Infusion Reaction Emergency Guide
What symptoms are you experiencing?
When you’re on a biologic therapy-whether it’s for rheumatoid arthritis, Crohn’s disease, or cancer-getting the infusion should feel like a step toward feeling better. But for up to 40% of patients, it’s the opposite. A sudden flush, chills, chest tightness, or a drop in blood pressure can turn a routine visit into a medical emergency. These are biologic infusion reactions, and they’re more common than most people realize. The good news? With the right prep and a clear emergency plan, most of these reactions can be prevented-or safely managed if they happen.
What Exactly Are Biologic Infusion Reactions?
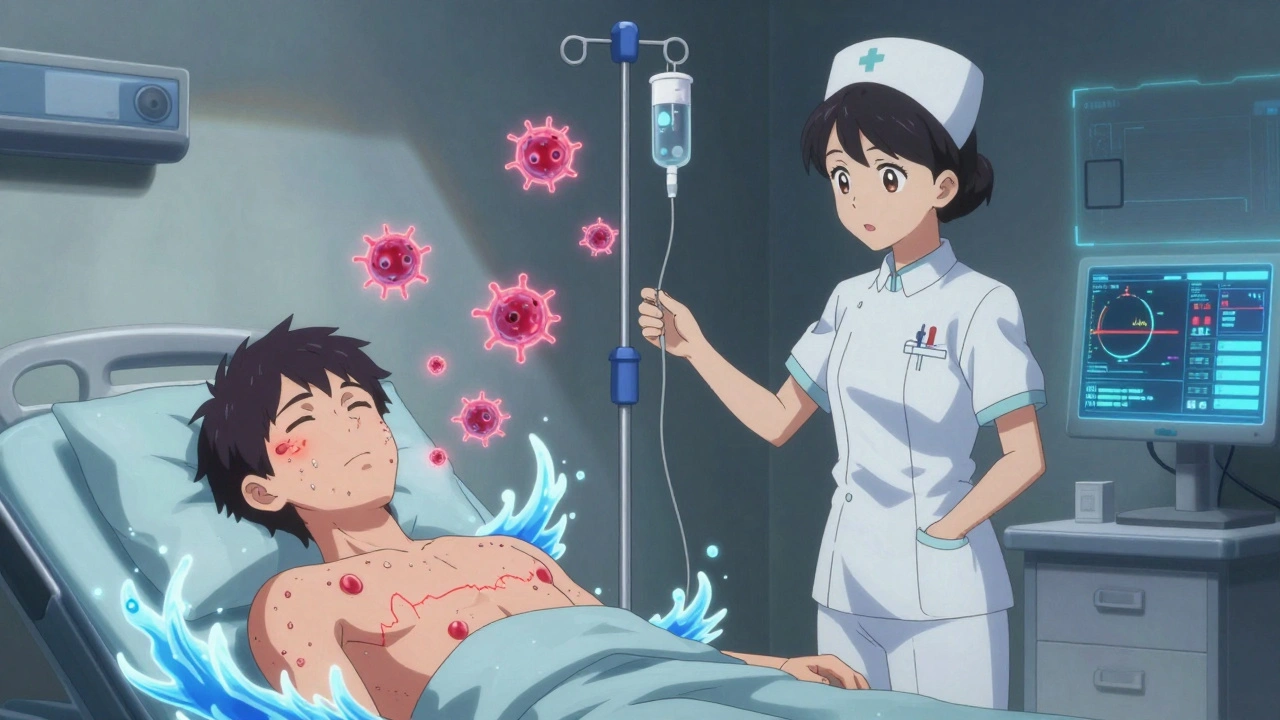
Biologic infusion reactions happen when your body reacts to medications made from living cells-like monoclonal antibodies (infliximab, rituximab, trastuzumab) or fusion proteins (etanercept). These drugs are powerful, targeting specific parts of your immune system. But because they’re foreign to your body, your immune system sometimes sees them as invaders. There are three main types:- Immediate hypersensitivity reactions (within 1-2 hours): Think hives, itching, swelling, trouble breathing. Often caused by IgE antibodies or other immune triggers.
- Cytokine release syndrome (minutes to hours): Fever, chills, low blood pressure, muscle aches. This happens when immune cells get overactivated and flood your system with inflammatory signals.
- Delayed reactions (24-72 hours later): Rash, joint pain, fever. Less urgent but still need attention.
Prevention Starts Before the Infusion
You can’t eliminate all risk, but you can cut it way down. The standard premedication protocol isn’t optional-it’s proven. Here’s what works:- Hydrocortisone 200 mg IV or methylprednisolone 125 mg IV given 30 minutes before the infusion. This reduces antibody formation by nearly half compared to no steroid.
- Diphenhydramine 50 mg IV or cetirizine 10 mg orally an hour before. Cetirizine gives the same allergy blocking as diphenhydramine but with 78% less drowsiness.
- Acetaminophen 1,000 mg orally an hour before to help with fever and chills.
What to Do If a Reaction Happens
If you start feeling anything unusual-flushing, tightness in your chest, dizziness, or a rapid heartbeat-stop the infusion immediately. Don’t wait. Don’t assume it’s just “a bad day.” Here’s the emergency checklist:- Stop the infusion.
- Position the patient flat on their back with legs elevated (Trendelenburg position) to improve blood flow to the heart and brain.
- Call for help. This isn’t something to handle alone.
- Give adrenaline (epinephrine) 0.01 mg/kg intramuscularly into the outer thigh. That’s about 0.3-0.5 mg for most adults. Repeat every 5 minutes if symptoms don’t improve.
- If breathing is hard, give nebulized adrenaline (5 mg in 3 mL saline). It opens airways in 2-5 minutes.
- For moderate reactions (Grade 2-3), give methylprednisolone 125 mg IV.
- For mild reactions, diphenhydramine 50 mg IV is fine.
Desensitization: Getting Back on Treatment
If you had a reaction but your biologic is the best option for your disease, you don’t have to quit. Desensitization is a controlled process that re-trains your immune system to tolerate the drug. The most common method is the 12-step, 3-bag protocol:- Start with 1% of the full dose, infused over 15 minutes at 0.1 mL/min.
- Gradually increase the dose in 11 more steps, doubling the rate each time.
- By step 12, you’re getting the full dose over 1-2 hours.
- Total time: 4-6 hours.
What Doesn’t Work (And Why)
Some practices sound logical but aren’t backed by evidence-or even make things riskier.- Skipping premeds to “save time”? That increases reaction rates by 2-3 times.
- Using only antihistamines without steroids? Not enough. Steroids stop the inflammatory cascade before it starts.
- Continuing after a Grade 4 reaction? Don’t. The risk of recurrence is 22%, and the next one could be fatal.
- Masking symptoms with steroids? Yes, corticosteroids can hide early warning signs like flushing or mild hypotension. One study found 18.7% of anaphylaxis cases were missed because of this.
New Tools Changing the Game
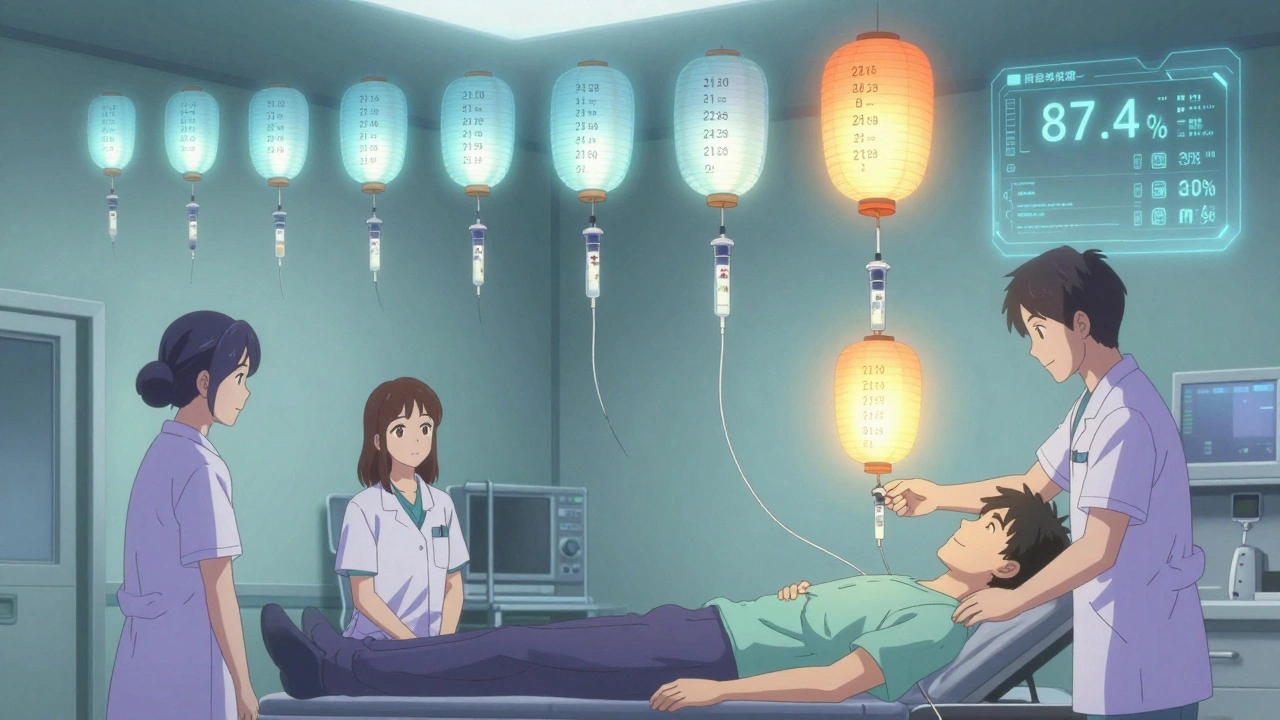
In 2024, the FDA approved the first standardized desensitization kit: BioShield®. It comes with pre-measured dilutions and step-by-step cards for 12 common biologics. No more manual mixing errors. The NIH’s DESERVE trial is testing a faster 8-step protocol with real-time IL-6 monitoring. Early results show 98.2% success. Imagine knowing your cytokine levels are spiking before you even feel sick-that’s the future. And then there’s AI. The BioReaction Score™ algorithm uses your genetic markers (like HLA-DRA*0102), baseline IL-6 levels, and even past antibiotic reactions to predict your risk with 87.4% accuracy. This isn’t sci-fi-it’s already being used in major cancer centers.Who’s Doing This Right?
In the U.S., 89% of cancer centers and 76% of rheumatology clinics have desensitization programs. But only 42% follow standardized protocols. That’s a problem. If your clinic doesn’t have a written, step-by-step plan for infusion reactions, ask for one. Your safety depends on it. The International Hypersensitivity Drug Desensitization Registry has tracked over 2,100 procedures across 47 centers. Success rate? 94.3%. That’s not luck-it’s protocol.What You Should Ask Your Provider
Before your next infusion, make sure you get clear answers to these questions:- Will I get premedication? What exactly, and when?
- What’s your emergency plan if I react?
- Do you use a standardized desensitization protocol?
- Will you check my tryptase level if I have a reaction?
- Do you track my reaction history to adjust future doses?
Bottom Line
Biologic infusion reactions aren’t rare. They’re predictable-and preventable. With proper premedication, hydration, monitoring, and a clear emergency plan, you can safely stay on the treatment that’s helping you live better. Desensitization isn’t a last resort-it’s a lifeline for those who need these drugs. And with new tools like AI risk prediction and standardized kits, the future of biologic therapy is safer than ever.Can biologic infusion reactions be fatal?
Yes, but it’s rare. Grade 4 reactions-life-threatening ones like cardiac arrest or severe airway obstruction-occur in less than 1% of infusions. Most reactions are mild or moderate. The key is early recognition and immediate action. Stopping the infusion and giving epinephrine within minutes can prevent death. The risk increases if you’ve had a prior severe reaction and continue treatment without proper desensitization.
Do all biologics cause infusion reactions?
No. Rates vary widely. Rituximab causes reactions in 30-80% of first infusions. Infliximab triggers them in 10-20%. Etanercept? Only 2-5%. TNF inhibitors like adalimumab and certolizumab are lower risk than monoclonal antibodies targeting CD20 or HER2. The drug’s structure, how it’s made, and your immune history all play a role. Always ask your provider about the specific reaction risk for your medication.
Can I take oral steroids instead of IV before my infusion?
Oral steroids like prednisone are less reliable. IV hydrocortisone or methylprednisolone ensures full, fast absorption. Oral steroids take 1-2 hours to kick in, and absorption can be inconsistent-especially if you have GI issues like Crohn’s. For maximum protection, IV is the standard. If you can’t get IV access, discuss alternatives with your provider, but know you’re accepting higher risk.
How long should I wait after a reaction before trying again?
For mild reactions (Grade 1-2), you can often resume within days with premedication and slower infusion. For moderate reactions (Grade 3), wait at least 1-2 weeks and consider desensitization. For severe reactions (Grade 4), you should not restart without a formal desensitization protocol-and even then, only under strict supervision. Never resume without a plan.
Is desensitization safe for elderly patients?
Yes, if they’re otherwise stable. Age alone isn’t a barrier. Older patients often have more comorbidities, so extra care is needed with hydration and heart monitoring. But studies show desensitization success rates in patients over 70 are just as high as in younger adults-around 90%. The key is individualized planning, not age-based exclusion.
What if I’m allergic to diphenhydramine?
There are alternatives. Cetirizine (10 mg orally) works just as well for allergy symptoms with less drowsiness. For IV use, ranitidine (though less common now) or hydroxyzine can be options. Always tell your team about any drug allergies before your infusion. They’ll adjust your premeds accordingly. Never skip premeds just because you’re allergic to one component.
Can I bring someone with me to my infusion?
Yes, and you should. Having someone with you helps monitor symptoms you might miss-like subtle changes in breathing or skin color. They can also help communicate with staff if you’re feeling unwell. Many infusion centers allow one visitor. Make sure they know what signs to watch for: flushing, swelling, trouble breathing, or sudden dizziness.
Do I need to avoid certain foods or supplements before my infusion?
There’s no strong evidence that diet affects infusion reactions. But avoid alcohol the day before-it can worsen inflammation. Some supplements like high-dose vitamin C, echinacea, or turmeric may stimulate the immune system, so talk to your provider about stopping them a few days before. Stick to your regular diet unless told otherwise.










Shubham Mathur
December 8, 2025 AT 06:02 AMMan I’ve had two of these reactions and they’re terrifying. First time I thought I was having a heart attack. The docs didn’t even have epinephrine ready. Thank god I screamed for help. Now I always ask for the full premed combo - steroids, antihistamine, and acetaminophen. And I bring my own saline bag. They don’t know what’s coming until it’s too late.
Ruth Witte
December 8, 2025 AT 15:08 PMTHIS. I just started rituximab last month and I was so scared. But I did the premeds, drank water like a maniac, and had my husband there to watch me. No reaction! 🙌 I’m so glad I didn’t skip anything. This post saved my life 💙
Delaine Kiara
December 10, 2025 AT 13:35 PMOkay but let’s be real - most clinics are just rushing through these infusions like it’s a fast food drive-thru. I had mine at a hospital where the nurse literally said ‘just tell me if you feel weird’ and then walked away to check on another patient. I had a Grade 2 reaction and they didn’t even stop the drip for 8 minutes. 8 minutes. My heart was pounding like a bass drum. I’m not even mad, I’m just… disappointed. This isn’t rocket science. Why is this so hard to get right?
And don’t even get me started on the ‘oral steroids are fine’ crowd. If you have Crohn’s, your gut’s already a mess. Oral meds? Please. Half of it’s probably just gonna sit in your colon and laugh at you. IV is non-negotiable. I’ve had both. The difference is night and day.
Also, why is no one talking about the tryptase test? I had to beg for it after my reaction. The nurse said ‘we don’t usually do that.’ Um. It’s literally in the guidelines. If you don’t test it, you don’t know if it was anaphylaxis or just a bad day. And if you don’t know that, you can’t protect yourself next time. This isn’t just paperwork - it’s your life insurance.
And desensitization? I did it for infliximab after my third reaction. Four hours. I cried. I was terrified. But I got my life back. My arthritis? Gone. My energy? Back. I’d do it again tomorrow. If your doctor won’t offer it, find someone who will. You deserve to feel better.
Also - stop telling people to ‘just relax.’ I’m not anxious. I’m traumatized. I’ve been in a hospital bed gasping for air because someone didn’t follow protocol. Don’t minimize it. Don’t say ‘it’s rare.’ It’s rare for you. It’s not rare for me.
And yes, I brought my husband. He held my hand. He told the nurse to stop. He knew the signs. You don’t have to be a doctor to save someone’s life. Just be present. And loud. If you see something, say something. Loudly.
Noah Raines
December 11, 2025 AT 00:59 AMBeen on adalimumab for 6 years. Only had one reaction - mild flush, no big deal. Did the premeds, hydrated like crazy, and slowed the drip. Done. No drama. Honestly, if you’re following the steps, this stuff is way safer than people think. Just don’t be lazy.
Katherine Rodgers
December 11, 2025 AT 01:20 AMOh sweetie. You really think IV steroids are the magic bullet? Let me guess - you also believe in flossing and eating kale. Cute. I’ve had 4 reactions. All while on full premeds. The steroids? They masked everything until my BP dropped to 60/40 and my tongue swelled like a balloon. You think you’re safe? You’re just delaying the inevitable. This whole system is a scam. Biologics are expensive, flashy, and frankly, overhyped. Your immune system isn’t broken - it’s trying to protect you. Stop poisoning it with lab-made antibodies and go try a real doctor.
Sarah Gray
December 12, 2025 AT 13:56 PMWhile the clinical data presented is statistically robust, one must critically interrogate the epistemological underpinnings of the so-called ‘standardized protocol.’ The very notion of protocolization presupposes a homogenized patient population - a fallacy, given the ontological plurality of immune response phenotypes. Furthermore, the uncritical adoption of BioShield® as a panacea reflects a technocratic epistemic hegemony that marginalizes patient autonomy and embodied knowledge. One wonders: if the algorithm predicts risk with 87.4% accuracy, what of the remaining 12.6%? Are they merely statistical noise - or are they the silenced voices of those whose bodies refuse to conform to the algorithm’s tyranny?
Brianna Black
December 12, 2025 AT 20:41 PMAs a rheumatology nurse in Chicago, I’ve seen it all. I’ve watched patients cry because they were scared to come back after a reaction. I’ve held their hands while they got their first desensitization dose. I’ve watched a 78-year-old woman walk out of here after her 12-step protocol - smiling, holding her granddaughter’s hand. This isn’t just medicine. It’s dignity. If your clinic doesn’t have a written plan, ask for it. If they say ‘we’ve never had a problem,’ tell them they’re just lucky. Luck isn’t a protocol. And your life isn’t a gamble.
And yes - I’ve seen patients skip premeds because they were ‘in a rush.’ Guess what? They ended up in the ICU. Not because they were weak. Because they were trusting the wrong system. Don’t be that person. Ask. Demand. Be loud. You’re not being difficult. You’re being smart.
ian septian
December 13, 2025 AT 07:35 AMPre-meds. Hydration. Stop the drip. Epinephrine on deck. That’s it. No magic. Just discipline.
Arun Kumar Raut
December 15, 2025 AT 03:50 AMI’m from India and we don’t have fancy kits or AI here. But we do have common sense. If someone feels bad - stop. Give water. Call for help. Use what you have. I’ve seen nurses use plain saline and a watch to manage reactions. It’s not about the tools. It’s about paying attention. Your life matters more than the clock.
Evelyn Pastrana
December 15, 2025 AT 06:58 AMWow. So you’re saying if I’m allergic to diphenhydramine, I should just… not get treated? That’s so helpful. Thanks for the life advice, doctor. 😏 I’m sure the 100 people who’ve had reactions on cetirizine are just lying about it. /s
precious amzy
December 16, 2025 AT 23:46 PMOne cannot help but observe the metaphysical paradox inherent in the desensitization paradigm: if the immune system is being ‘retrained’ to tolerate a foreign entity, then by what ontological authority is the foreign entity deemed ‘therapeutic’? Is not the body’s rejection a form of epistemic truth? To override it is not healing - it is epistemic violence. The algorithm may predict, but it cannot comprehend suffering. And suffering - real suffering - does not conform to statistics.
Carina M
December 17, 2025 AT 09:11 AMIt is deeply concerning that the medical establishment continues to prioritize procedural compliance over the intrinsic dignity of the patient’s biological autonomy. The normalization of pharmacological desensitization - a process predicated on the suppression of innate physiological defense mechanisms - constitutes a form of therapeutic coercion. One must question whether the preservation of life, in this context, is truly the objective - or merely the maintenance of profit-driven treatment paradigms. The patient is not a data point. The immune system is not a software bug to be patched.
Stacy Tolbert
December 18, 2025 AT 18:57 PMI just got back from my infusion. I had a reaction last time. I cried. I screamed. I felt like I was dying. They did everything right this time - premeds, slow drip, my mom holding my hand. I didn’t even feel anything. I just sat there, breathing. And for the first time in months… I didn’t feel like a patient. I felt like me. Thank you for writing this. I needed to know I’m not alone.
George Taylor
December 19, 2025 AT 05:32 AMWow. So much info. I’m just gonna… sit here. And think. About nothing. Because I’m tired. And I don’t want to feel anything anymore. Can I just… not do this anymore?