By age 75, one in three Americans has some form of age-related macular degeneration (AMD). It doesn’t take away your sight completely-but it steals the part you rely on most: your central vision. Reading the clock, recognizing a grandchild’s face, reading the newspaper, even threading a needle-these everyday moments become impossible. AMD is the leading cause of vision loss in people over 65 in the U.S., and it’s not going away. With the population aging, more than 10 million Americans currently live with it, and that number is expected to hit 288 million globally by 2040.
What Exactly Is AMD?
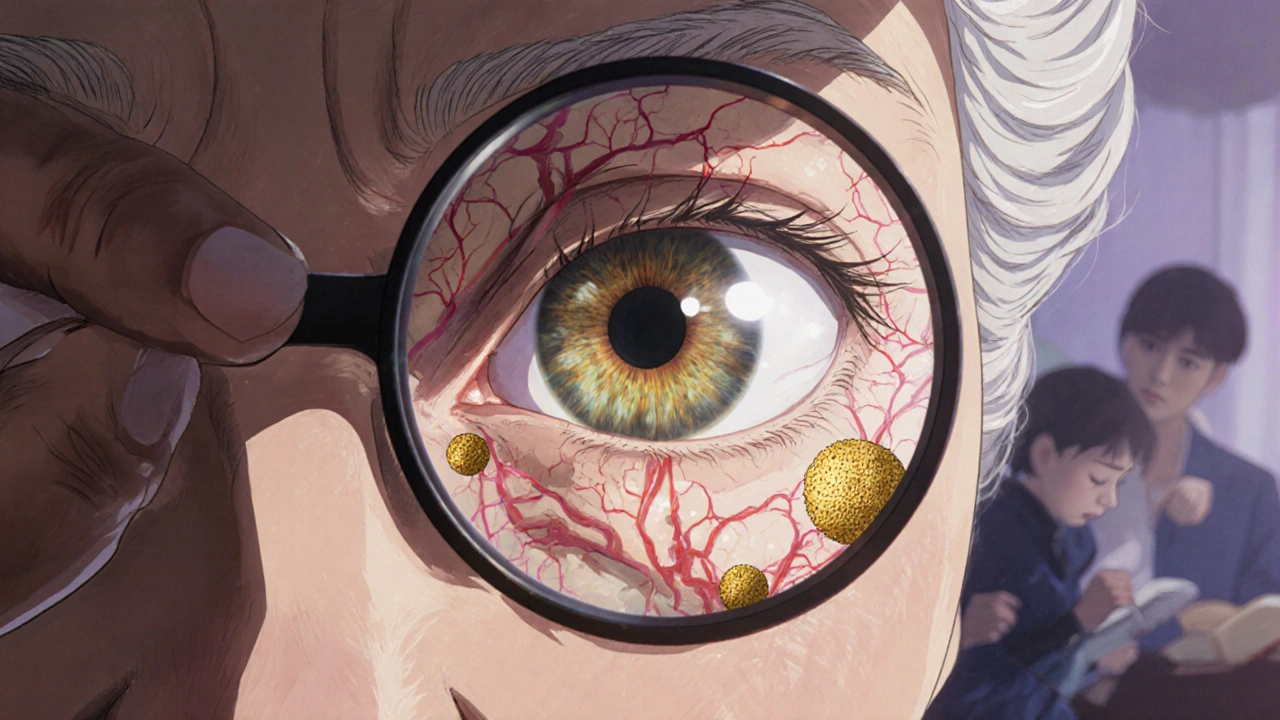
AMD attacks the macula, a tiny spot in the center of your retina packed with light-sensing cells called cones. This is your high-resolution zone-the part of your eye that lets you see fine details, colors, and faces clearly. When the macula breaks down, you lose that sharp central view. Peripheral vision stays intact, so you can still walk around and notice movement, but you can’t focus on what’s right in front of you.
There are two types: dry and wet. Dry AMD is the most common-about 90% of cases. It starts with tiny yellow deposits called drusen building up under the retina. Over time, these cause the retinal tissue to thin and die. This is called geographic atrophy in its advanced stage. It’s slow, often taking years to cause major vision loss.
Wet AMD is the scary one. It makes up only 10-15% of cases, but it’s responsible for 90% of severe vision loss from AMD. Here, abnormal blood vessels grow under the macula from the choroid layer below. These vessels are fragile. They leak fluid and blood, scarring the macula in weeks or months. Once that happens, vision loss can be rapid and permanent.
Here’s the key point: any stage of dry AMD can turn into wet AMD. That’s why regular eye exams are critical. You might not feel any change until it’s too late.
Who’s at Risk?
Age is the biggest factor. Less than 1% of people under 50 have AMD. By age 75, that jumps to 35%. But age isn’t the only thing.
Smoking is the #1 modifiable risk. If you smoke, you’re nearly four times more likely to develop AMD than someone who’s never smoked. Quitting doesn’t erase the risk overnight, but it cuts it in half over time.
Genetics matter too. If a parent or sibling has AMD, your risk jumps 3 to 6 times higher. Certain genes in the complement system-part of your immune response-are strongly linked to AMD. In fact, about half to 70% of AMD risk comes from inherited factors.
Race plays a role. White Americans are 2.5 times more likely to develop AMD than African Americans and 1.8 times more likely than Hispanic or Latino populations. The reasons aren’t fully understood, but differences in eye pigment and genetic variants may contribute.
Other factors? High blood pressure, high cholesterol, and obesity. People with a BMI over 30 have more than double the risk. Poor diet and lack of exercise don’t directly cause AMD, but they make your body more vulnerable to the damage.
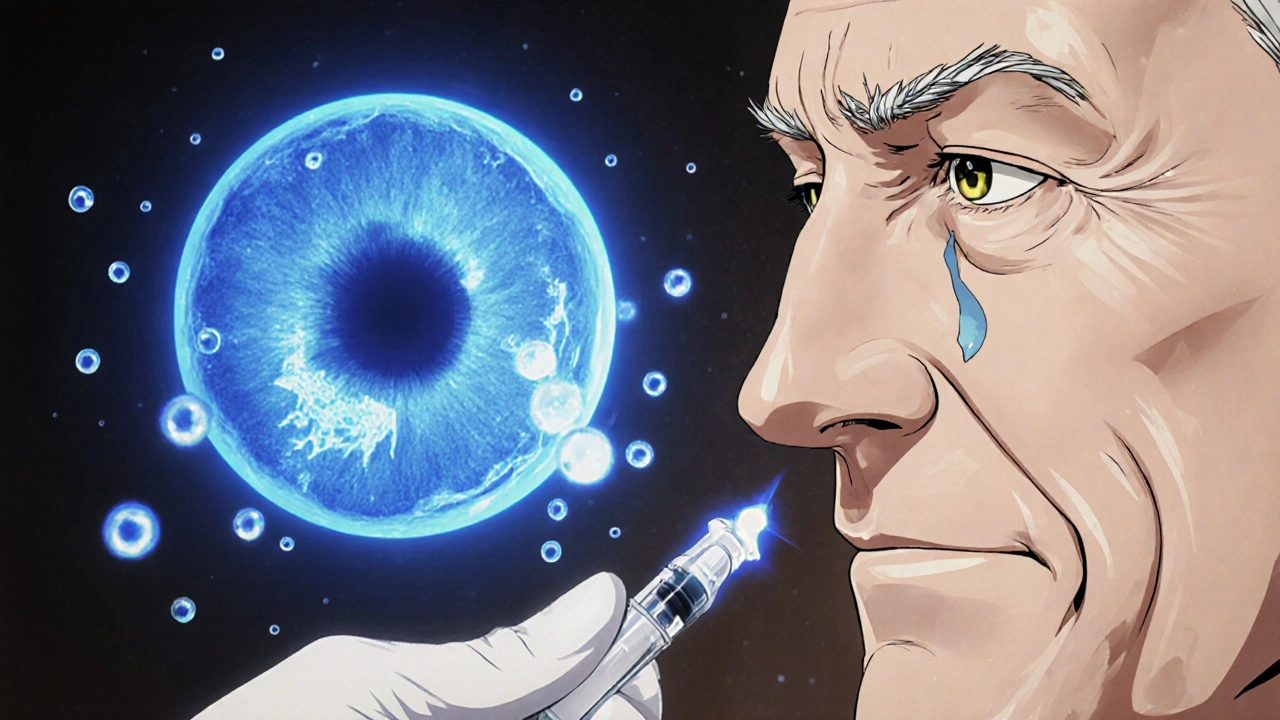
How Anti-VEGF Therapy Stops Wet AMD
Wet AMD is driven by one protein: VEGF-vascular endothelial growth factor. This protein tells your body to grow new blood vessels. In a healthy eye, VEGF is kept in check. In wet AMD, it goes into overdrive, triggering those dangerous, leaky vessels under the macula.
Anti-VEGF drugs block that signal. They’re injected directly into the eye-into the vitreous gel, just behind the pupil. These injections don’t cure AMD. But they stop the bleeding and leaking. In many cases, they even reverse some vision loss.
Think of it like turning off a faucet that’s flooding your basement. The water doesn’t vanish overnight, but the damage stops. That’s what anti-VEGF does. Without treatment, wet AMD can destroy central vision in months. With it, many people stabilize or even gain back some sight.
Studies show that 68% of patients on anti-VEGF therapy report stable or improved vision. One patient on Reddit shared: “After 12 Lucentis injections over 9 months, my vision stabilized at 20/40 from 20/200-worth every uncomfortable moment.” That’s not rare. It’s the norm for those who stick with treatment.
The Burden of Treatment
Anti-VEGF works-but it’s not easy. Most patients start with monthly injections for three months. Then, they move to a “treat-and-extend” or “as-needed” schedule based on scans from an OCT machine (optical coherence tomography), which shows fluid buildup in the retina.
That means clinic visits every 4 to 8 weeks, sometimes more. For older adults, especially those with mobility issues or no transportation, this is a huge burden. A Cleveland Clinic survey found that 82% of patients say frequent visits are their biggest challenge.
Some treatments are getting better. In 2021, the FDA approved Susvimo, a tiny implant that releases ranibizumab (an anti-VEGF drug) continuously for up to six months. It’s surgically placed in the eye and refilled in the doctor’s office. It’s not for everyone, but it’s a major step forward.
Another newer option is Vabysmo, approved in 2022. It blocks two proteins-VEGF and angiopoietin-2-which may mean fewer injections over time. Early data suggests patients can go longer between treatments compared to older drugs.
Still, 92% of U.S. ophthalmologists use anti-VEGF as the first-line treatment for wet AMD today. That’s up from just 15% in 2005, before the first anti-VEGF drug was approved for AMD. The shift happened because the results were undeniable.
What About Dry AMD?
There’s no injection for dry AMD. But there is something that helps: the AREDS2 formula. This isn’t a cure, but a daily supplement proven to reduce the risk of progression to advanced AMD by 25% in people with intermediate dry AMD.
The formula includes:
- Vitamin C (500 mg)
- Vitamin E (400 IU)
- Lutein (10 mg)
- Zeaxanthin (2 mg)
- Zinc (80 mg)
- Copper (2 mg)
It doesn’t contain beta-carotene anymore-that was linked to higher lung cancer risk in smokers. If you have dry AMD, talk to your eye doctor before starting any supplement. Not all “eye vitamins” are the same. Only the AREDS2 formula has the right mix and doses backed by science.
For advanced dry AMD with geographic atrophy, a new drug called Syfovre (pegcetacoplan) was approved in 2023. It slows the growth of atrophy by about 20% over a year. It’s not a cure, but it’s the first treatment ever approved for this stage.

Monitoring at Home
One of the best tools for catching wet AMD early is the Amsler grid. It’s a simple checkerboard pattern you look at with one eye at a time, every day. If straight lines start to look wavy, blurry, or missing, it could mean new fluid is building up under your macula.
Studies show 40% of patients spot changes on the Amsler grid before their next eye exam. That’s huge. Early detection means earlier treatment-and better outcomes.
Keep a notebook. Write down the date and what you see. If something changes, call your eye doctor the same day. Don’t wait.
What’s Next for AMD Treatment?
Researchers are working on ways to make treatment easier and longer-lasting. Gene therapy is one of the most promising. Since half to 70% of AMD risk is genetic, scientists are testing ways to deliver healthy versions of the faulty genes directly into the eye. Early trials are showing safety and some signs of slowing disease progression.
Other ideas? Oral medications that reach the eye, eye drops that deliver anti-VEGF drugs, and even wearable devices that monitor vision changes at home. These are still in testing, but they’re moving fast.
The goal isn’t just to stop vision loss-it’s to restore it. And while we’re not there yet, the progress over the last 20 years has been extraordinary. What used to be a death sentence for central vision is now a manageable condition for most.
Living With AMD
AMD doesn’t have to mean isolation. Low-vision aids-magnifiers, screen readers, high-contrast lighting-can help you keep reading, watching TV, and staying connected. Many community centers and vision rehabilitation programs offer free training.
And don’t underestimate the power of routine. Annual eye exams after 65. Daily Amsler grid checks. Taking your AREDS2 pills. Quitting smoking. Eating leafy greens, fish, and nuts. These aren’t glamorous-but they’re the difference between losing your vision and keeping your life.
AMD is not a death sentence. It’s a challenge. And with the right care, it’s one you can live with.
Can AMD be cured?
No, AMD cannot be cured. But its progression can be slowed-or even reversed in wet AMD-through treatments like anti-VEGF injections. For dry AMD, the AREDS2 supplement reduces the risk of advancing to the more serious forms by 25%. Early detection and consistent care are key to preserving vision.
How often do you need anti-VEGF injections?
Most patients start with monthly injections for three months. After that, the schedule is adjusted based on eye scans (OCT). Many go to every 6 to 8 weeks, and some can stretch to 12 weeks. Newer treatments like Vabysmo and the Susvimo implant aim to reduce how often you need shots.
Is the injection painful?
Most people feel only a slight pressure or pinch. The eye is numbed with drops before the injection. The whole process takes less than a minute. Anxiety is common, but the discomfort is brief. Many patients say the fear is worse than the actual procedure.
Can I prevent AMD if I have a family history?
You can’t change your genes, but you can lower your risk. Don’t smoke. Eat leafy greens, fish, and nuts. Control blood pressure and cholesterol. Get annual eye exams after age 65. If you have intermediate AMD, take the AREDS2 supplement. These steps can delay or prevent vision loss, even with a strong family history.
What happens if I miss an anti-VEGF injection?
Missing injections increases your risk of vision loss. Studies show patients who miss more than 25% of scheduled treatments lose about 30% more vision than those who stick to their plan. If you miss one, call your doctor right away. Don’t wait for your next appointment. Early intervention can still save your sight.
Are there side effects from anti-VEGF injections?
Side effects are rare but possible. The most common are temporary eye redness, floaters, or mild discomfort. Serious risks include infection inside the eye (endophthalmitis), retinal detachment, or increased eye pressure. These happen in less than 1% of injections. The benefits of preserving vision far outweigh the risks for most patients.
Does diet help with AMD?
Yes. Diets rich in lutein and zeaxanthin-found in kale, spinach, broccoli, and eggs-support macular health. Omega-3s from fatty fish like salmon may also help. The AREDS2 supplement is specifically formulated to reduce progression risk. But no food or supplement can replace medical treatment for wet AMD.
Can I still drive with AMD?
It depends on how much vision you’ve lost. Many people with early or moderate AMD can still drive safely, especially with bioptic telescopes or other low-vision aids. But if central vision is severely impaired, driving becomes dangerous. Your eye doctor can help determine if you’re still safe to drive, and state laws vary on minimum vision requirements.









Peter Aultman
November 14, 2025 AT 05:38 AMI've been getting these injections for 3 years now. At first I thought I'd never get used to it, but honestly? The needle pinch is nothing compared to the fear of going blind. My grandkids can finally see me smile again.
Just keep showing up. It's a grind, but worth every second.
Barry Sanders
November 14, 2025 AT 16:40 PMThis whole anti-VEGF thing is just Big Pharma's golden goose. They're milking old people for monthly cash grabs while pushing expensive implants nobody can afford.
Joe Goodrow
November 16, 2025 AT 10:56 AMYou people act like this is some new scam. My dad had AMD, went blind in 6 months before these injections existed. Now my mom gets them every 6 weeks and she's still reading the newspaper. If you're complaining about clinic visits, you're not thinking about what happens when you don't go.
Sean Evans
November 17, 2025 AT 14:50 PMLOL imagine being so old you need a needle in your eyeball just to see your own face 😂
Why don't you just accept nature? 🤷♂️
Sean Hwang
November 18, 2025 AT 13:36 PMI work in a clinic and see this every day. People think the shots are scary, but the real horror is waiting too long. One guy missed 4 months, came back with a hemorrhage. We saved his sight, but he lost 20/40 vision he had before. Don't be that guy. Keep your appointments.
Scarlett Walker
November 18, 2025 AT 14:21 PMMy mom started taking AREDS2 after her diagnosis and honestly? She says her vision feels clearer already. Not magic, but she's got hope. And that matters more than you think.
Anjan Patel
November 20, 2025 AT 03:35 AMI'm from India and we don't have access to half this stuff. My uncle went blind because the nearest specialist was 400 miles away. This post feels like a luxury for rich Americans. What about the rest of the world?
kshitij pandey
November 20, 2025 AT 15:21 PMI'm from India too and I want to say this: in my village, we use turmeric and warm oil massages for eye health. Not science, but it brings comfort. And we teach our elders to look at the sun at dawn - not to stare, but to feel the light. Maybe we don't have drugs, but we have tradition. And love. That matters too.
Brittany C
November 22, 2025 AT 14:07 PMThe OCT monitoring protocol is critical for treatment optimization. Subretinal fluid dynamics are highly variable between individuals, and the treat-and-extend paradigm has demonstrated superior long-term visual acuity outcomes compared to fixed dosing regimens in multiple multicenter trials.
Chris Ashley
November 24, 2025 AT 01:20 AMHey, I just got my first injection yesterday. I was terrified. But the nurse held my hand and said, 'You're stronger than this fear.' I cried. Then I laughed. And now I'm gonna go get my AREDS2 pills. Thanks for this post. It helped.