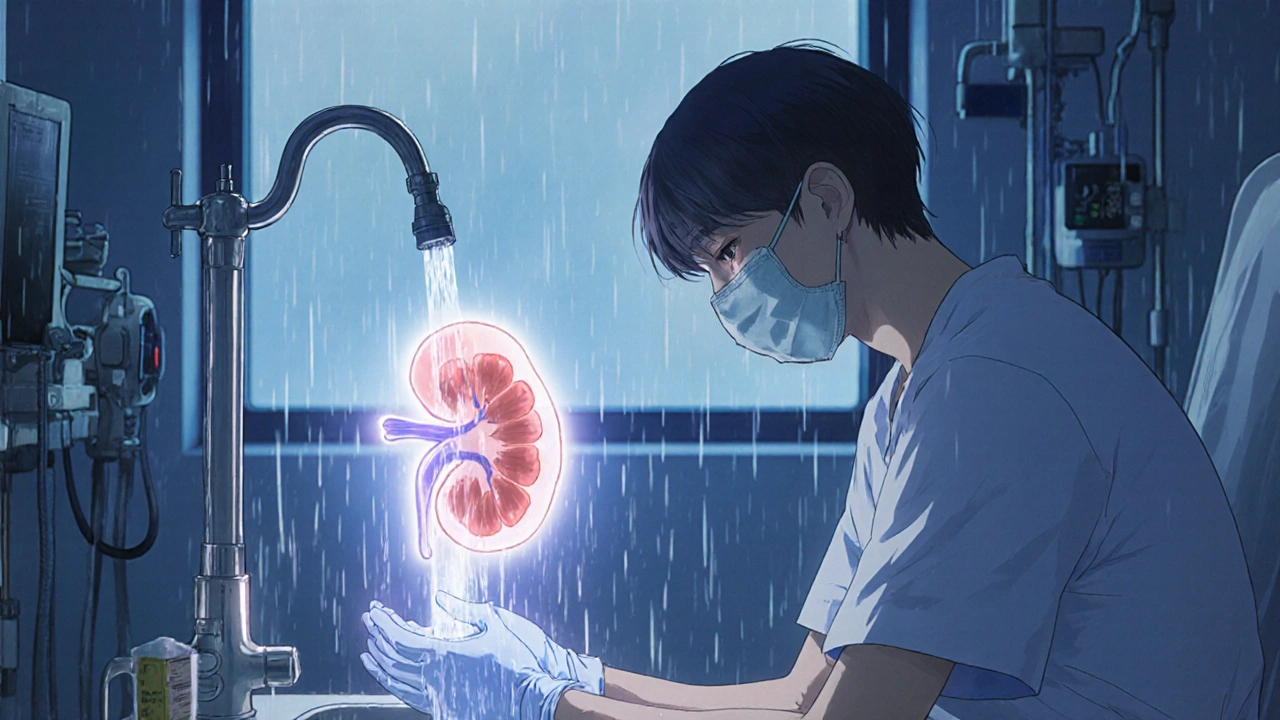
After a kidney transplant, your new organ is a gift - but your body is also fighting to keep it. The very drugs that stop rejection also leave you wide open to infections. In fact, post-transplant infections are one of the top reasons people end up back in the hospital within the first year. It’s not about being careless. It’s about understanding the risks and knowing exactly what to do - before, during, and after.
Why Infections Are So Dangerous After a Transplant
You’re not just more likely to get sick. You’re more likely to get seriously sick. Immunosuppressants like tacrolimus or mycophenolate don’t just calm your immune system - they turn it down so low that common germs can become life-threatening. A cold virus that would make you sneeze for a week could turn into pneumonia. A small cut could lead to a bloodstream infection. And because your body can’t mount a normal defense, symptoms often show up late - or not at all.
The biggest threats? Bacteria like Staphylococcus and Escherichia coli, fungi like Aspergillus, and viruses like cytomegalovirus (CMV). CMV alone increases your risk of organ rejection by 23-34%. It’s not rare. About half of all kidney transplant recipients get some form of CMV within the first year if they’re not protected.
Prevention Starts Before the Surgery
Waiting until after your transplant to think about infections is too late. The best defense is built before the knife even cuts.
First, your team will test you and your donor for viruses like CMV, Epstein-Barr, and hepatitis B. If you’re CMV-negative (R-) and your donor is CMV-positive (D+), you’re in the highest-risk group. That means you’ll likely start antiviral medicine - usually valganciclovir - right after surgery. This isn’t optional. It’s standard care.
Vaccines are next. You’ll get them before transplant if possible. Inactivated shots - like flu, pneumococcal, and hepatitis B - are safe and critical. Live vaccines like MMR or chickenpox? Absolutely not after transplant. They can cause the disease they’re meant to prevent.
And don’t forget your family. The CDC calls this "cocooning" - making sure everyone around you is up to date on their shots. If your grandkid comes over with the flu, you’re at risk. If they’ve had the flu shot? You’re safer.
Medicines That Keep You Safe After Transplant
After surgery, you’ll be on a cocktail of preventive drugs. This isn’t a one-size-fits-all list. It’s tailored to your risk.
- Antivirals: Valganciclovir for CMV, acyclovir or valacyclovir for herpes simplex - usually for 3 to 6 months. Some high-risk patients now get letermovir, a newer drug that’s easier on the kidneys and works longer.
- Antibiotics: Trimethoprim-sulfamethoxazole (Bactrim) prevents Pneumocystis jirovecii pneumonia and some bacterial infections. You’ll likely take this for at least 6 months.
- Antifungals: If you’re on high-dose steroids or had a long ICU stay, you might get fluconazole or voriconazole to block fungal infections.
These aren’t lifelong. Most stop after 3-12 months. But stopping too soon? That’s when infections spike. Around 6 months post-transplant, many patients feel fine and skip follow-ups. That’s dangerous. Infections don’t disappear - they just hide.
How to Avoid Germs in Daily Life
You can’t live in a bubble. But you can make smart choices.
Food safety is huge. No raw seafood. No soft cheeses like brie or feta unless they’re labeled "pasteurized." Don’t eat undercooked eggs or meat. Wash fruits and veggies like you’re preparing them for a baby. Listeria from deli meats or unpasteurized dairy can cause sepsis in transplant patients.
Water matters too. Avoid hot tubs. Don’t drink from garden hoses. If your tap water is from a private well, get it tested. Some areas have cryptosporidium or giardia in the water supply - parasites that cause months of diarrhea.
Animals? Yes - but carefully. Dogs and cats can be great for your mental health. But don’t clean litter boxes or bird cages. Wear gloves when gardening. Wash your hands after petting animals. Reptiles? Skip them. They carry salmonella.
Hands. Always. Wash with soap and water for 20 seconds. Use hand sanitizer when you can’t wash. Avoid crowded places during flu season. Wear a mask in airports, hospitals, or nursing homes. Even if you feel fine - you’re still a walking target for airborne viruses.
Monitoring: Catching Infections Before They Catch You
Waiting for a fever or cough is too late. You need active monitoring.
For CMV, your doctor will check your blood every 1-2 weeks for the first 3 months, then monthly. A simple PCR test finds viral DNA long before you feel sick. That’s preemptive therapy - and it saves lives.
For fungal infections, blood tests for galactomannan or beta-D-glucan help spot aspergillosis early. For bacteria, urine cultures and wound swabs are routine if you have symptoms. And if you’ve had a central line - like a PICC or port - your team will check for signs of CLABSI (central line-associated bloodstream infection). Daily chlorhexidine baths for ICU patients reduce these infections by up to 22%.
Some transplant centers now screen for multidrug-resistant organisms like MRSA or ESBL-producing bacteria. If you’ve been hospitalized before or traveled internationally, you might get a rectal swab every few weeks. It’s not fun - but it prevents outbreaks.
What Happens After 6 Months?
Many patients think they’re "out of the woods" after six months. They’re wrong.
Yes, immunosuppression often gets lighter. But your immune system is still playing catch-up. You’re still at higher risk for community-acquired infections - like respiratory viruses, urinary tract infections, and even shingles (which can flare up from dormant chickenpox virus).
And here’s the scary part: if you stopped your antiviral or antibiotic early because you "felt fine," you’re now vulnerable to late-onset CMV or Pneumocystis. These can show up 8-12 months after transplant. No warning. No fever. Just fatigue, low oxygen, and a failing graft.
That’s why follow-ups don’t stop. You need blood work, urine tests, and check-ins - even if you’re feeling great.
New Frontiers: What’s Coming Next
Science is catching up. There’s no CMV vaccine yet - but over a dozen are in clinical trials. One candidate, mRNA-based, showed promising results in 2024.
Fecal microbiota transplants (FMT) are being tested to fight drug-resistant bacteria in the gut. Instead of antibiotics that wipe out good and bad bugs, FMT rebuilds a healthy microbiome that naturally blocks harmful ones.
And researchers are starting to measure immune function directly - not just by drug levels, but by how your T-cells respond. Imagine a test that tells your doctor: "Your immune system is strong enough to skip this antiviral." That’s the future. Personalized prevention.
Bottom Line: Stay Alert, Stay Alive
Post-transplant infection prevention isn’t about fear. It’s about control. You’ve already done the hard part - getting a new kidney. Now it’s about protecting it.
Take your meds. Get your shots. Wash your hands. Avoid risky foods. Show up for your labs. Don’t ignore fatigue, low fever, or weird aches. These aren’t "just a cold." They could be the first sign of something serious.
Your transplant team is your partner. But you’re the one who lives this every day. Be smart. Be consistent. Your new kidney depends on it.
Can I get the flu shot after a kidney transplant?
Yes - but only the inactivated flu shot, never the nasal spray. The nasal spray contains live virus and is dangerous after transplant. Get the shot at least 6 months after your transplant, and make sure it’s given by your transplant clinic or primary care provider who knows your history. Family members should also get the flu shot to reduce your exposure.
Is it safe to have pets after a kidney transplant?
Yes, but with strict rules. Avoid reptiles, birds, and young animals. Don’t clean litter boxes, bird cages, or fish tanks. Wash your hands after petting dogs or cats. Keep pets up to date on vaccines and parasite control. Pets can reduce stress and improve mental health - but only if you manage the risks. Never let pets lick your face or open wounds.
Why do I need to take antivirals for so long after transplant?
Your immune system is suppressed to protect your new kidney, but that also lets viruses like CMV hide and grow. Antivirals like valganciclovir block the virus from multiplying. Stopping too early - even if you feel fine - can let CMV explode months later. Studies show that 3-6 months of prophylaxis cuts CMV infection rates by 70-80%. Skipping it increases your risk of rejection and death.
What foods should I avoid after a kidney transplant?
Avoid raw or undercooked meat, fish, and eggs. Skip soft cheeses like brie, camembert, and blue cheese unless labeled "pasteurized." Don’t eat deli meats unless reheated until steaming. Avoid unpasteurized milk, juice, or honey. Wash all produce thoroughly. Listeria and salmonella can cause severe infections in transplant patients - even from foods that are safe for healthy people.
Can I travel after a kidney transplant?
Yes - but wait at least 3-6 months and get clearance from your transplant team. Avoid areas with poor sanitation or outbreaks of diseases like dengue, malaria, or Zika. Don’t drink tap water abroad. Bring your own bottled water. Carry a letter from your doctor listing your medications. Know where the nearest transplant center is in case of emergency. Traveling is possible - but planning is non-negotiable.
What are the signs of an infection I shouldn’t ignore?
Fever over 100.4°F (38°C), even without other symptoms. Unexplained fatigue. New cough, shortness of breath, or chest pain. Pain or burning when urinating. Diarrhea lasting more than 2 days. Redness, swelling, or pus around your surgical site. Any new rash or mouth sores. Don’t wait for a high fever - transplant patients often don’t get one. If something feels "off," call your transplant team immediately.








shubham seth
November 18, 2025 AT 16:49 PMLet’s be real - this post reads like a pharmaceutical sales pitch dressed up as medical advice. Valganciclovir? Bactrim? Fluconazole? You’re not treating infection, you’re weaponizing your bone marrow. Half the time these prophylactics do more harm than the bugs they’re supposed to kill. I’ve seen patients with kidney transplants develop fungal sepsis from antifungals, and that’s not even counting the gut microbiome carnage. We’re medicating fear, not health.
kora ortiz
November 19, 2025 AT 23:50 PMThis is exactly the kind of clarity people need after transplant. No fluff, no sugarcoating - just facts that save lives. Wash your hands. Get the shot. Don’t touch that brie. These aren’t suggestions, they’re survival rules. If you skip one, you’re gambling with your new kidney. And trust me - no one wins that game. Stay sharp. Stay safe. You got this.
Jeremy Hernandez
November 21, 2025 AT 08:54 AMCMV screening? Antivirals? Please. Big Pharma’s been pushing this ‘preventive drug cascade’ for decades. Who’s really benefiting here? The hospital? The lab? The drug reps? Not the patient. I know a guy who got CMV after 4 months on valganciclovir - because the virus mutated around the drug. They just swap one toxic pill for another. The real solution? Stop suppressing the immune system entirely. Let the body fight. It’s not broken - it’s being murdered by protocol.
Tarryne Rolle
November 22, 2025 AT 14:50 PMThere’s a deeper question here: Why are we treating the body as a machine that needs constant calibration? Transplant medicine treats survival as a technical problem, not a spiritual one. You’re told to avoid pets, raw cheese, and travel - but no one asks if you’re still alive inside. Maybe the real infection isn’t CMV. Maybe it’s the loss of trust in your own body. The drugs don’t just suppress immunity - they suppress the will to live freely.
Kyle Swatt
November 24, 2025 AT 05:24 AMI’ve been on the other side of this - transplant survivor, 8 years out. The fear? It never leaves. But here’s what nobody tells you: the best medicine isn’t in the pill bottle. It’s in the quiet moments. Walking barefoot in the grass. Talking to your dog without gloves. Laughing so hard you forget to check your temperature. Yeah, you need the labs. You need the meds. But you also need to remember you’re still human. The body remembers joy - and joy is the most underrated immunomodulator out there.
Deb McLachlin
November 25, 2025 AT 23:52 PMThe clinical guidelines referenced here are consistent with current ISHLT and KDIGO recommendations. However, the omission of individualized risk stratification based on donor-recipient serostatus and HLA mismatch is notable. Additionally, while fecal microbiota transplantation is under investigation, its efficacy in transplant recipients remains unproven in randomized controlled trials. I would encourage further citation of peer-reviewed meta-analyses to strengthen the evidence base for prophylactic regimens beyond 6 months.
saurabh lamba
November 27, 2025 AT 18:41 PMbro why are we even doing this? like... you get a new kidney and now you gotta live like a germaphobe monk? no parties, no street food, no pets, no travel... what’s the point? i’d rather live 5 years happy than 20 years scared. also who the hell has time to wash hands for 20 seconds every time they touch a doorknob? 🤡
Kiran Mandavkar
November 28, 2025 AT 05:08 AMYou call this prevention? This is medical colonialism. The poor are told to wash their hands while the rich get personalized immune monitoring. The rich get mRNA vaccines in trials. The rest get Bactrim and fear. You don’t protect a kidney by locking people in sterile cages - you protect it by dismantling the system that makes them vulnerable in the first place. Poverty, food deserts, lack of access - those are the real pathogens. This post is just a Band-Aid on a bullet wound.