Pregnancy Medication Risk Checker
Check medication safety by trimester. Based on current medical evidence, this tool provides information about risks and alternatives for common medications during pregnancy.
Enter a medication and select a trimester to see safety information.
When you’re pregnant, taking even a simple pain reliever can feel like walking a tightrope. You need relief - maybe from headaches, nausea, or anxiety - but you’re terrified of hurting your baby. The truth is, not all medications are dangerous during pregnancy, but when you take them matters just as much as what you take. The first, second, and third trimesters aren’t just time markers - they’re windows of vulnerability, each with its own set of risks and safe options.
First Trimester: The Critical Window for Birth Defects
The first 12 weeks of pregnancy are when your baby’s organs are forming. That’s why this is the most sensitive time for medication exposure. From day 21 to day 55 after fertilization, your baby’s heart, brain, limbs, and face are all being built - and certain drugs can interfere in very specific ways.
Take isotretinoin, the acne medication sold as Accutane. If taken during this window, it raises the risk of severe brain and heart defects by 50 times compared to the general population. That’s why the FDA requires the iPLEDGE program - two negative pregnancy tests before you start, monthly tests while you’re on it, and one full month after stopping. Since the program began, pregnancy rates among users dropped from nearly 5 per 100 women per year to less than 1.
Not all risks are this extreme. Ondansetron, used for severe nausea, has been linked to a small increase in heart defects - but only if taken before week 10. After that, the risk disappears. Meanwhile, doxylamine and pyridoxine (Diclegis), a common treatment for morning sickness, shows no increased risk of birth defects at any point in pregnancy.
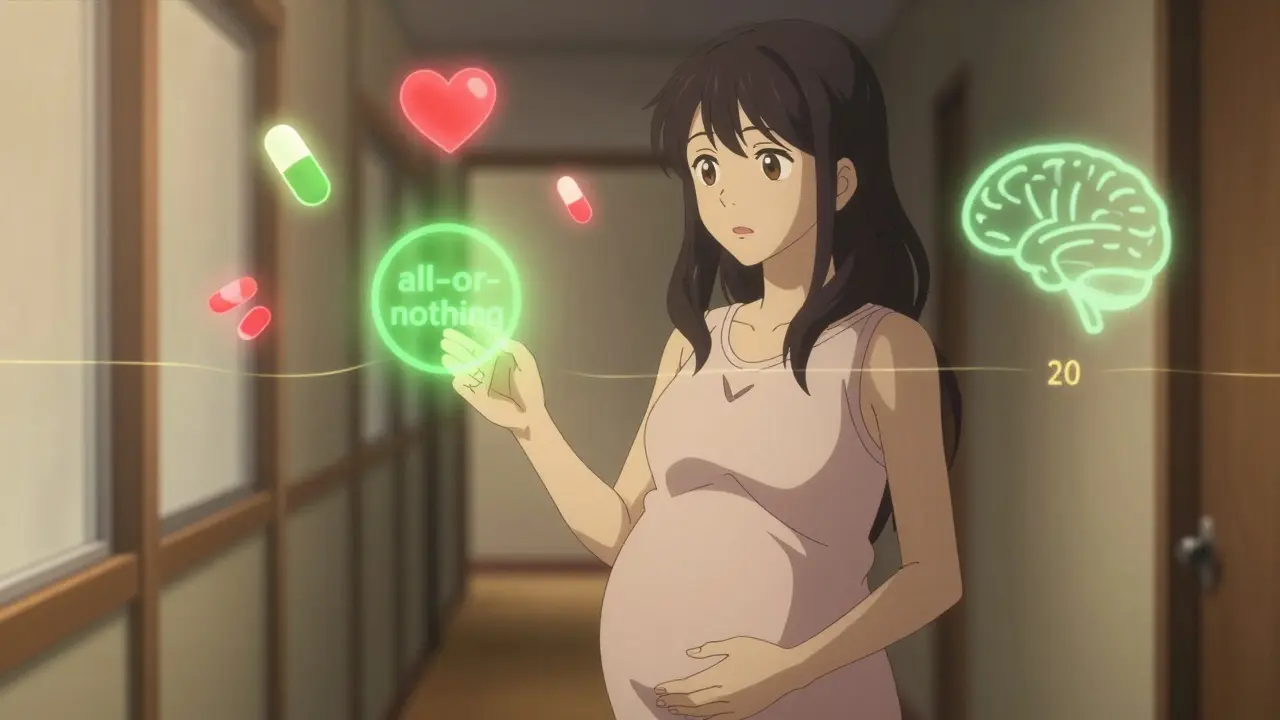
Here’s the key: if you’re taking medication before you know you’re pregnant, don’t panic. Before day 20 after fertilization, most drugs follow an “all-or-nothing” rule. Either they cause a miscarriage, or they don’t affect the baby at all. That’s why many early exposures turn out to be harmless.
Second Trimester: Shifting from Structure to Function
By week 13, your baby’s major organs are formed. The risk of major structural birth defects drops sharply. But that doesn’t mean medications are safe to use freely. Now, the concern shifts to how drugs affect your baby’s growing brain, lungs, and kidneys.
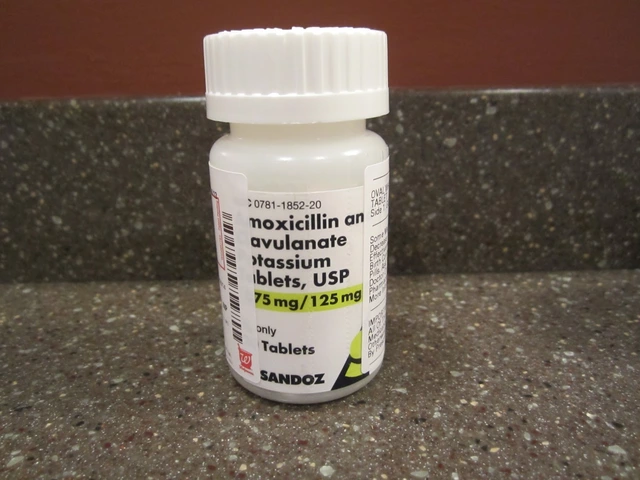
ACE inhibitors - common blood pressure meds like lisinopril - are fine in the first trimester but become dangerous after week 8. After week 12, they can cause kidney failure, low amniotic fluid, and even skull deformities. That’s why doctors switch you to labetalol or methyldopa if you’re hypertensive. These drugs have been studied across more than 12,000 pregnancies and show no increased risk of birth defects at any stage.
Antidepressants also change their risk profile. Sertraline (Zoloft) is considered the safest SSRI in the first trimester - studies of over 850,000 pregnancies show no increased risk of heart defects or other major malformations. But if you take it in the second trimester, the main concern isn’t birth defects - it’s your baby’s developing nervous system. Some studies suggest a possible link to subtle changes in motor development, though the evidence is still unclear.
NSAIDs like ibuprofen and naproxen are generally okay until week 20. After that, they can cause the ductus arteriosus - a vital blood vessel in the fetal heart - to close too early. That can lead to high blood pressure in the baby’s lungs and heart failure. ACOG recommends avoiding NSAIDs after week 20 unless under strict medical supervision.
Third Trimester: The Newborn’s First Days
In the last 12 weeks, your baby isn’t growing new organs - they’re getting ready for life outside the womb. That’s why medication risks now focus on withdrawal, breathing problems, and temporary physiological changes.
SSRIs like paroxetine (Paxil) and fluoxetine (Prozac) are the biggest concern here. About 30% of babies exposed to paroxetine in the third trimester develop neonatal adaptation syndrome - jitteriness, feeding trouble, breathing issues, and irritability. These symptoms usually resolve within days or weeks, but they can mean a longer hospital stay.
That’s why guidelines now recommend tapering SSRIs slowly in the third trimester. If you’ve been on sertraline at 100mg daily, your doctor might suggest cutting to 75mg at 34 weeks, then 50mg at 36 weeks. Abruptly stopping can trigger a relapse in your depression, which is just as risky for your baby as the medication itself.
Other common drugs like acetaminophen (Tylenol) are still considered first-line for pain and fever throughout pregnancy. But even this “safe” drug has caveats. Long-term use - over 3,500mg a day for more than two weeks - has been linked in some studies to possible behavioral issues later in childhood. Stick to the lowest dose for the shortest time.
What You Should Do - Step by Step
Knowing the risks isn’t enough. You need a plan. Here’s how to navigate medication use safely during pregnancy:
- Get your dates right. Don’t rely on your last period. An ultrasound before week 10 gives you the most accurate gestational age. Misdating leads to unnecessary panic - and sometimes, unnecessary terminations.
- Review every medication. This includes prescriptions, over-the-counter drugs, supplements, and herbal remedies. Even “natural” products like black cohosh or dong quai can be dangerous.
- Use trusted resources. The CDC’s Treating for Two tool, MotherToBaby (1-866-626-6847), and the TERIS database are backed by science. Avoid Reddit threads, Instagram posts, or Facebook groups with conflicting advice.
- Work with a team. Your OB-GYN, pharmacist, and mental health provider should all be on the same page. Only 31% of providers feel confident interpreting trimester-specific data - don’t assume they know everything.
- Don’t stop cold turkey. If you’re on a medication for anxiety, epilepsy, or high blood pressure, stopping suddenly can be more dangerous than continuing it. Always talk to your doctor first.
Common Myths vs. Science
Let’s clear up some misinformation:
- Myth: All antidepressants cause birth defects. Fact: Sertraline and citalopram show no significant increase in major malformations. Paroxetine carries a small risk - but only in early pregnancy.
- Myth: You can’t take any allergy meds while pregnant. Fact: Loratadine (Claritin) and cetirizine (Zyrtec) are Category B, meaning no proven risk in human studies. Diphenhydramine (Benadryl) is also safe in moderation.
- Myth: Acetaminophen is completely risk-free. Fact: It’s still the safest option, but long-term, high-dose use may carry subtle risks. Use it wisely.
- Myth: If you took a drug before knowing you were pregnant, your baby is doomed. Fact: Before day 20, most exposures are “all-or-nothing.” If you’re still pregnant, your baby is likely fine.
What’s Changing in 2026
The way we assess medication safety during pregnancy is evolving. In 2023, the NIH launched a $4.7 million project to build a personalized risk calculator that factors in your genetics, exact gestational age, and how your body processes drugs. By 2028, we may have individualized recommendations - not just “avoid this in the first trimester,” but “you can safely take this at 12 weeks and 3 days because of your CYP2D6 gene variant.”
The FDA is also pushing for real-time reporting of pregnancy-related side effects in electronic health records. Right now, only 27% of drug labels include precise trimester-specific risk data. That’s changing fast.
For now, the best tools you have are accurate dating, trusted sources, and open communication with your care team. You don’t need to be perfect. You just need to be informed.
Can I take ibuprofen during pregnancy?
Avoid ibuprofen after week 20. Before that, it’s generally safe for short-term use, like for a headache or muscle strain. After week 20, it can cause the baby’s heart vessel (ductus arteriosus) to close too early, leading to high lung pressure. After week 32, the risk of low amniotic fluid also increases. Acetaminophen is the safer pain reliever throughout pregnancy.
Is it safe to take Zoloft while pregnant?
Yes, sertraline (Zoloft) is considered one of the safest SSRIs during pregnancy. Large studies of over 850,000 pregnancies show no increased risk of major birth defects. In the third trimester, it may cause mild newborn symptoms like jitteriness or feeding trouble in about 2-3% of cases - far less than with paroxetine. Never stop abruptly. Work with your doctor to adjust your dose if needed.
What should I do if I took a risky medication before knowing I was pregnant?
Don’t panic. If the exposure happened before day 20 after fertilization, the drug likely had no effect or caused a miscarriage - if it was going to, it already did. After day 20, contact MotherToBaby (1-866-626-6847) or your OB-GYN. They can review the exact timing, dosage, and medication to give you a risk estimate. Most exposures turn out to be low-risk. Ultrasound dating can help clarify whether you’re at risk.
Are herbal supplements safe during pregnancy?
Most haven’t been studied enough to be considered safe. Herbs like black cohosh, blue cohosh, and pennyroyal can trigger contractions or harm the baby. Even ginger - often used for nausea - should be limited to under 1,000mg per day. Always tell your provider about every supplement you’re taking. Just because it’s “natural” doesn’t mean it’s safe.
How do I know if my doctor is giving me good advice about meds in pregnancy?
Ask them: “Is this based on human pregnancy data?” and “Do you know the exact risk by trimester?” If they rely on old letter categories (A, B, C, D, X) or say “I’ve never seen a problem,” that’s not enough. Look for providers who use tools like Micromedex, Lexicomp, or refer you to MotherToBaby. If they dismiss your concerns or say “just don’t take anything,” that’s not care - that’s avoidance.
Next Steps for Safer Medication Use
If you’re planning a pregnancy, review your meds with your doctor now. If you’re already pregnant, schedule a med review with your OB-GYN or a maternal-fetal medicine specialist. Bring a list of everything you take - including vitamins, teas, and topical creams.
Use the CDC’s Treating for Two tool to explore safe options. Call MotherToBaby for free, confidential advice - they’re specialists in pregnancy and medication safety. And if you’re feeling overwhelmed, you’re not alone. Nearly 70% of pregnant people take at least one medication. The goal isn’t zero risk - it’s smart, informed choices.









Ian Long
January 10, 2026 AT 12:01 PMMan, I took ibuprofen for a week before I knew I was pregnant. Thought I was toast. Turned out my kid’s 7 now and runs faster than me. Don’t let fear run your life - just talk to your doc and move on.
Patty Walters
January 10, 2026 AT 12:24 PMi’ve been on zoloft since before i got preggo and i was terrified. my ob-gyn referred me to mothertobaby and they said sertraline is basically the gold standard. my baby’s 4 months old and hitting all milestones. you’re not alone.
ps: don’t trust reddit threads. i almost quit my med because of one.
Phil Kemling
January 10, 2026 AT 13:29 PMIt’s fascinating how medicine treats pregnancy as a monolithic state - one size fits all. But biology isn’t a spreadsheet. Every woman’s metabolism, every fetus’s gene expression, every drug’s half-life - it’s all a dynamic system. We reduce risk to trimesters because it’s convenient, not because it’s complete.
The real question isn’t ‘what drug to take’ - it’s ‘how do we stop treating pregnant bodies like error-prone machines?’ We need personalized pharmacokinetics, not blanket warnings. The NIH’s 2026 project? That’s the first real step toward dignity in prenatal care.
tali murah
January 12, 2026 AT 09:59 AMOh wow. So now we’re supposed to trust a 4.7 million dollar NIH project that won’t even be ready until 2028? Meanwhile, women are being told to ‘just take Tylenol’ like it’s a vitamin.
Let me guess - the same people who told you ‘it’s fine to drink in the first trimester’ in 1998 are now writing these guidelines.
And don’t even get me started on ‘natural’ supplements. If your grandma used it, it’s not safe - it’s just old. Stop romanticizing herbalism. It’s not a yoga pose. It’s pharmacology with a side of pseudoscience.
Jenci Spradlin
January 13, 2026 AT 09:44 AMjust wanted to say - if you took accutane before you knew you were preggo, don’t freak out. i did. my kid’s 5 and has no issues. the ‘all or nothing’ thing is real.
but yeah, avoid ibuprofen after 20 wks. my cousin’s baby had low fluid bc she took naproxen at 30 wks. total nightmare.
and pls stop taking those ‘pregnancy tea’ blends. one of my friends had contractions from blue cohosh. true story.
Heather Wilson
January 15, 2026 AT 05:09 AMIt’s alarming how casually this post dismisses the long-term neurodevelopmental risks of SSRI exposure in utero. The studies cited are observational, not causal, yet they’re presented as gospel.
And let’s not forget: the FDA’s labeling system was dismantled precisely because it was too simplistic - but replacing it with vague trimester-based advice is not an improvement. It’s a placebo.
Where’s the data on epigenetic changes? On transgenerational effects? On the cumulative impact of polypharmacy?
Someone needs to stop treating pregnancy like a clinical trial and start treating it like the sacred, complex biological process it is. Instead, we get bullet points and cheerleading.
Micheal Murdoch
January 15, 2026 AT 14:10 PMI’ve been a doula for 12 years. I’ve held hands through panic over Zoloft, through guilt over a single Advil, through the shame of taking something ‘not natural.’
Here’s what I know: the most dangerous thing in pregnancy isn’t the medication - it’s the isolation. The silence. The fear that if you speak up, you’ll be judged.
If you’re reading this and you’re scared - you’re not failing. You’re trying. And you deserve a care team that meets you there, not one that hands you a pamphlet and says ‘just be careful.’
Call MotherToBaby. They don’t judge. They don’t scare you. They just give you the facts - and then they let you decide. That’s what real care looks like.
Chris Kauwe
January 16, 2026 AT 00:17 AMLet’s be real - this whole ‘trimester-specific’ framework is just corporate medicine’s way of offloading liability. They don’t want to admit that we still don’t know enough. So they slap on a calendar and call it science.
Meanwhile, the real issue is that 70% of pregnant women are on meds because our healthcare system doesn’t support mental health or chronic disease management outside of pregnancy.
Stop blaming the drugs. Start fixing the system. Until then, we’re just rearranging deck chairs on the Titanic - with extra emojis.
RAJAT KD
January 16, 2026 AT 20:09 PMAcetaminophen over 3,500mg/day for two weeks? That’s 10 pills a day. Who’s taking that?
If you’re on that much, you have a serious issue - and no pill is going to fix it. See a doctor. Don’t just Google and panic.
Pooja Kumari
January 17, 2026 AT 02:30 AMI took Zoloft the whole time and now I feel like a monster because my baby cries so much. Everyone says it’s fine, but I know it’s my fault. I saw a study that said SSRIs might affect serotonin levels in the brain long-term. What if he never sleeps right? What if he’s anxious? What if I ruined him?
I didn’t want to take it. I cried every time I swallowed one. But I was so depressed I couldn’t get out of bed. My husband said ‘just take it’ - but now I can’t look at him without feeling like I betrayed us.
I just need someone to say it’s okay to feel this way. Not ‘you’re fine’ - just ‘I see you.’
Jacob Paterson
January 17, 2026 AT 04:34 AMOh wow. So the solution to complex prenatal pharmacology is… calling a hotline? And trusting a doctor who ‘uses Lexicomp’?
That’s it? That’s the pinnacle of 2025 maternal care?
Meanwhile, in China, they’ve got AI-driven fetal drug metabolism models. In Sweden, they track every medication exposure through national registries. And here? We’re handing out pamphlets and praying.
It’s not ‘informed choice’ - it’s informed despair.