When your lungs can't get enough oxygen, your heart has to work harder. But what happens when the blood vessels in your lungs narrow and stiffen? That’s when pulmonary hypertension starts creeping in - silently, dangerously, and often mistaken for something else entirely.
What Pulmonary Hypertension Really Means
Pulmonary hypertension (PH) isn’t just high blood pressure. It’s high pressure specifically in the arteries that carry blood from your heart to your lungs. Normal pulmonary artery pressure is around 8-20 mmHg at rest. When it climbs above 20 mmHg - confirmed by right heart catheterization - you’re diagnosed with PH. This isn’t a one-size-fits-all condition. The World Health Organization breaks it into five groups:
- Group 1: Pulmonary arterial hypertension (PAH) - the rarest, often genetic or idiopathic
- Group 2: PH due to left heart disease - the most common, tied to heart failure
- Group 3: PH from lung diseases like COPD or pulmonary fibrosis
- Group 4: Chronic thromboembolic PH - caused by old blood clots stuck in lung arteries
- Group 5: PH with unclear causes, like kidney disease or blood disorders
Most people don’t realize they have it until symptoms get bad. And by then, the right side of the heart is already struggling.
Red Flags: Symptoms You Can’t Ignore
Early PH feels like being out of shape. You get winded climbing stairs. Your legs feel heavy. You’re tired all the time. Doctors often mistake it for asthma, anxiety, or aging. But there are clues that don’t lie:
- Progressive shortness of breath - worse than your lung function suggests
- Chest pain or pressure, especially during activity
- Fainting or near-fainting spells
- Swelling in ankles, legs, or belly - not from kidney or liver problems
- Lips or fingers turning blue (cyanosis) in cold weather
- A loud second heart sound (S2) heard through a stethoscope
One patient on Reddit shared: “My doctor told me I was just out of shape for 18 months. My 6-minute walk distance dropped from 520 meters to 220. By the time they tested me, my pulmonary pressure was 58 mmHg.” That’s not normal fatigue. That’s your heart screaming for help.
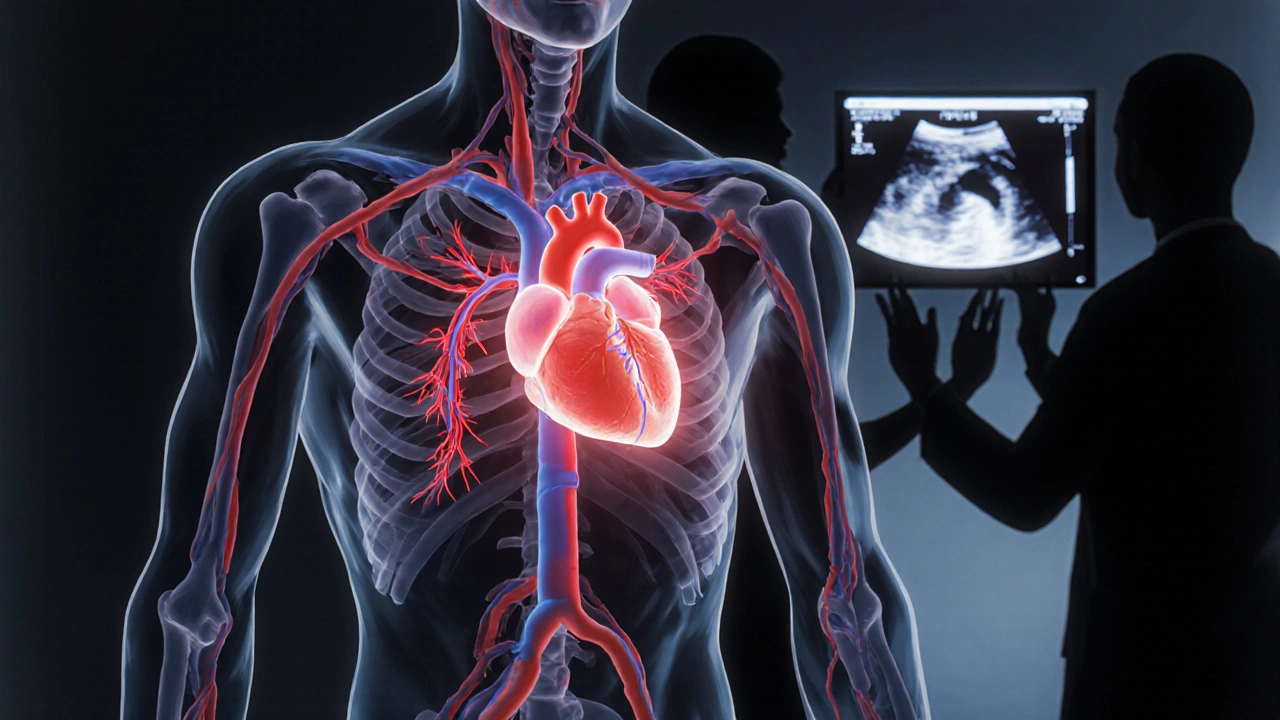
How Right Heart Strain Shows Up - And Why It’s Dangerous
When the pulmonary arteries resist blood flow, the right ventricle - the chamber that pumps blood to the lungs - has to pump harder. Over time, it thickens, stretches, and weakens. This is right heart strain. And if it’s not caught, it leads to right heart failure.
Doctors look for three key signs on echocardiograms:
- Right ventricular wall thickness >5 mm - muscle thickening from overwork
- Right ventricular dilation >22 cm² - the chamber is ballooning
- TAPSE <17 mm - a measure of how well the heart squeezes. Below 17, it’s a red flag.
These aren’t just numbers. They predict survival. A TAPSE under 17 means your risk of death in the next year nearly doubles. BNP and NT-proBNP blood levels above 180 pg/mL and 1,400 pg/mL, respectively, also signal severe strain. High levels mean your heart is releasing stress hormones because it’s failing.
And the 6-minute walk test? If you can’t walk 380 meters without stopping, your prognosis worsens. That’s not a fitness test - it’s a life-or-death gauge.
Diagnosis: Why Echocardiograms Aren’t Enough
Many doctors start with an echocardiogram. It’s quick, non-invasive, and shows if the right side is enlarged. But here’s the problem: it’s only 88% sensitive and 56% specific. That means it misses cases - and falsely flags others. One study found it overestimates pressure by 10-15 mmHg in nearly half the patients.
That’s why right heart catheterization is still the gold standard. It’s the only test that gives you exact numbers: pulmonary artery pressure, cardiac output, and pulmonary vascular resistance. Without it, you can’t tell if it’s Group 1 PAH or Group 2 from heart failure. And treatment depends on that.
Yes, catheterization has risks - arrhythmias, bleeding, pneumothorax. But the risk of misdiagnosis is far worse. Dr. Nazzareno Galiè says it plainly: “Non-invasive methods cannot replace direct pressure measurement.”
Cardiac MRI gives the clearest picture of right heart function - but only 37% of PH centers have it. Most rely on echo + catheterization together. And that’s the standard of care.
Modern Therapy: It’s Not Just One Pill Anymore
Twenty years ago, PH meant a life expectancy of under three years. Today? Five-year survival is over 60%. That’s thanks to combination therapy.
There are now 14 FDA-approved drugs for PH, grouped into five classes:
- Endothelin receptor antagonists (bosentan, macitentan) - block constricting chemicals
- PDE-5 inhibitors (sildenafil, tadalafil) - relax blood vessels
- Prostacyclin analogs (epoprostenol, treprostinil) - IV or inhaled, powerful vasodilators
- Soluble guanylate cyclase stimulators (riociguat) - boost natural vasodilation
- TGF-β inhibitors (sotatercept) - new disease-modifying drug that reverses vessel remodeling
Back in 2015, most patients got one drug. Now, 68% start with two or three together. Why? Because PH attacks from multiple angles. One drug won’t cut it.
Sotatercept, approved in 2021, is a game-changer. In the STELLAR trial, it cut the risk of death or worsening by 44%. For the first time, we’re not just managing symptoms - we’re changing the disease.
But access is uneven. Nearly two-thirds of patients report insurance delays of over 30 days for IV therapies. Some wait months. Every day counts.
Why Specialized Care Matters
Pulmonary hypertension isn’t something your general doctor can handle alone. It takes a team: a pulmonologist, a cardiologist, a PH pharmacist, a nurse coordinator, and sometimes a social worker.
There are only about 35 certified PH centers in the entire U.S. But they treat 75% of patients. Why? Because they know the details. They track TAPSE, NT-proBNP, and 6-minute walk distance every 3-6 months. They adjust meds before you feel worse.
One patient wrote: “The PH clinic caught my right ventricular function dropping to 35% on echo. I had no symptoms yet. They switched my meds. My BNP dropped from 850 to 190 in three months.” That’s early intervention. That’s survival.
PH centers also handle complex logistics: IV pumps, central line care, medication storage, insurance appeals. A dedicated PH nurse reduces hospitalizations by 27%.

What’s Coming Next
The diagnostic threshold dropped from 25 mmHg to 20 mmHg in 2022. That means more people will be diagnosed earlier - potentially increasing cases by 25%. That’s good news, if we’re ready.
Researchers are testing let-7 microRNA as a blood biomarker for early right heart damage. Another trial is looking at dichloroacetate, a drug that helps the right ventricle use energy more efficiently. Early results are promising.
But the biggest barrier isn’t science - it’s equity. Minority patients wait 47% longer for diagnosis. Their mortality rate is 32% higher. Education for primary care doctors is critical. “Red flag” symptoms - unexplained breathlessness, right heart strain on EKG, persistent swelling - need to be recognized early.
What You Can Do
If you’ve been told you’re “just tired,” but your symptoms are getting worse - push back. Ask for an echocardiogram. If your doctor says no, ask for a referral to a pulmonary hypertension specialist. Don’t wait for fainting or swelling. Don’t wait for a crisis.
PH isn’t curable yet. But it’s manageable. With the right care, many people live full, active lives. The key is catching it before the right side of your heart gives out.
Can pulmonary hypertension be cured?
There is no cure for pulmonary hypertension yet. But with modern combination therapies, many patients stabilize their condition, improve their symptoms, and live for many years. In rare cases, lung or heart-lung transplant can be curative, but it’s reserved for the most severe cases that don’t respond to medication.
Is pulmonary hypertension the same as regular high blood pressure?
No. Regular high blood pressure (systemic hypertension) affects arteries throughout the body. Pulmonary hypertension only affects the arteries between the heart and lungs. They’re measured differently, treated differently, and have different causes. You can have one without the other.
How is pulmonary hypertension diagnosed?
Diagnosis starts with an echocardiogram to check for signs of strain. But the only way to confirm it is through right heart catheterization - a procedure where a thin tube is inserted into the heart to directly measure pressure in the pulmonary arteries. Blood tests for BNP and a 6-minute walk test also help assess severity.
What are the risks of right heart catheterization?
The procedure is generally safe when done by experienced teams. Risks include arrhythmia (3.4%), bleeding or hematoma (5.7%), and pneumothorax (1.2%). Serious complications are rare. The bigger risk is not doing the test - missing the diagnosis or misclassifying the type of PH, which leads to wrong treatment.
Can lifestyle changes help with pulmonary hypertension?
Yes - but not as a replacement for medication. Avoiding high altitudes, quitting smoking, getting vaccinated for flu and pneumonia, and following a low-salt diet can help reduce strain on the heart. Light exercise, under medical supervision, can improve stamina. But you still need targeted PH drugs to treat the underlying disease.
Why do some patients delay diagnosis for years?
Symptoms like shortness of breath and fatigue are common and often dismissed as asthma, anxiety, or aging. Many patients see multiple doctors before being referred to a PH specialist. On average, diagnosis is delayed by 2.8 years. Women and minority patients face even longer delays due to bias and lack of provider awareness.
Are there new treatments on the horizon?
Yes. Sotatercept, approved in 2021, is the first drug that reverses blood vessel changes, not just lowers pressure. Trials are now testing oral versions of prostacyclins, gene therapies, and drugs that improve right heart energy use. The LIBERTY trial is also exploring let-7 microRNA as an early warning biomarker - potentially allowing detection before symptoms appear.
Final Thought: Time Is the Enemy
Pulmonary hypertension doesn’t wait. It creeps in, and by the time you feel it, your heart is already working too hard. Early diagnosis saves lives. Knowing the signs - progressive breathlessness, swelling, fainting - and demanding the right tests can make the difference between survival and decline. If you suspect something’s wrong, don’t settle for “it’s just stress.” Push for an echo. Push for a specialist. Your heart is counting on it.










Holly Powell
November 17, 2025 AT 12:36 PMPulmonary arterial hypertension (PAH) is a hemodynamically distinct entity characterized by elevated pulmonary vascular resistance (PVR) >3 Wood units, often with a transpulmonary gradient >12 mmHg and pulmonary capillary wedge pressure ≤15 mmHg. The current ESC/ERS guidelines emphasize early right heart catheterization as the gold standard for diagnosis, particularly in the absence of left heart disease or chronic lung pathology. Without this, you're just guessing - and guessing kills in PH.
Group 2 PH is overdiagnosed because clinicians conflate systolic dysfunction with pulmonary vascular disease. The key is distinguishing pre-capillary from post-capillary PH - and no, echocardiographic TAPSE alone doesn't cut it. You need RV systolic pressure estimation, septal flattening on MRI, and ideally, cardiac output measurement via Fick or thermodilution.
Most primary care providers still treat PH like it's asthma. They give albuterol. They tell patients to lose weight. They miss the fact that this is a vasculopathy, not a ventilatory issue. We need better screening algorithms - maybe even automated AI-based ECG analysis for right axis deviation patterns.
And let's not forget: PAH is not one disease. It's a syndrome with molecular subtypes - BMPR2 mutations, KCNK3 variants, even epigenetic dysregulation. Precision medicine isn't buzzword bingo here - it's survival.
Don't get me started on the FDA's approval pathway for new agents. We still rely on 6MWT as a primary endpoint when we have biomarkers like NT-proBNP and troponin that correlate better with mortality. It's archaic.
Real progress? Riociguat for CTEPH. Sotatercept for PAH. These aren't just drugs - they're paradigm shifts. But access? Forget it. Insurance denies it unless you're dying. That's the real tragedy.
And yes, cyanosis matters. It's not just 'blue fingers.' It's deoxygenated blood pooling because the right ventricle can't push through the stiffened vasculature. That's end-stage. You don't wait for that.
Bottom line: If you're seeing progressive dyspnea with normal spirometry, stop calling it anxiety. Run the echo. Refer to a PH center. Don't let another patient become a statistic because someone didn't know the difference between pulmonary hypertension and pulmonary venous hypertension.
Emanuel Jalba
November 19, 2025 AT 08:32 AMThis is literally life or death and people are still brushing it off like it’s just ‘being out of shape’ 😭
I had a cousin who died at 34 because her doctor said she was ‘just stressed.’ She was climbing stairs and passed out. Three months later, she was on a transplant list. Too late.
STOP MINIMIZING THIS. 🙏🩹
Heidi R
November 20, 2025 AT 07:02 AMGroup 1 PAH is rare, but when it hits, it’s brutal. And most patients are women in their 30s. Coincidence? I think not.
Estrogen metabolism. Endothelial dysfunction. Autoimmune overlap. We’ve known this for 20 years. Yet we still treat it like a generic heart issue.
Someone needs to call out the gender bias in cardiology.
Bailey Sheppard
November 21, 2025 AT 10:26 AMThanks for laying this out so clearly. I’ve seen too many people dismissed for years with ‘it’s just anxiety’ or ‘you’re getting older.’
It’s scary how many red flags are ignored until it’s too late. I hope this post reaches someone who’s been told they’re fine - but know they’re not.
Kristi Joy
November 22, 2025 AT 12:31 PMFor anyone reading this and thinking ‘maybe this is me’ - don’t wait. Write down your symptoms. Track your walk distances. Bring it to your doctor with the WHO classification in hand.
You know your body better than anyone. If something feels wrong, push. Hard.
Hal Nicholas
November 23, 2025 AT 00:08 AMOf course they missed it. The medical system is broken. They’re paid to treat symptoms, not find root causes. Big Pharma doesn’t want you cured - they want you on lifelong meds.
And don’t even get me started on how they ignore Group 5. It’s a dumping ground for everything they don’t understand.
Louie Amour
November 24, 2025 AT 12:20 PMWow. So you’re telling me that a cardiologist who doesn’t know the difference between Group 1 and Group 2 shouldn’t be allowed to practice? That’s not a critique - that’s a public safety issue.
Someone should sue the AMA for not mandating PH training in residency. This is malpractice waiting to happen.
Kristina Williams
November 25, 2025 AT 18:04 PMThey’re hiding something. The government knows PH is linked to certain chemicals in water supplies. That’s why it’s rising in the Midwest. They don’t want you to know. Look up the EPA reports from 2012 - redacted. Coincidence? I think not.
Also, 5G might be making it worse. The radiation stresses the endothelium.
Shilpi Tiwari
November 26, 2025 AT 08:32 AMAs a pulmonology fellow in Mumbai, I see Group 3 PH daily - COPD patients with severe hypoxia, but no one checks their pulmonary pressures until they’re in right heart failure.
Our echocardiography machines are old. We don’t have right heart cath labs in most district hospitals. The gap between WHO guidelines and reality is a canyon.
But we’re starting community screening camps. Small steps. Still, the mortality rate here is 4x higher than in the US. We need global equity in PH care.
Christine Eslinger
November 28, 2025 AT 03:02 AMThere’s something beautiful in how the body tries to compensate - the right ventricle hypertrophies, the heart rate increases, the blood gets shunted - all to keep oxygen flowing. But it’s a temporary fix. Like a car with a failing alternator running on battery power.
What’s tragic isn’t just the diagnosis - it’s how long people suffer before they’re heard.
I’ve sat with patients who cried because they finally had a name for their suffering after five years of being told they were ‘dramatic.’
Knowledge is power. But compassion? That’s what saves lives.
Denny Sucipto
November 28, 2025 AT 05:34 AMMan, I used to think ‘shortness of breath’ was just what happened when you got older or didn’t work out.
Then my sister got diagnosed. She was 29. No smoking. No asthma. Just… tired. Like, bone-deep tired.
She’s on epoprostenol now. It’s a drip. She carries it in a backpack. She still hikes. Still laughs. Still lives.
This isn’t the end. It’s a new beginning. And if you’re reading this and you’re scared - you’re not alone. We’ve got your back.
Brenda Kuter
November 29, 2025 AT 13:33 PMWait - so this is why my neighbor’s daughter died in her sleep at 22? They said it was ‘sudden cardiac arrest.’ But she had blue lips. And she was always tired.
What if they just checked her echo? What if someone had listened?
They’re covering this up. I know it. I’ve seen the reports. The CDC doesn’t want panic. But silence kills.
Shaun Barratt
November 29, 2025 AT 14:27 PMWhile the clinical presentation of pulmonary hypertension is well-documented in the literature, the diagnostic delay remains a persistent issue across multiple healthcare systems. The mean time from symptom onset to diagnosis is approximately 2.8 years in North American cohorts, with significant disparities observed in underserved populations. This delay correlates strongly with increased mortality and diminished functional capacity.
Furthermore, the utilization of echocardiographic parameters such as TAPSE, RV fractional area change, and S’ wave velocity remains inconsistent in primary care settings, contributing to underdiagnosis.
Recommendations for standardized screening protocols in high-risk populations (e.g., connective tissue disease, familial PAH, chronic hypoxia) are warranted.
Iska Ede
November 30, 2025 AT 19:20 PMSo let me get this straight - we have drugs that can extend life by years, but people are still being told they’re ‘just out of shape’?
Wow. The medical system is a sitcom written by someone who hates humanity.
Gabriella Jayne Bosticco
December 2, 2025 AT 07:57 AMI’m a nurse in London. I’ve seen this too many times.
One patient, 41, female, was told she had ‘chronic fatigue syndrome’ for 3 years. Then she collapsed at work. Echo showed RVSP of 72. She’s on treprostinil now.
She said: ‘I just thought I was lazy.’
That’s the worst part.