Amoeba Infection Risk Calculator
Your Risk Assessment
Common Symptoms to Watch For
- Severe headache, stiff neck, fever, vomiting, rapid neurological decline
- Bloody diarrhea, abdominal cramping, fever
- Eye pain, redness, blurred vision, photophobia
- Headache, seizures, focal neurological deficits
Recommended Preventive Measures
- Boil drinking water for at least one minute, especially in endemic regions
- Use NSF-certified filters that remove cysts (rated at 1 micron or smaller)
- Avoid submerging your head in warm freshwater lakes or poorly maintained pools
- Disinfect contact lenses with appropriate solutions; replace cases every three months
amoeba infections are often misunderstood, yet they cause serious illness and occasional deaths worldwide. This article breaks down the science, the global impact, and practical steps you can take to protect yourself and your community.
Key Takeaways
- Amoebae can cause both gastrointestinal disease and deadly brain infections.
- Free‑living amoebae are found in warm fresh water, soil, and even tap water systems.
- Millions of cases of amoebic dysentery occur each year, while rare brain infections claim dozens of lives annually.
- Early diagnosis and proper treatment dramatically improve outcomes.
- Simple water‑handling practices can cut the risk of infection.
What Are Amoeba Infections?
When discussing amoeba infections infections caused by single‑cell protozoa that can invade human tissue, leading to disease ranging from mild diarrhea to fatal brain inflammation, we’re dealing with a diverse group of organisms. Some live inside the human gut as harmless commensals, while others-known as free‑living amoebae-thrive in the environment and become opportunistic pathogens when they enter the body.
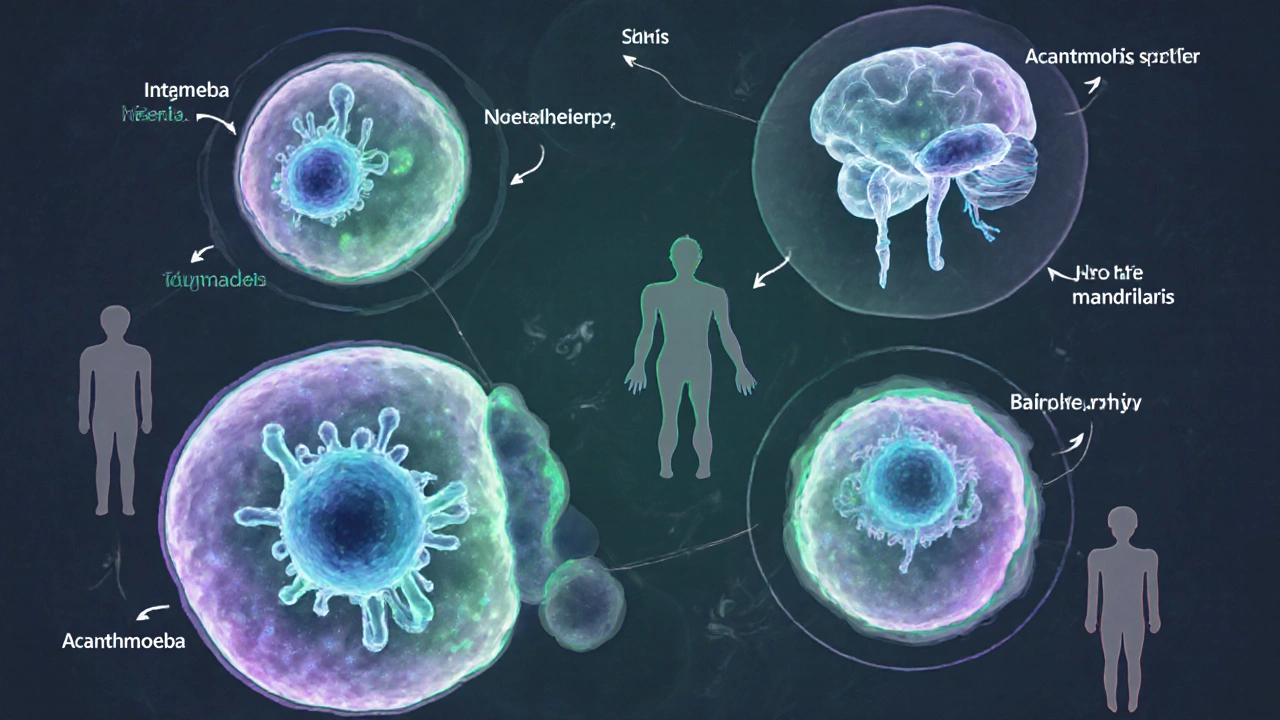
Types of Pathogenic Amoebae
Not all amoebae pose a threat, but a handful are responsible for most human disease.
- Entamoeba histolytica the cause of amoebic dysentery, a severe intestinal infection that can spread to the liver
- Naegleria fowleri the “brain‑eating” amoeba that invades the central nervous system via the nasal passages
- Balamuthia mandrillaris causes granulomatous amoebic encephalitis (GAE), affecting both immunocompromised and healthy individuals
- Acanthamoeba spp. linked to keratitis in contact‑lens wearers and also to GAE
- Free‑living amoeba a broad category that includes the above species and lives in soil, lakes, hot springs, and even municipal water supplies
Global Burden and Recent Outbreaks
The World Health Organization (WHO the UN agency leading global health surveillance and response) estimates that amoebic dysentery accounts for up to 100million cases and 70000 deaths annually, predominantly in low‑resource regions with poor sanitation.
In contrast, Naegleria fowleri infections are rare-about 150 reported cases worldwide each year-but they carry a mortality rate above 95%. Outbreaks often surface after heavy rains fill swimming holes, as documented in the United States during the 2022 summer spike in the southern states.
Recent reports from Brazil, India, and Kenya highlight rising cases of Acanthamoeba keratitis, tied to increased contact‑lens use without proper hygiene. Meanwhile, climate change is expanding the geographic range of thermophilic amoebae, pushing them into temperate zones previously considered safe.
How People Get Infected
Understanding transmission pathways lets you break the chain of infection.
- Contaminated water ingestion: Drinking untreated or poorly filtered water containing Entamoeba histolytica cysts leads to intestinal infection.
- Nasal exposure: Diving or water‑sports in warm freshwater can force water up the nose, delivering Naegleria fowleri trophozoites directly to the brain.
- Skin or eye contact: Open wounds or contact‑lens mishandling expose the eye to Acanthamoeba spores, causing keratitis.
- Inhalation of aerosols: Some free‑living amoebae become airborne in dust storms, leading to rare respiratory infection.
- Medical devices: Inadequately sterilized equipment can harbor amoebae, a risk noted in dialysis units.
The Centers for Disease Control and Prevention (CDC the U.S. public health authority monitoring infectious disease trends) stresses that most cases are preventable with basic water safety and hygiene.
Symptoms and Clinical Presentation
| Infection | Primary Symptoms | Typical Onset | Mortality (if untreated) |
|---|---|---|---|
| Entamoeba histolytica (amoebic dysentery) | Bloody diarrhea, abdominal cramping, fever | 1‑2 weeks after exposure | ≈50% |
| Naegleria fowleri (primary amebic meningoencephalitis) | Severe headache, stiff neck, fever, vomiting, rapid neurological decline | 2‑5 days after nasal exposure | ≈95% |
| Acanthamoeba spp. (keratitis) | Eye pain, redness, blurred vision, photophobia | Weeks after lens contamination | Low, but can cause blindness |
| Balamuthia mandrillaris (granulomatous amoebic encephalitis) | Headache, seizures, focal neurological deficits | Weeks to months after skin or respiratory exposure | ≈90% |
Diagnosis, Treatment, and Outcomes
Timely diagnosis hinges on clinical suspicion and laboratory testing.
- Stool microscopy and antigen detection confirm Entamoeba histolytica. PCR offers higher sensitivity. \n
- CSF analysis-including PCR and culture-identifies Naegleria fowleri or Balamuthia.
- Corneal scrapings examined with confocal microscopy detect Acanthamoeba cysts.
Effective therapies differ by species:
- E. histolytica: Metronidazole followed by a luminal agent (e.g., paromomycin) clears intestinal and cyst stages.
- Naegleria fowleri: Combination of amphotericin B, miltefosine, rifampin, and azithromycin, administered within 48hours, improves survival.
- Acanthamoeba keratitis: Topical polyhexamethylene biguanide (PHMB) or chlorhexidine, often combined with oral itraconazole.
- Balamuthia: High‑dose flucytosine, pentamidine, sulfadiazine, and azithromycin-an aggressive regimen.
Outcomes improve dramatically when treatment starts early. For example, a 2023 multicenter study showed 30% survival for Naegleria infection when therapy began within 24hours, versus 5% when delayed.
Prevention: What You Can Do Today
Because many infections stem from water, focus on safe water practices.
- Boil drinking water for at least one minute, especially in endemic regions.
- Use NSF‑certified filters that remove cysts (rated at 1 micron or smaller).
- Avoid submerging your head in warm freshwater lakes or poorly maintained pools; wear a nose clip if you must.
- Disinfect contact lenses with appropriate solutions; replace cases every three months.
- Maintain household plumbing-regularly disinfect water heaters and replace old pipes.
- Support community-level sanitation projects that improve sewage treatment.
Public health agencies recommend that municipalities monitor water for free‑living amoebae, especially during heatwaves that boost amoeba growth.
Future Challenges and Research Directions
Despite advances, several gaps persist.
- Surveillance gaps: Many low‑income countries lack routine testing for amoebic pathogens, leading to under‑reporting.
- Therapeutic limitations: Drugs like miltefosine are expensive and not widely available; research into novel anti‑amoebic agents is ongoing.
- Climate impact: Rising temperatures expand habitats for thermophilic amoebae, demanding climate‑adapted public‑health strategies.
The WHO continues to develop guidelines for water‑borne protozoan monitoring, while the CDC offers a toolbox for clinicians to recognize and report rare amoebic infections. Collaboration between researchers, engineers, and policymakers will be key to turning the tide on this hidden global health threat.

Frequently Asked Questions
Can I get amoebic dysentery from tap water?
Yes, if the municipal water isn’t properly treated. In many developing regions, untreated or poorly filtered tap water can carry Entamoeba histolytica cysts. Boiling or using a certified filter eliminates the risk.
Is there a vaccine against free‑living amoebae?
Currently, no vaccine exists for any free‑living amoeba. Research is exploring antigen‑based candidates, but progress has been slow due to the organisms’ complex life cycles.
What’s the difference between a cyst and a trophozoite?
A cyst is the dormant, highly resistant form that survives harsh conditions and is the main vehicle for transmission. A trophozoite is the active, feeding stage that causes tissue damage once it reaches a suitable environment inside the host.
How quickly does Naegleria fowleri act after exposure?
Symptoms usually appear within 2‑5days. The disease progresses rapidly, often leading to death within a week if not treated urgently.
Are contact‑lens solutions effective against Acanthamoeba?
Most multipurpose solutions kill the trophozoite form but may not fully eradicate cysts. Rotating to a hydrogen peroxide system or daily disinfecting with a fresh solution reduces the risk significantly.








Michelle Zhao
October 4, 2025 AT 17:06 PMWhile the exposition on amoebic threats is undeniably thorough, one cannot help but note the tendency to amplify panic rather than inform. The prose, though replete with data, drifts toward melodrama, suggesting that every tap water sip is a death sentence. A measured approach, emphasizing risk stratification, would serve the readership far better.
Eric Parsons
October 5, 2025 AT 12:33 PMPhilosophically speaking, fear is a natural response to the unknown, yet it is also a catalyst for rational precaution. The article rightly outlines the pathogenic mechanisms of Entamoeba histolytica and Naegleria fowleri, but a practical guide-such as routine boiling durations-could bridge the gap between knowledge and action. In short, balance curiosity with concrete steps.
Mary Magdalen
October 6, 2025 AT 07:59 AMFrom an American standpoint, it’s laughable how often foreign media sensationalize protozoan microbes as if they’re a national security threat. Our water treatment standards are among the world’s best, and yet the article paints a picture of imminent doom for anyone sipping tap water. Let’s keep things in perspective: the real danger lies in complacency, not exotic pathogens.
Dhakad rahul
October 7, 2025 AT 03:26 AMAh, but dear compatriot, you overlook the pride of our indigenous water sources, pristine yet perilous when ignored! The drama of a "brain‑eating" amoeba stalking unsuspecting swimmers is as exhilarating as any Bollywood climax 😎. Remember, humility before nature is paramount, even for the most advanced nations.
William Dizon
October 7, 2025 AT 22:53 PMHey folks, just wanted to add a friendly reminder: if you’re traveling to regions with unreliable sanitation, a portable NSF‑certified filter is a game‑changer. Boiling water for a full minute kills cysts, and using proper lens disinfectant slashes eye‑infection risk dramatically. Stay safe and enjoy those adventures!
Jenae Bauer
October 8, 2025 AT 18:19 PMSure, your advice is helpful, but have you considered the hidden agenda of big water corporations? They profit from keeping us afraid, pushing pricey filters while the real cure is simple community sanitation. I suspect there’s a coordinated effort to sustain a market for fear‑based products.
vijay sainath
October 9, 2025 AT 13:46 PMLook, the data is crystal clear: amoebic infections are rare in developed nations, and the article overstresses the risk. People need to focus on real threats like antibiotic resistance, not chase every microscopic organism.
Daisy canales
October 10, 2025 AT 09:13 AMWow, such a subtle point you made.
keyul prajapati
October 11, 2025 AT 04:39 AMWhen evaluating the global burden of amoebic diseases, one must adopt a multi‑faceted perspective that encompasses epidemiology, environmental science, and public health policy. First, the prevalence of Entamoeba histolytica in low‑resource settings correlates strongly with inadequate sewage infrastructure. Second, climate change is expanding the habitable range of thermophilic species such as Naegleria fowleri, which thrive in warm freshwater bodies. Third, the pathophysiology of these organisms reveals a dichotomy: cysts enable environmental persistence, while trophozoites drive tissue invasion. Fourth, diagnostic challenges arise because many laboratories lack PCR capability, leading to under‑reporting. Fifth, treatment regimens differ markedly; metronidazole remains the cornerstone for intestinal amoebiasis, whereas amphotericin B combined with miltefosine offers the only hope for primary amebic meningoencephalitis. Sixth, public health interventions, such as community education on water boiling practices, have demonstrated measurable reductions in incidence. Seventh, the role of contact lens hygiene cannot be overstated, as Acanthamoeba keratitis accounts for a notable proportion of sight‑threatening infections in developed countries. Eighth, water treatment plants must consider installing ultrafiltration membranes capable of removing cysts smaller than one micron. Ninth, policy frameworks should mandate routine monitoring of municipal water for free‑living amoebae, especially during heatwaves. Tenth, international collaboration through WHO and CDC can streamline reporting standards to generate more accurate global estimates. Eleventh, research into novel anti‑amoebic compounds, such as nitroimidazole derivatives, is progressing but faces funding hurdles. Twelfth, public awareness campaigns leveraging social media have the potential to disseminate preventive measures rapidly. Thirteenth, travel medicine clinics should incorporate amoeba risk assessments into pre‑travel consultations. Fourteenth, clinicians must maintain a high index of suspicion when encountering patients with unexplained neurological decline after freshwater exposure. Fifteenth, ultimately, a coordinated effort that blends scientific insight, community engagement, and robust infrastructure will be essential to curtail the hidden menace of amoebic infections.
Alice L
October 12, 2025 AT 00:06 AMEsteemed colleagues, I concur with the comprehensive analysis presented above and would like to emphasize the necessity of adhering to WHO guidelines for water safety. Implementing routine cyst surveillance and promoting public education are paramount.
Seth Angel Chi
October 12, 2025 AT 19:33 PMThe article overstates the threat and underplays existing safeguards.
Kristen Ariies
October 13, 2025 AT 14:59 PMWow!!! Absolutely! The data is compelling, and yet we must remember that vigilance is the key!!! Every precaution-boiling, filtering, lens care-saves lives!!! Let's spread the word!!!
Ira Bliss
October 14, 2025 AT 10:26 AM💧🦠 Staying safe from amoebas is easier than you think! Just boil, filter, and keep those lenses sparkling clean! 🌟👍
Donny Bryant
October 15, 2025 AT 05:53 AMGreat tips! Boiling water for a minute is simple and effective.
kuldeep jangra
October 16, 2025 AT 01:19 AMAllow me to elaborate on the importance of community-level interventions, for they form the backbone of any sustainable public‑health strategy. When we speak of safeguarding populations from protozoan threats, the first pillar is education; workshops that teach proper water treatment methods empower individuals to take charge of their own safety. The second pillar involves infrastructure development-investing in reliable filtration systems and maintaining chlorination processes at municipal plants ensures that pathogens are neutralized before reaching households. Moreover, integrating local health workers into surveillance networks facilitates rapid detection of outbreak clusters, enabling swift containment measures. It is also critical to foster partnerships between governments, NGOs, and private enterprises to fund research into affordable, point‑of‑use technologies. In regions where resources are scarce, low‑cost solutions such as solar‑powered UV purifiers have shown promising results. Finally, consistent messaging through radio, social media, and school curricula reinforces best practices and builds a culture of vigilance. By weaving together education, infrastructure, surveillance, and collaboration, we can dramatically reduce the burden of amoebic diseases worldwide.
harry wheeler
October 16, 2025 AT 20:46 PMCommunity effort and low‑cost tech are key.
faith long
October 17, 2025 AT 16:13 PMI hear the call for collective action, and I must stress that complacency is the enemy of progress. When we stand idle, the microscopic invaders seize any lapse in hygiene to proliferate unchecked. It is not enough to merely advise boiling water; we must demand that local authorities allocate budgets for water treatment upgrades, and that schools integrate hands‑on demonstrations of filtration. The stakes are high-every misstep can translate to a life lost, a vision blurred, a family shattered. We owe it to ourselves to push for rigorous standards, to hold policymakers accountable, and to champion transparent reporting of infection rates. Only through relentless advocacy and personal responsibility can we turn the tide against these invisible foes.