1.3, you’re very unlikely to have advanced fibrosis. If it’s above 2.67, you’re at high risk. The beauty of FIB-4? It’s free. Your doctor runs a basic blood panel, plugs the numbers into a calculator, and gets an answer. Many electronic health records do this automatically now.
APRI is simpler-just AST and platelets. A score above 2.0 suggests cirrhosis. It’s not as accurate as FIB-4, but it’s easy to use in places with limited resources.
ELF is more advanced. It measures three specific proteins linked to liver scarring: hyaluronic acid, procollagen III peptide, and tissue inhibitor of metalloproteinases. It’s more expensive than FIB-4, around $100 per test, but it’s more accurate than either FIB-4 or APRI for detecting advanced fibrosis.
Serum scores are great for screening. They’re cheap, fast, and can be done during a regular checkup. But they’re not as good at confirming advanced disease. A 2023 study found FIB-4 missed more than 80% of patients with true advanced fibrosis. That means a low score is reassuring-but a high score doesn’t always mean you have cirrhosis. It just means you need more testing.
FibroScan vs. Serum Scores: Which One Should You Trust?
Here’s the truth: neither one is perfect on its own. But together? They’re powerful.
Think of it like this: FIB-4 is your first filter. If your score is low (<1.3), you probably don’t have advanced fibrosis. No need for FibroScan or biopsy. If your score is high (>2.67), you’re at risk. That’s when FibroScan comes in. If your FibroScan result matches your FIB-4-both high-you’re likely dealing with real scarring. If they disagree? That’s when doctors get cautious.
A 2020 study showed that using FIB-4 first, then FibroScan for intermediate cases, reduced the need for liver biopsies by 70%. That’s huge. Biopsies are invasive. They carry a small risk of bleeding or infection. Avoiding them when possible is a win.
But here’s the catch: FibroScan is more accurate at detecting advanced fibrosis (F3/F4) than serum scores. One study found FibroScan correctly identified advanced fibrosis in 85% of cases, while FIB-4 only got it right in 17%. On the flip side, FIB-4 is better at ruling out disease. If your FIB-4 is low, you can be 90% sure you don’t have advanced scarring.
So who wins? Neither. They’re teammates. FIB-4 says, “You’re probably fine.” FibroScan says, “Let’s look closer.” Together, they give a clearer picture than either one alone.
Real-World Challenges: When Tests Don’t Match
Patients often come away confused. One person told me their FIB-4 said “high risk,” but their FibroScan said “mild fibrosis.” They were scheduled for a biopsy-and it turned out they had moderate scarring. Both tests were wrong, but in different ways.
This happens. FibroScan can be thrown off by fat, inflammation, or obesity. FIB-4 struggles in younger people. A 30-year-old with fatty liver might have a normal FIB-4, even if they’re developing fibrosis. That’s because FIB-4 uses age as a factor-older people naturally have higher scores. So if you’re under 35, FIB-4 loses accuracy.
Another issue? Cost. FibroScan costs $50-$150 per test. FIB-4? Less than $10. In rural clinics or underfunded hospitals, serum scores are the only practical option. But in places with access to FibroScan, skipping it can mean missing serious disease.
And then there’s the human factor. A patient with a BMI of 38 might need three attempts with the XL probe. One Reddit user said it took three visits and $200 extra just to get a usable result. That’s frustrating. It’s not the test’s fault-it’s the body’s.
What’s Next? The Future of Liver Testing
The field is moving fast. In April 2024, Echosens released FibroScan 730, which uses artificial intelligence to judge whether a test result is reliable. Early data shows it cuts technical failures by 22%. That’s a big deal.
There’s also a new serum score called FIB-5, which adds blood sugar levels to the mix. It’s especially useful for people with diabetes, who are at higher risk for aggressive liver scarring. One study showed FIB-5 was 89% accurate at spotting advanced fibrosis in diabetic NAFLD patients.
Even more promising? Combining FibroScan, FIB-4, and ELF into a single algorithm. A 2023 trial showed this three-test approach reduced unnecessary biopsies by 82% while still catching 94% of cirrhosis cases. That’s the future: not choosing one test, but using a smart sequence.
Meanwhile, MRI-based elastography (MRE) is gaining ground. It’s more accurate than FibroScan, with 95% sensitivity for early fibrosis. But it costs 10 times more and isn’t widely available. For now, it’s reserved for complex cases.
What Should You Do If You’re at Risk?
If you have fatty liver, diabetes, obesity, or a history of heavy alcohol use, ask your doctor about noninvasive testing. Don’t wait for symptoms. Most people with early fibrosis feel nothing.
Here’s what to ask for:
- “Can you calculate my FIB-4 score from my last blood work?”
- “If my FIB-4 is high, can I get a FibroScan?”
- “If we’re still unsure, should we consider ELF or an MRE?”
Don’t accept a vague answer like “We’ll watch you.” Push for numbers. If your doctor doesn’t offer these tests, ask why. Most clinics in the U.S. now have FibroScan machines. If they don’t, they can refer you to a center that does.
And if your results are conflicting? Don’t panic. Ask for a second opinion. Liver fibrosis isn’t a yes-or-no diagnosis-it’s a spectrum. The goal isn’t to label you. It’s to catch change early so you can reverse it.
Liver fibrosis can be stopped. Sometimes, even reversed. Weight loss, cutting back on alcohol, managing diabetes, and avoiding processed foods can make a huge difference. But you have to know where you stand first. That’s what these tests are for.
Can FibroScan detect fatty liver?
Yes. FibroScan measures liver fat using the Controlled Attenuation Parameter (CAP), which gives a score from 100 to 400 dB/m. A CAP score above 238 suggests at least 11% liver fat, and above 290 means 67% or more. This helps identify non-alcoholic fatty liver disease (NAFLD) without needing a biopsy.
Is FIB-4 accurate for younger people?
Not as much. FIB-4 becomes less reliable in people under 35 because it uses age as a factor. In younger patients, the accuracy drops from 85% to around 67%. For this group, doctors often rely more on FibroScan or other markers like ELF.
Why does my FibroScan result vary between tests?
Several factors can affect FibroScan results: recent meals, alcohol use, liver inflammation (like from a cold or infection), or obesity. Results can be falsely high if you ate within 3 hours or have high liver enzymes. Always follow pre-test instructions and get tested under consistent conditions for the most reliable comparison.
Can serum scores replace a liver biopsy?
For many people, yes. Guidelines from EASL and AASLD now recommend using FIB-4 and FibroScan together to rule out advanced fibrosis in most cases. Biopsies are only needed when results conflict, or when other conditions like autoimmune hepatitis are suspected. This approach avoids unnecessary procedures in up to 70% of patients.
How often should I get tested for liver fibrosis?
If you have NAFLD or NASH and your initial tests show mild fibrosis, repeat testing every 1-2 years is common. If your scores are stable and you’re making lifestyle changes, you might extend that to every 3 years. If you have advanced fibrosis or cirrhosis, your doctor will monitor you more closely, often with imaging and blood tests every 6 months.











Nicole M
November 12, 2025 AT 19:56 PMFibroScan is a game-changer, but I wish more doctors actually use it. My PCP just ordered a blood panel and said 'come back in six months.' No mention of FIB-4 or anything. I had to look this up myself after reading a study on NAFLD. It’s wild that we’re still relying on guesswork in primary care.
Shante Ajadeen
November 12, 2025 AT 22:32 PMThis is exactly the kind of info I needed. My dad has type 2 and fatty liver, and he’s been ignoring it. I’m printing this out and giving it to his doctor tomorrow. No more 'watch and wait'-we’re pushing for the FibroScan now.
Johnson Abraham
November 14, 2025 AT 14:26 PMlol so fibroscan is just a fancy ultrasound? i thought it was magic. also fiv-4? u mean fib-4? smh. why do docs make everything sound like sci-fi?
Benjamin Stöffler
November 16, 2025 AT 01:13 AMLet’s be clear: the entire non-invasive fibrosis paradigm is a statistical illusion dressed in medical jargon. FIB-4? A crude algorithm derived from population averages that collapses under the weight of individual variability. APRI? A relic from the pre-digital era. ELF? A costly luxury for the insured. And FibroScan? A device whose accuracy plummets precisely when it’s needed most-in obese, inflamed, or metabolically dysregulated patients. We’re not diagnosing fibrosis; we’re guessing based on noisy proxies. And yet, we’ve institutionalized this as standard of care. The real scandal? The biopsy, the only direct measure, is vilified as 'invasive'-as if truth itself were the problem.
Amie Wilde
November 17, 2025 AT 23:59 PMMy FibroScan was flagged as 'inconclusive' twice. Third time worked. Took three visits. No one told me it might fail. Frustrating. But worth it when they finally got a number.
Erica Cruz
November 18, 2025 AT 20:33 PMOf course this is all just a money grab. FibroScan machines cost $50k. Labs charge $100 for ELF. Meanwhile, your doctor gets paid for 'consults' and 'follow-ups.' No one’s talking about how this industry profits from turning healthy people into 'at-risk' patients. Wake up.
manish kumar
November 19, 2025 AT 05:07 AMI’ve been managing NAFLD for five years now, and I can tell you this: the real breakthrough isn’t the tech-it’s the mindset shift. For years, doctors treated fatty liver like a cosmetic issue. 'Lose weight,' they’d say. But no one told me what 'mild fibrosis' meant, or that it could be reversed. When I finally got my FIB-4 and FibroScan done together, I saw the numbers: my stiffness went from 8.2 to 6.1 over 18 months after cutting sugar and walking daily. That’s not magic. That’s biology. And it’s happening to millions who don’t even know they’re eligible for these tests. If you’re overweight, diabetic, or just feel 'off' after meals, ask for FIB-4. It’s free. If it’s high, push for FibroScan. Don’t wait for jaundice or swelling. By then, it’s too late. The liver doesn’t scream-it whispers. These tests are the only way to hear it before it’s too quiet.
Deepa Lakshminarasimhan
November 20, 2025 AT 14:16 PMWhy is this info only coming out now? I’ve been reading about liver scans since 2018. Why don’t insurance companies cover FibroScan like they do mammograms? Who’s blocking this? I’m starting to think this is all about keeping people dependent on expensive treatments later. The system doesn’t want you to fix it early-it wants you to pay for the late-stage fix.
Esperanza Decor
November 21, 2025 AT 06:40 AMI’m a nurse and I’ve seen this firsthand. Patients with diabetes and fatty liver often get told 'it’s not bad yet.' But then they come back two years later with cirrhosis. We started using FIB-4 in our clinic last year-now we catch 3x more advanced cases early. The trick? We don’t wait for the patient to ask. We run it automatically on anyone over 40 with high BMI or prediabetes. It’s simple. It’s cheap. And it saves lives. If your doctor doesn’t do this, find one who does.
dace yates
November 22, 2025 AT 16:51 PMIs there a study comparing FibroScan accuracy in people with different skin tones? I read somewhere that ultrasound penetration varies with melanin levels. Just wondering if the calibration is biased.