Imagine waking up in the middle of a conversation, only to find your knees buckling and your arms dropping to your sides-completely awake, but unable to move. That’s cataplexy. For people with narcolepsy type 1, it’s not a rare oddity. It’s a daily reality. And it’s not just about being tired. It’s about your brain losing control of the boundaries between sleep and wakefulness, triggered by laughter, anger, or even surprise. This isn’t just sleepiness. It’s a neurological disorder with a clear biological root: the loss of hypocretin-producing neurons in the brain. And there’s one treatment that doesn’t just manage symptoms-it rewires the sleep-wake cycle in a way nothing else can: sodium oxybate.
What Narcolepsy with Cataplexy Really Looks Like
Narcolepsy with cataplexy, officially called narcolepsy type 1, isn’t just about falling asleep at random times. It’s a five-part syndrome: excessive daytime sleepiness, sudden muscle weakness (cataplexy), sleep paralysis, vivid hallucinations when falling asleep or waking up, and broken nighttime sleep. Of these, cataplexy is the fingerprint of the disease. It’s not fainting. It’s not a seizure. It’s a sudden, brief loss of muscle tone-your head drops, your jaw goes slack, your legs give out-while you’re fully aware. Episodes last seconds to a few minutes. They can be mild, like a drooping eyelid, or severe, causing a full collapse.
People often dismiss these episodes. A 2022 survey by the Narcolepsy Network found that 42% of patients first thought their cataplexy was just dizziness or weakness. One man in Seattle told his doctor he was having panic attacks-until he realized the episodes only happened when he laughed at his kid’s jokes. That’s the hallmark: emotion triggers it. Joy, anger, surprise. Not stress alone. Not fatigue. Specific emotional spikes.
It usually starts between ages 10 and 30. But diagnosis? That takes years. On average, 8.7 years. Why? Because doctors don’t ask the right questions. Patients don’t know what to call it. And sleep specialists are few and far between. In the U.S., only 40% of sleep centers can run the full diagnostic test. That means most people are misdiagnosed-first with depression, then with anxiety, then with sleep apnea.
How Doctors Diagnose It (And Why It’s So Hard)
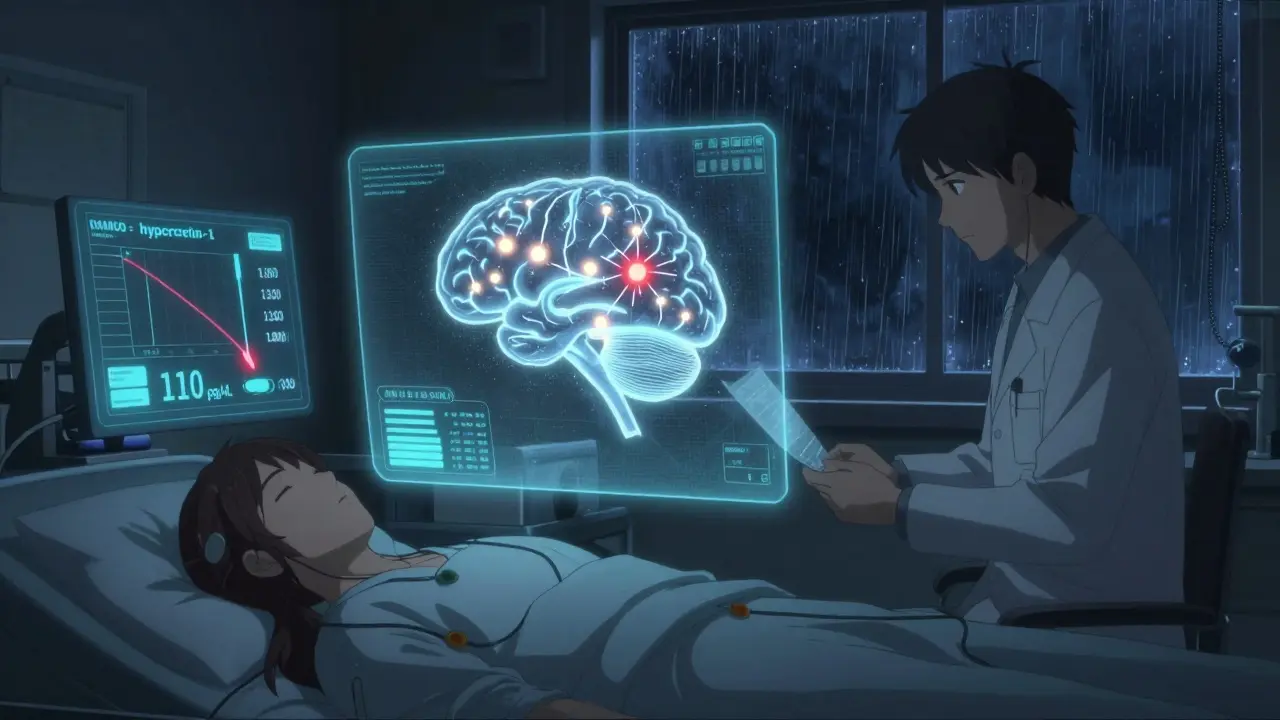
There are two main ways to confirm narcolepsy type 1: the Multiple Sleep Latency Test (MSLT) and the cerebrospinal fluid (CSF) hypocretin-1 test. Both are needed for certainty, but they’re not equally accessible.
The MSLT requires an overnight sleep study first-polysomnography-then four to five naps the next day, spaced two hours apart. You’re hooked up to sensors, asked to lie still and try to fall asleep. The test measures how fast you fall asleep and whether you enter REM sleep right away. If you hit REM within 15 minutes during two or more naps, that’s a SOREMP-sleep-onset REM period. Two SOREMPs, plus daytime sleepiness lasting at least three months, meets diagnostic criteria. But here’s the catch: sleep deprivation, medications, or even a bad night’s sleep can throw off the results. Up to 10% of healthy people show false positives.
The CSF test is more direct. It measures hypocretin-1, a brain chemical that keeps you awake and regulates muscle tone during REM sleep. In narcolepsy type 1, these neurons are destroyed. The result? Hypocretin-1 levels drop below 110 pg/mL. This test is 98% sensitive and 99% specific. If your levels are that low, you have narcolepsy type 1. No doubt. But it requires a lumbar puncture-a spinal tap. That’s uncomfortable. And it carries a 10-30% risk of post-dural headache, which can last days.
That’s why some experts, like Dr. Michael Thorpy, argue that if cataplexy is clear and HLA-DQB1*06:02 (a genetic marker found in 90-95% of patients) is positive, you might not even need the MSLT. But most insurance companies still require the sleep study. And many doctors don’t know to order the CSF test at all.
Why Sodium Oxybate Is the Only Treatment That Works for Cataplexy
There are other drugs for narcolepsy: modafinil for sleepiness, pitolisant for wakefulness, solriamfetol to reduce daytime fatigue. But none of them touch cataplexy. Not even close.
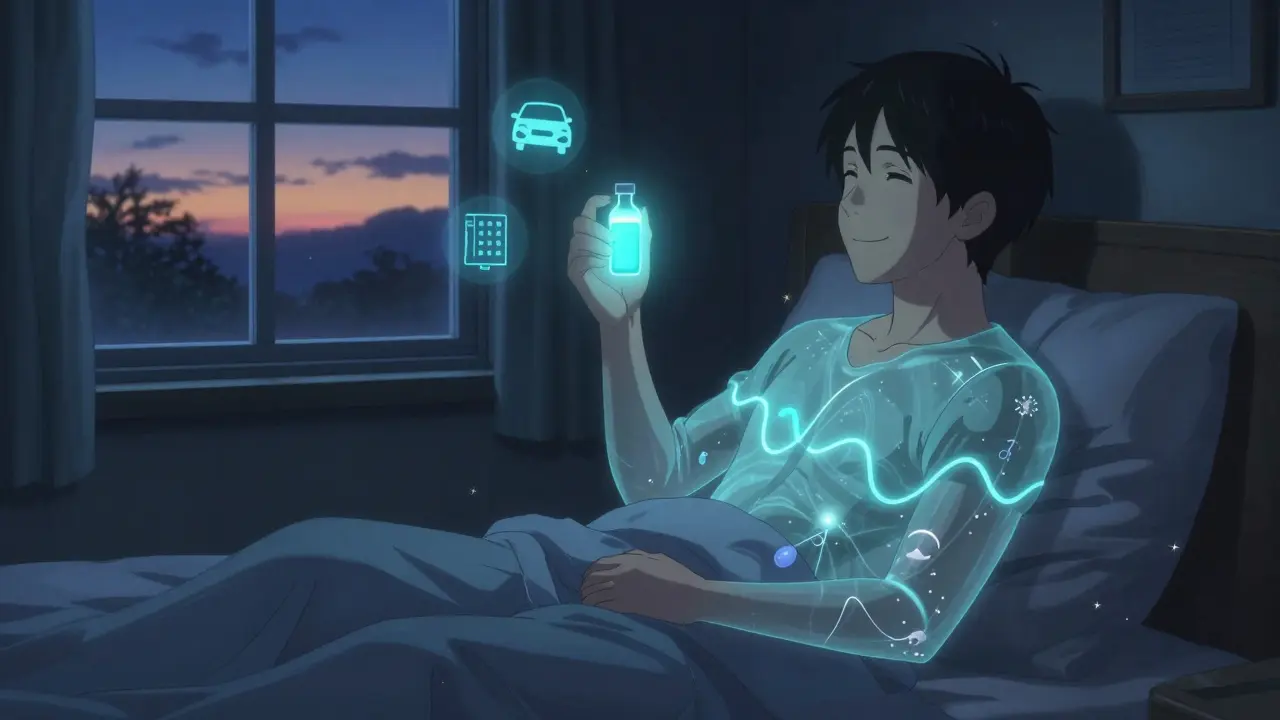
Sodium oxybate-the active ingredient in Xyrem and Xywav-is the only medication approved by the FDA specifically for treating cataplexy in narcolepsy type 1. It’s also the only one that improves both excessive daytime sleepiness and cataplexy at the same time. How? It’s a version of gamma-hydroxybutyrate (GHB), a naturally occurring brain chemical that’s converted from GABA. At night, it promotes deep, restorative sleep, especially slow-wave sleep. That’s key. People with narcolepsy don’t get enough deep sleep. Sodium oxybate fixes that. And by stabilizing sleep architecture, it reduces the brain’s tendency to slip into REM sleep at the wrong times-preventing cataplexy, hallucinations, and sleep paralysis.
Real-world data from PatientsLikeMe shows that 85% of users see a dramatic drop in cataplexy-from seven episodes a week down to just 1.2. That’s not a slight improvement. That’s life-changing. People go back to driving. They return to work. They laugh again without fear.
But it’s not simple. Sodium oxybate comes as a liquid you drink. And you have to take it twice a night: once at bedtime, and again 2.5 to 4 hours later. That means waking up in the middle of the night to take a second dose. Sixty-five percent of patients say this is the hardest part. Missing a dose? Cataplexy can come roaring back.
The Hidden Costs and Barriers to Getting It
Even if you’re diagnosed, getting sodium oxybate isn’t easy. Xyrem costs $10,000 to $15,000 a month before insurance. Xywav, the newer version with less sodium, is slightly cheaper but still runs $8,000-$12,000. Insurance rarely covers it without a fight. In 2023, 92% of U.S. patients needed prior authorization. And 28% of those were denied at least once.
There’s also the REMS program-Risk Evaluation and Mitigation Strategy. Because GHB has a history of abuse, the FDA requires doctors to be specially certified to prescribe it. Pharmacies must be certified to dispense it. And you can’t get it from your local pharmacy. It’s shipped directly from a single centralized pharmacy. That adds delays. One patient in Portland waited six weeks between her diagnosis and her first bottle.
Side effects are real too. Nausea affects 38%. Dizziness, 29%. Enuresis (bedwetting), 12%. Most improve after a few weeks. But some patients can’t tolerate it. And for 12% of users, the medication doesn’t work at all-often because they’re misdiagnosed.
What’s Coming Next
The future is promising. In July 2023, Xywav was approved for children as young as 7. That’s huge. Kids with cataplexy can now get the only treatment that actually stops their episodes.
And then there’s FT001-a new version of sodium oxybate designed to be taken just once at night. Phase 3 trials showed it works just as well as Xyrem, without the midnight dose. If approved, it could double adherence rates.
Even more exciting? Oral hypocretin receptor agonists. Takeda’s TAK-994 showed a 92% drop in cataplexy in early trials. It’s not available yet-development paused due to liver safety concerns-but it proves the concept: replacing the missing brain chemical might be the real cure.
Meanwhile, the next version of the diagnostic guide (ICSD-4), expected in late 2024, will lower the CSF hypocretin-1 threshold from 110 to 80 pg/mL. That means more people will be correctly diagnosed earlier. And better tools are being developed to quantify cataplexy-like wearable sensors that detect muscle tone drops.
What to Do If You Suspect Narcolepsy with Cataplexy
If you or someone you know has unexplained daytime sleepiness plus emotional muscle weakness, don’t wait. Start here:
- Keep a sleep diary for two weeks. Note when you feel sleepy, when you nap, and if you ever collapse during strong emotions.
- Take the Epworth Sleepiness Scale. Score above 10? That’s abnormal.
- Find a sleep specialist-not a general neurologist or primary care doctor. Use the American Academy of Sleep Medicine’s directory.
- Ask for both an overnight polysomnography and a CSF hypocretin-1 test. Don’t settle for MSLT alone if cataplexy is present.
- If diagnosed, ask about sodium oxybate. Request Xywav if you’re on a low-sodium diet or have high blood pressure.
- Enroll in the REMS program early. It takes time to get certified.
This isn’t a condition you can outgrow. But with the right diagnosis and treatment, it’s manageable. You don’t have to live in fear of laughing too hard. You don’t have to quit your job because you can’t stay awake. Sodium oxybate isn’t perfect. But it’s the closest thing we have to a cure for the core problem-and for many, it’s the difference between isolation and living again.
Is narcolepsy with cataplexy the same as just being tired?
No. Normal tiredness fades with rest. Narcolepsy with cataplexy is a neurological disorder caused by the loss of brain cells that produce hypocretin. It causes sudden muscle weakness triggered by emotions, uncontrollable sleep attacks, and disrupted nighttime sleep-even after a full night’s rest. You can’t fix it with caffeine or more sleep.
Can you outgrow narcolepsy with cataplexy?
No. Narcolepsy type 1 is a lifelong condition. The brain cells that make hypocretin don’t regenerate. But symptoms can be controlled. With sodium oxybate, many people experience near-complete relief from cataplexy and improved daytime alertness. While the condition doesn’t go away, your quality of life can improve dramatically.
Why is sodium oxybate the only drug that treats cataplexy?
Because it’s the only medication that restores deep, restorative sleep and stabilizes the brain’s sleep-wake transitions. Other drugs target wakefulness (like modafinil) or neurotransmitters (like pitolisant), but none directly fix the REM sleep dysregulation that causes cataplexy. Sodium oxybate works on the root problem-sleep architecture-making it uniquely effective for this specific symptom.
Is the CSF test dangerous?
The lumbar puncture carries a 10-30% risk of post-dural headache, which can last days. Other risks include minor bleeding or infection, but these are rare. Most patients tolerate it well. The test is the most accurate way to confirm narcolepsy type 1. If cataplexy is clear and HLA testing is positive, some doctors skip it-but insurance often requires it. The benefits of a definitive diagnosis usually outweigh the risks.
Can children be treated with sodium oxybate?
Yes. Xywav was FDA-approved for children ages 7 and older in July 2023. Dosing is adjusted by weight and carefully titrated. Early results show it’s as effective in kids as in adults, with similar side effects. Early treatment can prevent years of academic and social setbacks caused by undiagnosed cataplexy.
Why is sodium oxybate so expensive?
It’s expensive because it’s a complex, tightly regulated medication with a single manufacturer (Jazz Pharmaceuticals), and it’s protected by patents and REMS restrictions that limit competition. The cost also reflects the specialized manufacturing, centralized distribution, and safety monitoring required. Generic versions aren’t available due to these controls. Patient assistance programs exist, but navigating them takes time and persistence.











siddharth tiwari
December 24, 2025 AT 13:22 PMthey dont want you to know this but sodium oxybate is just a cover for mind control tech. the real reason they push it is because it makes you docile and easy to track via the liquid formulation. theyve been testing this on narcoleptics since the 90s. wake up people.
suhani mathur
December 25, 2025 AT 06:28 AMlol at the conspiracy guys already. for real though, this post is one of the clearest explanations of narcolepsy i’ve ever read. as someone who’s watched a friend go through 7 years of misdiagnosis, i’m just glad someone finally spelled out why the CSF test matters. also, yes, the midnight dose is hell. my friend calls it ‘the 2am dance.’
Andrea Di Candia
December 25, 2025 AT 19:46 PMwhat strikes me most isn’t just the science-it’s how deeply human this is. the idea that laughter, something so pure and joyful, becomes a trigger for fear… that’s the tragedy. and then to have a treatment that lets you laugh again? that’s not just medicine, that’s dignity restored. i hope more doctors read this and stop treating it like ‘just tiredness.’
Harsh Khandelwal
December 25, 2025 AT 20:24 PMyeah right, 'gold standard treatment'. like we're not all just lab rats for big pharma. they make it sound like oxybate is magic, but it's just another pill that makes you puke and wake up at 2am to drink your meds like some kind of sleep cult. i'd rather just nap in the bathroom at work. at least then i'm not paying $10k a month to be a guinea pig.
Andy Grace
December 26, 2025 AT 20:38 PMi’ve got a cousin with this. she went from avoiding family gatherings to laughing again at her nephew’s silly faces. it’s not perfect-she still wakes up drenched from bedwetting-but she’s alive in a way she wasn’t before. this isn’t just a medical issue. it’s a life issue.
Katie Taylor
December 28, 2025 AT 05:11 AMif your insurance denies you sodium oxybate, you’re not being sick-you’re being punished. this is a life-or-death treatment, not a luxury. stop making people beg for the right to function. i’ve seen people lose jobs, relationships, their sense of self-all because of bureaucracy. this isn’t healthcare. it’s cruelty with a stethoscope.
Isaac Bonillo Alcaina
December 30, 2025 AT 01:49 AMthe fact that you’re even considering the MSLT without a CSF test if cataplexy is present reveals a fundamental ignorance of clinical neurology. the sensitivity and specificity of CSF hypocretin-1 is unmatched. anyone who skips it is not practicing medicine-they’re gambling with diagnostic accuracy. also, the REMS program exists for a reason: GHB is not candy. stop romanticizing it.
Bhargav Patel
December 31, 2025 AT 14:48 PMthe philosophical underpinning of this condition reveals a profound truth: human consciousness is not a monolith, but a fragile equilibrium maintained by biochemical precision. the loss of hypocretin neurons is not merely a physiological anomaly-it is the dissolution of a boundary between states that defines our very experience of being awake. sodium oxybate, in its imperfect form, attempts to restore this boundary-not by force, but by harmony. it is not a cure, but a reconciliation. and in this reconciliation lies not only symptom relief, but the quiet restoration of the self.