When a life-saving medication disappears from the pharmacy shelf, patients don’t just lose a pill-they lose control, trust, and peace of mind. A drug shortage isn’t just a supply chain problem. It’s a communication crisis. And healthcare providers are on the front lines of managing it.
In 2023, nearly 300 drugs were in short supply across the U.S., from heart medications to cancer treatments. These aren’t rare glitches. They’re systemic failures that hit patients hardest when they’re most vulnerable. Yet too often, patients find out about the shortage when they show up to refill their prescription-and the pharmacist says, "It’s out of stock. We’ll call you."
That’s not enough. Patients need more than a callback. They need clarity, empathy, and a plan. And that’s where provider responsibility begins.
What Providers Are Required to Do
It’s not optional. Federal rules and professional standards now demand clear, timely communication during drug shortages. The FDA’s 2012 Safety and Innovation Act requires manufacturers to report potential shortages six months in advance. But that’s just the start. Providers must turn that data into action.
By January 2025, the Joint Commission will require all accredited facilities to have structured, empathetic communication protocols in place for drug shortages. Failure to comply could mean losing accreditation. That’s not a threat-it’s a reality.
Providers must do four things:
- Notify patients before they ask
- Explain why the drug is unavailable
- Offer a safe, evidence-based alternative
- Give a realistic timeline for when the original drug might return
Doing less isn’t negligence-it’s a breach of trust. Studies show that 73% of patients lose confidence in their provider if they hear about a shortage from the pharmacy first. That’s not just bad customer service. It’s a risk to health outcomes.
How to Communicate Clearly-No Jargon Allowed
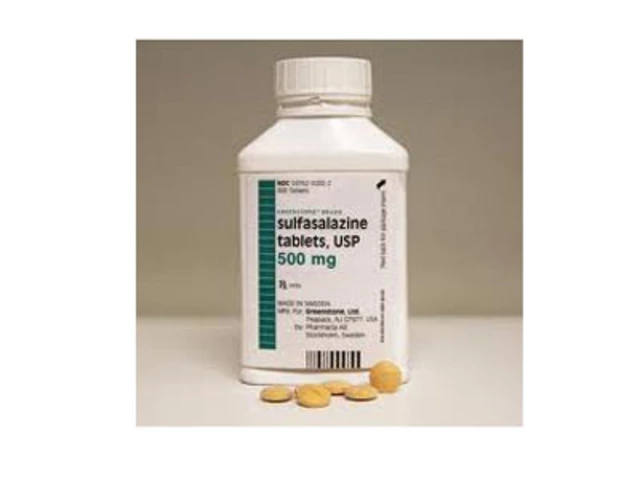
Patients aren’t pharmacists. They don’t know what "generic imipramine 75 mg capsule" means. And they shouldn’t have to.
The CDC’s Health Literacy Universal Precautions Toolkit says it plainly: all shortage communication must be written or spoken at a 6th- to 8th-grade reading level. That means no Latin names, no abbreviations, no passive voice.
Instead of saying: "We’re experiencing a supply disruption of the branded formulation of metoprolol succinate ER, which has led to substitution with the immediate-release generic." Say this: "Your heart medication, Toprol XL, is currently hard to find. We’re switching you to a different pill that works the same way but is easier to get right now. It’s called metoprolol tartrate. You’ll take it twice a day instead of once. Here’s what you need to know."
And don’t just tell them. Ask them to repeat it back. This is called the "teach-back" method. It’s not extra work-it’s safety. If a patient can’t explain how to take the new drug, they’re at risk of taking it wrong. And that’s how errors happen.
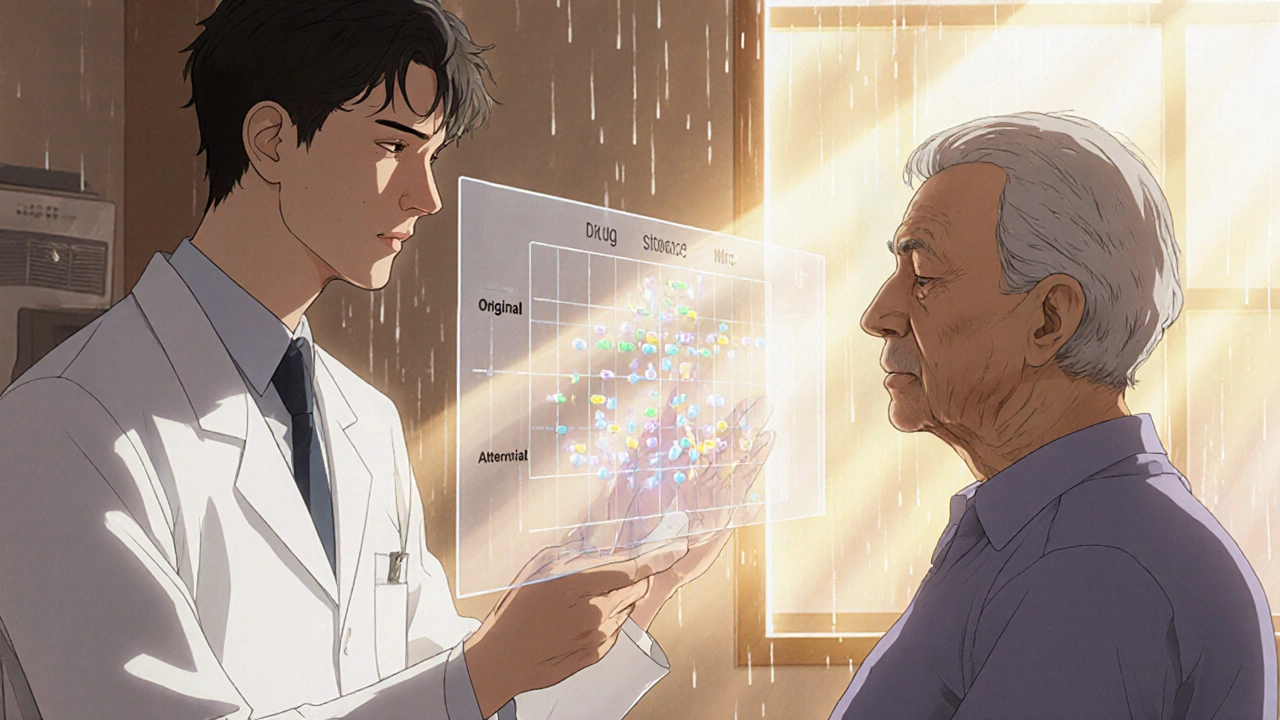
Alternatives Aren’t Just Substitutes-They’re Solutions
When a drug is out, providers often hand over a different pill and say, "This will work fine." But patients aren’t fooled. They want to know: Why is this better? Is it safe? Will it hurt?
Research shows that 78% of patients will accept a switch if they understand why. But only 32% actually get that explanation.
Here’s what works:
- "This alternative has been tested in 12 clinical trials and works just as well for your condition."
- "The side effects are similar, but you might feel a little more tired at first. That usually fades in a week."
- "We’ve given this to over 200 patients like you. 85% stayed on it without problems."
Visual aids help too. A simple chart comparing the old and new drug-dosage, frequency, side effects-cuts confusion in half. Some clinics now print these and hand them out. Others send them by email. Either way, it’s worth the five minutes it takes.
When Time Is Short, Structure Is Key
Most primary care visits last 15 minutes. That’s not enough to explain a shortage, answer questions, and reassure a scared patient. But structure makes it possible.
Take the "Chunk, Check, Change" method:
- Chunk: Give one piece of information at a time. "Your medication is out of stock."
- Check: Ask, "Can you tell me in your own words what we just talked about?"
- Change: If they’re confused, rephrase it. Don’t repeat the same words. Use a different example.
This cuts communication time by 40% and doubles patient understanding. Kaiser Permanente integrated this into their EHR system. Now, when a shortage alert pops up, the provider clicks a button and a pre-written script appears-customized to the patient’s drug and condition. It takes 90 seconds.
Rural and Non-English Patients Are Falling Through the Cracks
Not all patients get the same level of care. In rural areas, 68% of providers say they don’t get real-time updates on drug availability. That means patients in small towns are often the last to know-and the most likely to go without.
For non-English speakers, the problem is worse. Studies show they’re 3.2 times more likely to misunderstand shortage information. Translating a pamphlet isn’t enough. You need trained interpreters who understand medical terms and can explain alternatives in context.
Some clinics now use video interpreters during appointments. Others partner with community health workers who speak the patient’s language and know their cultural beliefs about medicine. These aren’t luxury services-they’re necessities.
What Happens When Communication Fails
Patients don’t just get frustrated. They stop taking their meds.
One patient on Reddit wrote: "My doctor just handed me a different pill. No explanation. I thought it was a mistake. I didn’t take it for two weeks. I ended up in the ER."
That’s not an outlier. A 2023 study found that 18% of patients stopped their medication during a shortage because they weren’t given a clear plan. That’s 1 in 5 people risking a heart attack, seizure, or worse.
And it’s not just patients. Pharmacists are overwhelmed. One pharmacist said: "I’ve had patients cry because I didn’t know when their drug would come back. I didn’t know either."
When providers don’t communicate, everyone suffers.
What’s Working-And What’s Next
Some places are getting it right. Mayo Clinic’s SHIP protocol reduced patient complaints by 65%. Memorial Sloan Kettering assigns communication specialists to handle cancer drug shortages-no provider is left alone with a terrified patient.
Even the FDA is stepping up. Their new Drug Shortage Communication Collaborative now requires manufacturers to provide ready-to-use patient materials within 24 hours of a shortage being declared. That’s a game-changer.
By 2025, AI tools will predict shortages before they happen-based on supply chain data, manufacturing delays, and even weather patterns affecting raw materials. But technology won’t replace human connection. It will just free up time for providers to do what matters most: talk to patients.
Patients don’t need perfect systems. They need to know someone is looking out for them. That’s the real job of a provider during a drug shortage-not just prescribing, but protecting.
What should I do if my medication is suddenly unavailable?
Don’t stop taking it without talking to your provider. Call your doctor’s office right away-even if it’s after hours. Many clinics have on-call providers for this exact situation. Ask: "Is there a safe alternative? Why is this drug gone? When will it come back?" Write down their answers. If you’re not satisfied, ask to speak with a pharmacist or care coordinator.
Are generic drugs always safe substitutes?
Most of the time, yes. Generic drugs have the same active ingredient, strength, and effect as brand-name versions. But not all generics are equal. Some have different fillers or release mechanisms that can affect how they work in your body. Your provider should explain why they chose a specific generic and whether it’s been tested for your condition. If you’ve had bad reactions to a generic before, say so. Your history matters.
Can I request my original medication even if it’s on shortage?
You can ask, but providers can’t guarantee it. If the shortage is severe, pharmacies may not be able to get it at all-even if you’re willing to pay extra. Providers are ethically and legally bound to prescribe what’s safe and available. Pushing for an unavailable drug can delay your care or put you at risk if you’re forced to use an unsafe alternative. Trust your provider’s judgment-but ask for the reasoning behind their choice.
How do I know if my provider is following best practices?
Look for these signs: They explain why the drug is unavailable using simple language. They offer at least one alternative with clear benefits. They ask you to repeat back what you’ll do next. They give you written or emailed info. They follow up within a week. If none of this happens, it’s okay to ask for a care coordinator or switch providers. Good communication isn’t a bonus-it’s part of your right to care.
What if I can’t afford the alternative medication?
Cost is a real barrier. Tell your provider. Many clinics have drug assistance programs, coupons, or connections to nonprofit organizations that help with medication costs. Some manufacturers offer free samples during shortages. Pharmacies sometimes have discount programs for generics. Never assume you can’t afford it-ask. Your provider’s job is to find a solution that works for your health and your budget.







vikas kumar
November 25, 2025 AT 15:09 PMBeen there. My dad’s heart med ran out last year and the pharmacy just shrugged. No call, no plan. He ended up skipping doses for 10 days. We didn’t know it was a shortage until we called the doctor. Providers need to stop treating this like a logistics problem and start treating it like a human one.
Vanessa Carpenter
November 27, 2025 AT 05:36 AMI work in a clinic and we started using the Chunk, Check, Change method last month. It’s not magic, but it cuts down on panic calls by like 60%. Patients actually remember what we tell them now. Small change, huge difference.
Damon Stangherlin
November 27, 2025 AT 14:57 PMSo many docs still think 'just hand them a pill and go' is fine. But when you're scared, you don't care about the brand name-you care if you're gonna be okay. I've seen patients cry because their chemo med was swapped without explanation. It's not just about info, it's about feeling safe. The 78% stat? That's not a number, that's a person. And we owe them better.
Also, the visual charts? Genius. I printed one for my aunt with diabetes when her insulin switched. She showed it to her whole family. That’s the kind of thing that sticks.
And yeah, rural folks get left out. My cousin in Nebraska had to drive 90 miles to get a refill because the local pharmacy didn't even know the drug was short. We need better systems, not just better words.
AI predicting shortages? Cool. But if the provider still talks like a robot, none of it matters. Tech helps. Humanity heals.
Also, typo: 'imipramine' not 'imipramine'. But you get the point. 😅
hannah mitchell
November 27, 2025 AT 15:48 PMMy mom’s on a med that’s been out for 8 months. We’ve gotten three different generics. None of them came with a real explanation. Just a note in the portal. I had to Google half of it. Providers: stop treating patients like they’re IT help desks.
Bea Rose
November 29, 2025 AT 01:15 AM73% lose trust. 18% stop meds. 3.2x more confusion for non-English speakers. These aren’t anecdotes. They’re data points. And yet, nothing changes. Because accountability is hard and paperwork is easy.
Michael Collier
November 30, 2025 AT 14:18 PMIt is imperative that healthcare institutions recognize that the communication protocols delineated herein are not merely procedural enhancements, but foundational elements of ethical patient care. The Joint Commission’s forthcoming mandate is not a burden, but a necessary alignment with the Hippocratic imperative to do no harm through omission.
Furthermore, the implementation of standardized, evidence-based communication frameworks-such as the Chunk, Check, Change methodology-constitutes a demonstrable improvement in patient comprehension and adherence, as evidenced by the Kaiser Permanente case study.
It is therefore recommended that all accredited facilities adopt these practices without delay, and that institutional leadership prioritize training, resource allocation, and audit mechanisms to ensure compliance.
Shannon Amos
December 1, 2025 AT 04:47 AMSo let me get this straight. We’re telling doctors they have to explain drug shortages like they’re explaining a Netflix subscription? Cool. Meanwhile, the FDA’s still letting companies wait six months to report a shortage. Like, maybe fix the supply chain before you make us all babysit patients’ anxiety?
Wendy Edwards
December 3, 2025 AT 04:26 AMI’m a nurse and I’ve seen this play out too many times. One lady came in crying because her blood pressure med was swapped and she thought she was being poisoned. She’d read the label wrong and thought the new pill had ‘poison’ in the ingredients. It was just ‘magnesium stearate’ but she didn’t know what that meant. We sat there for 20 minutes. Drew a picture. She finally smiled. That’s the job. Not the script. Not the EHR pop-up. The human moment. And if you’re not doing that? You’re just a pill dispenser with a stethoscope.
Also, cost matters. I had a patient who refused her new med because she thought it was ‘expensive’. Turned out she was scared she couldn’t afford it. We found a coupon. She cried again. But this time, it was because she was relieved. We need to talk about money. It’s not embarrassing. It’s real.
And to the guy who said ‘imipramine’ wrong? Yeah, I did that too last week. We’re all human. Just don’t forget the people on the other side of the chart.