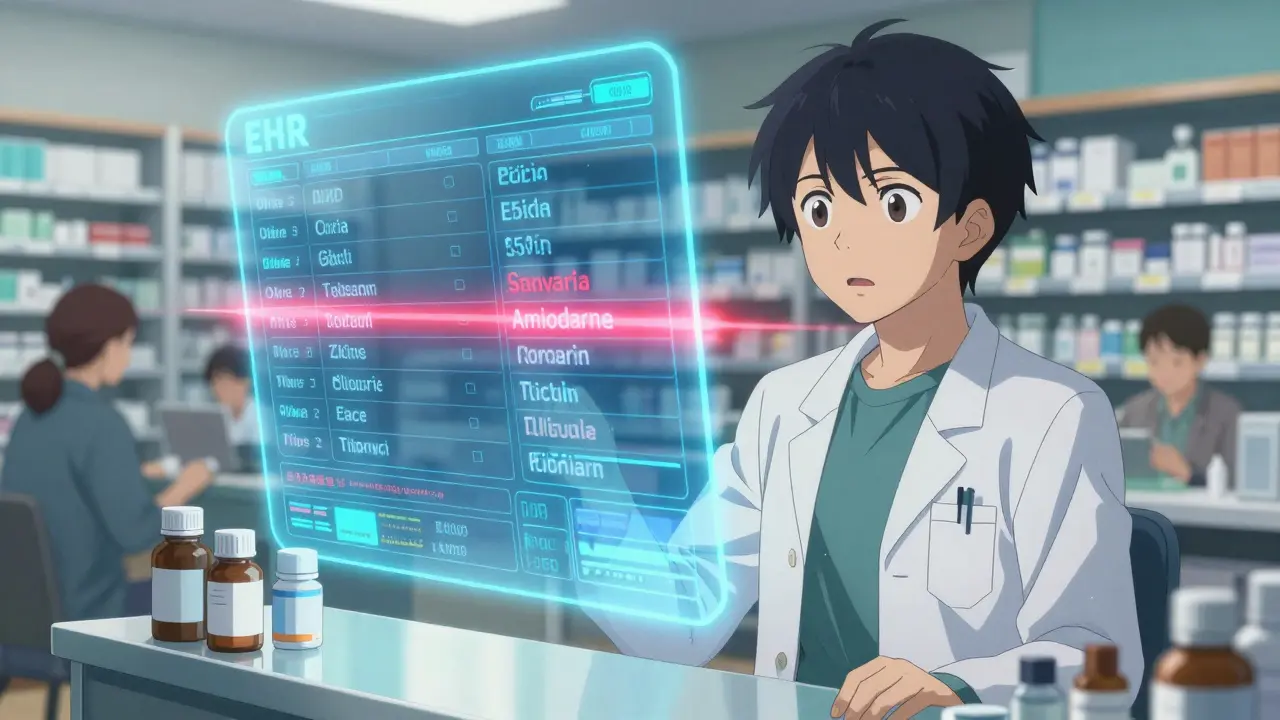
Imagine this: You’re a pharmacist. A patient walks in with a new prescription for warfarin. You check their history and see they’ve been taking amiodarone for months. That’s a dangerous combo. You call the doctor. They haven’t seen the patient in six months. The prescription came through electronically, but the doctor has no idea about the other meds the patient is on. You spend 20 minutes on the phone. The patient leaves with the script, but the risk stays. Now imagine if your pharmacy system could EHR integration directly with the doctor’s system - and show you every drug, lab result, and allergy in real time. No calls. No delays. Just safety.
Why EHR Integration Matters More Than Ever
In 2025, most U.S. pharmacies still operate in the dark when it comes to patient data. Even though over 76% of prescriptions are sent electronically, only 15-20% of pharmacies can actually see what’s happening in the provider’s electronic health record (EHR). That gap isn’t just inconvenient - it’s deadly. Medication errors cause over 7,000 deaths each year in the U.S., and nearly half of them happen because providers and pharmacists aren’t talking to each other. EHR integration fixes that. It means your pharmacy system can automatically pull up a patient’s full medication list, recent lab values, allergies, and even care plans from the doctor’s EHR. And it works both ways: pharmacists can send back notes about drug interactions, adherence issues, or dosage tweaks - and those notes show up right in the provider’s chart. No more sticky notes, no more missed messages. This isn’t science fiction. It’s happening - slowly. A 2021 proof-of-concept study in East Tennessee showed that when independent pharmacies connected their systems to Epic EHR, providers accepted 92% of the clinical interventions pharmacists suggested. That’s not a small win. That’s a revolution in care.How EHR Integration Actually Works
There are two main standards keeping this system running: NCPDP SCRIPT and HL7 FHIR. NCPDP SCRIPT (version 2017071) is what sends the actual prescription from the doctor’s office to the pharmacy. It’s been around for decades and handles the basics: drug name, dose, quantity, instructions. Simple. Reliable. But SCRIPT doesn’t tell you anything about the patient’s history. That’s where HL7 FHIR (Fast Healthcare Interoperability Resources) comes in. FHIR is the new language of health data. It lets systems share detailed clinical info - like kidney function tests, recent hospital discharges, or a list of all current meds - in a structured, machine-readable format. The Pharmacist eCare Plan (PeCP), built on FHIR, lets pharmacists document their clinical recommendations and send them straight into the provider’s EHR. The technical side isn’t easy. Systems need secure APIs with OAuth 2.0 authentication, TLS 1.2+ encryption, and strict HIPAA compliance. Every data exchange must be logged. Audit trails are mandatory under the 21st Century Cures Act. That’s why big players like Surescripts dominate - they’ve built the infrastructure. They process over 22 billion transactions a year, including medication history checks, eligibility verification, and electronic prior authorizations. For a pharmacy, connecting to Surescripts means instant access to data from 97% of U.S. pharmacies.Real Benefits - Numbers That Matter
The data doesn’t lie. When EHR integration works, outcomes improve - fast. - Medication errors drop by 48% thanks to automated alerts for interactions and duplications. (UpToDate, 2023) - Prescription processing time falls from 15.2 minutes to 5.6 minutes per script. That’s a 63% time savings. (EnlivenHealth® study, 2022) - Pharmacists identify 4.2 medication problems per patient visit - up from 1.7 without EHR access. (Snyder et al., 2020) - Hospital readmissions due to medication issues drop by 31% in integrated systems. (University of Tennessee, 2022) - Patients are 23% more likely to stick to their meds when pharmacists can monitor and adjust therapy in real time. (PMC, 2022) One community pharmacy in Ohio saw a 40% reduction in calls from patients asking why their prescription was denied - because now, when a prior authorization fails, the system auto-notifies the provider and suggests alternatives. The pharmacist doesn’t have to chase it down. In Australia, the My Health Record system cut preventable hospitalizations by 27% just by giving pharmacists access to full medication histories. That’s the same outcome we can achieve here - if we fix the barriers.
The Big Barriers - Why It’s Not Everywhere
You’d think with benefits like these, everyone would jump on board. But here’s the truth: most independent pharmacies still can’t do it. The biggest problem? Cost. Installing and maintaining integration can run $15,000 to $50,000 upfront - plus $5,000 to $15,000 a year in maintenance. For a small pharmacy, that’s more than their annual software budget. Then there’s time. Pharmacists average just 2.1 minutes per patient interaction. Even if they had EHR access, they don’t have time to dig through it. A 2021 survey found 68% of pharmacists feel overwhelmed trying to use the data during busy shifts. Technical chaos is another nightmare. There are over 120 different EHR systems in the U.S. and 50+ pharmacy software platforms. They don’t talk to each other. Data mapping errors happen in 73% of integration attempts. One pharmacy might use Epic. Another uses Cerner. The pharmacy software? Maybe PioneerRx or RxConnect. Getting them to sync? It’s like trying to plug a USB-C cable into a PS/2 port. And reimbursement? Almost nonexistent. Only 19 states had payment models for pharmacist EHR-based services as of early 2024 - even though 48 states let pharmacists prescribe. Without being paid for their clinical work, pharmacies can’t justify the cost. The result? Only 3 out of 127 community pharmacies in Wisconsin had formal EHR access agreements with local health systems. That’s less than 0.01% of pharmacists in the state.Who’s Doing It Right - And How
Some are breaking through. Surescripts is the backbone. Their Medication History service gives pharmacies access to 3.5 billion annual transactions - meaning they can pull up a patient’s full prescription history across all providers and pharmacies. It’s not perfect, but it’s the closest thing we have to a national network. SmartClinix and DocStation offer pharmacy-specific EHR platforms that integrate with major systems like Epic and Cerner. SmartClinix starts at $199/month per provider, with a $1,500 setup fee. Users praise the seamless integration but complain about the learning curve. DocStation’s strength? Billing and provider network management - great for clinics that want to offer medication therapy management (MTM) services. The University of Tennessee pilot showed that even small, independent pharmacies can integrate successfully - if they have the right partner. They used EnlivenHealth® to connect PioneerRx with Epic across 12 pharmacies and 3 clinics. Over 1,800 clinical interventions were documented. Providers accepted them almost every time. The key? Start small. Don’t try to connect everything at once. Begin with medication history access. Then add alerts. Then let pharmacists send notes back. Build the workflow slowly.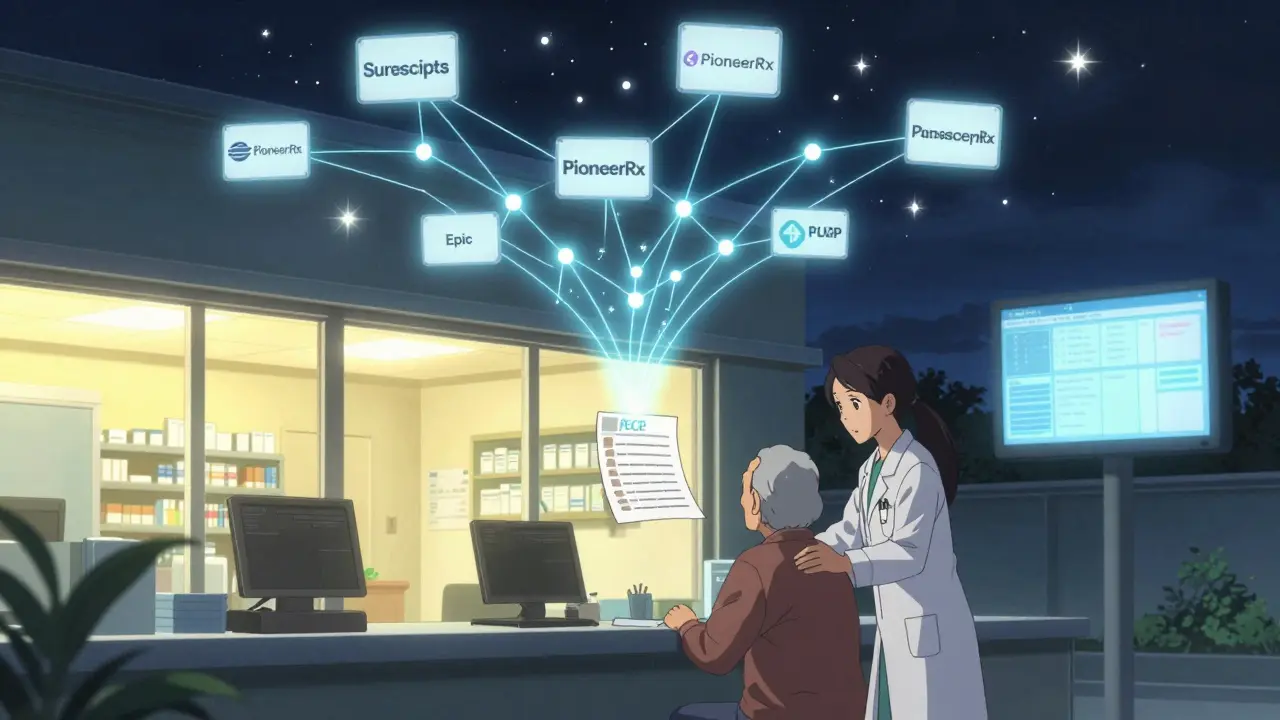
What’s Next - And How to Prepare
The future is coming - whether you’re ready or not. By 2026, California will require all pharmacies offering MTM services to have EHR integration. CMS has already mandated that Medicare Part D plans with 4+ star ratings must have integrated pharmacy-provider communication. The Office of the National Coordinator for Health IT wants 50% of community pharmacies to have bidirectional EHR access by 2027. New tools are on the horizon. The CARIN Blue Button 2.0 system lets patients share their own data from insurers directly with pharmacies. NCPDP is rolling out PeCP Version 2.0 in late 2024 with smarter clinical decision support. CVS and Walgreens are testing AI that scans integrated data to flag high-risk patients - and they’re seeing a 37% increase in intervention accuracy. For pharmacies looking to get started:- Assess your readiness. Do you have staff trained in FHIR or HL7? Do you have a dedicated IT contact?
- Start with Surescripts’ Medication History service. It’s the lowest barrier to entry.
- Partner with a local health system or clinic. Ask if they’ll let you connect to their EHR. Offer to reduce their prior authorization backlog.
- Apply for state or federal grants. Some programs help small pharmacies cover integration costs.
- Train your team. Don’t just teach them how to use the system - teach them how to act on the data.
The Bottom Line
EHR integration isn’t about technology. It’s about trust. It’s about recognizing that pharmacists aren’t just pill counters - they’re medication experts who see patients more often than most doctors. When systems talk to each other, care gets smarter, safer, and faster. The gap between where we are and where we need to be is wide. But the cost of doing nothing is higher. Patients are still getting the wrong meds. Hospitals are still filling with preventable readmissions. Pharmacists are still wasting hours on phone calls. Integration isn’t optional anymore. It’s the next standard of care. The question isn’t whether you’ll do it. It’s when - and how well.What is EHR integration for pharmacies?
EHR integration for pharmacies means connecting a pharmacy’s management system directly to a healthcare provider’s electronic health record. This allows pharmacists to view a patient’s full medical history - including medications, allergies, lab results, and diagnoses - and send clinical notes back to the provider in real time. It’s a two-way data exchange that improves medication safety and care coordination.
How does EHR integration reduce medication errors?
Integrated systems automatically flag dangerous drug interactions, duplicate prescriptions, and incorrect dosages before the prescription is filled. They also show pharmacists what other drugs the patient is taking - something they wouldn’t know if they only saw the new script. Studies show this reduces medication errors by up to 48%.
Why don’t all pharmacies have EHR integration?
Cost is the biggest barrier - independent pharmacies face $15,000 to $50,000 in setup fees and $5,000-$15,000 annually in maintenance. Technical complexity, incompatible systems, lack of reimbursement for pharmacist services, and limited staff time also prevent adoption. Only 15-20% of U.S. pharmacies currently have full bidirectional integration.
Can patients access their own data through EHR integration?
Yes. Through systems like CARIN Blue Button 2.0, patients can download their prescription and claims history from insurers and share it directly with their pharmacy. This gives pharmacists even more complete data - even if the provider’s EHR isn’t fully integrated yet.
What’s the difference between SCRIPT and FHIR in pharmacy integration?
NCPDP SCRIPT is the standard for sending electronic prescriptions - it’s about the order. HL7 FHIR is for sharing clinical data - like lab results, allergies, and care plans. SCRIPT tells the pharmacy what to dispense. FHIR tells them why, and what else the patient is taking. Both are needed for full integration.
Is EHR integration required by law?
Not yet for all pharmacies, but regulations are pushing hard. The 21st Century Cures Act bans information blocking, meaning providers can’t refuse to share data with pharmacies. CMS requires Medicare Part D plans with high ratings to have integrated communication. California mandates it for MTM services by 2026. Federal goals aim for 50% of community pharmacies to be integrated by 2027.
What should a small pharmacy do first to start integration?
Start with Surescripts’ Medication History service - it’s the easiest and most widely supported entry point. It gives you access to a patient’s full prescription history across all pharmacies and providers. Once you’re using that, explore connecting with a local clinic or health system to test two-way data exchange. Focus on one clinical use case first, like reducing prior authorization delays.
How long does EHR integration take to implement?
For an independent pharmacy, it typically takes 3 to 6 months. The process includes a readiness assessment (2-4 weeks), technical setup (8-12 weeks), staff training (4-8 weeks), and testing. Some parts, like connecting to Surescripts, can be done in weeks. Full bidirectional integration with a provider’s EHR takes longer due to data mapping and credentialing delays.










Janice Holmes
December 28, 2025 AT 04:56 AMOH MY GOD. I just had a patient come in with warfarin and amiodarone-same scenario. I called the prescriber, they said, 'Oh, we didn't know she was on it.' I nearly cried. This isn't just inefficiency-it's a waiting room for preventable hemorrhages. 🤯 EHR integration isn't a 'nice-to-have,' it's a life-or-death firewall. And yet we're still using fax machines in 2025? I'm not mad, I'm just disappointed. 😭
Alex Lopez
December 28, 2025 AT 06:21 AMWhile the data presented is compelling, one must consider the systemic inertia inherent in healthcare IT. The notion that interoperability is solely a technical challenge is a fallacy; it is, in fact, a sociopolitical and economic one. The 15-20% adoption rate reflects not technological deficiency, but the absence of a unified regulatory incentive structure. One cannot simply 'integrate' when stakeholders are misaligned in reimbursement models, liability frameworks, and data governance protocols. The solution requires legislative intervention, not merely API endpoints.
Liz Tanner
December 29, 2025 AT 22:20 PMAs a pharmacist who’s been doing this for 18 years, I’ve seen the pain points firsthand. But I’ve also seen how small steps add up. We started with Surescripts Medication History last year-just that one piece-and our error rate dropped 30% in 6 months. No fancy EHR, no $50k investment. Just access to what patients were actually taking. If you’re scared to start, just do that. It’s free. It works. You don’t need to boil the ocean to save a life.
John Barron
December 31, 2025 AT 11:58 AMLet me be perfectly clear: the entire EHR integration narrative is a distraction orchestrated by Surescripts and Epic to lock in monopolistic control over clinical data. The real problem? The FDA and CMS incentivize volume over value. They pay for scripts, not safety. They pay for filling bottles, not preventing overdoses. And now they’re pushing FHIR like it’s a miracle cure while ignoring that 73% of data mappings fail because the underlying data is garbage-in, garbage-out. You think your pharmacist can fix a broken system? They’re just the canaries in the coal mine. The system is designed to fail. And you’re all just rearranging deck chairs on the Titanic. 🚢💀
Liz MENDOZA
January 1, 2026 AT 00:35 AMThank you for writing this. I work in a rural pharmacy where we don’t have an IT person. We’re the ones holding the whole thing together. But when I saw that 4.2 medication problems per visit stat-I cried. That’s not just data. That’s me saving people. I’ve had patients say, 'I didn’t know I was taking two of the same thing.' We need more support-not just tech, but time. Maybe we need pharmacy liaisons embedded in clinics. Or at least 15 extra minutes per day to use the tools we have. We’re not just dispensing. We’re healing. And we deserve to be heard.
Miriam Piro
January 2, 2026 AT 00:54 AMThey’re not hiding the data because it’s hard to share-they’re hiding it because they’re making billions off the chaos. Big Pharma, EHR vendors, Surescripts-they all profit from the gaps. Every phone call a pharmacist wastes? That’s billable time for the doctor’s office. Every hospital readmission? That’s revenue for the hospital. Integration would cut their profits. That’s why it’s not happening. The 21st Century Cures Act? A PR stunt. The real power players don’t want transparency. They want control. And you? You’re just the pawn they use to sell the dream of 'better care' while the machine keeps grinding. 🕵️♀️🔍
Paula Alencar
January 3, 2026 AT 03:33 AMWhile the benefits of EHR integration are unequivocally documented, the implementation challenges remain profoundly underestimated. The notion that 'starting small' is sufficient ignores the structural fragmentation of the U.S. healthcare ecosystem. A pharmacy using PioneerRx cannot seamlessly exchange data with a clinic using Epic without middleware, custom HL7 mappings, and a dedicated compliance officer. Moreover, the regulatory burden of HIPAA-compliant audit trails, OAuth 2.0 implementation, and TLS 1.2+ enforcement is not trivial. These are not software bugs-they are institutional barriers. Until federal funding is allocated to subsidize interoperability for independent pharmacies, the promise of EHR integration will remain an aspirational white paper, not a clinical reality.
James Bowers
January 3, 2026 AT 14:17 PMIt is disingenuous to suggest that pharmacists are 'medication experts' when the majority of them lack formal clinical training beyond dispensing. The notion that pharmacists should be sending clinical notes into EHRs is a dangerous overreach. This is not medicine-it is scope creep. The physician remains the primary decision-maker. Allowing pharmacists to 'adjust therapy' without oversight is a liability waiting to happen. The data may look good, but the risk of misinterpretation, especially in polypharmacy cases, is immense. This is not innovation. It is negligence dressed in FHIR.
Will Neitzer
January 5, 2026 AT 09:57 AMI’ve been on the front lines of this for a decade. I work with a health system that integrated 12 community pharmacies with Epic via EnlivenHealth®. The results? 1,800 interventions, 92% acceptance rate, zero adverse events tied to communication gaps. But here’s the secret: we didn’t start with the tech. We started with trust. We held monthly huddles. We let pharmacists sit in on rounds. We gave them a voice. The system followed the culture. If you want integration, build relationships first. The API will come. But if you only care about the API? You’ll fail. And patients will pay the price.
Gerald Tardif
January 6, 2026 AT 07:27 AMOne sentence: Start with Surescripts. Now. Today. Don’t wait for the perfect solution. Just get the history. It’s free. It’s fast. And it saves lives. 🙌