Tuberculosis‑HIV co‑infection is a medical condition where a person simultaneously suffers from active tuberculosis (TB) and HIV/AIDS, leading to heightened disease severity and mortality. The dual burden accounts for nearly one‑third of global TB deaths, according to the World Health Organization (WHO). Understanding why these two infections feed off each other is essential for clinicians, public‑health planners, and anyone caring for affected families.
Why HIV Makes Tuberculosis Lethal
HIV attacks CD4+ T cells (a type of white blood cell that coordinates immune responses). When CD4 counts drop below 200 cells/µL, the immune system loses the ability to contain Mycobacterium tuberculosis (the bacterium that causes TB). This creates a perfect storm: the bacterium proliferates unchecked, and the body cannot mount an effective granuloma response.
Statistics from a 2023 WHO report show that people living with HIV are 18‑times more likely to develop active TB than HIV‑negative individuals. The risk spikes in the first six months after HIV infection, when viral replication peaks and CD4 depletion accelerates.
How TB Accelerates HIV Progression
Active TB triggers chronic inflammation, raising levels of cytokines such as TNF‑α and IL‑6. These molecules can increase HIV replication by activating the viral transcription factor NF‑κB. Clinical studies from Kenya and South Africa documented that TB‑co‑infected patients experience a faster decline in CD4 count-averaging a loss of 50 cells/µL per year compared to 30 cells/µL in HIV‑only patients.
Another key player is the phenomenon of “immune reconstitution inflammatory syndrome” (IRIS). When antiretroviral therapy (ART) restores immune competence, the revived immune system may overreact to dormant TB lesions, causing severe tissue damage. IRIS occurs in roughly 15‑20% of co‑infected patients who start ART within two weeks of TB treatment.
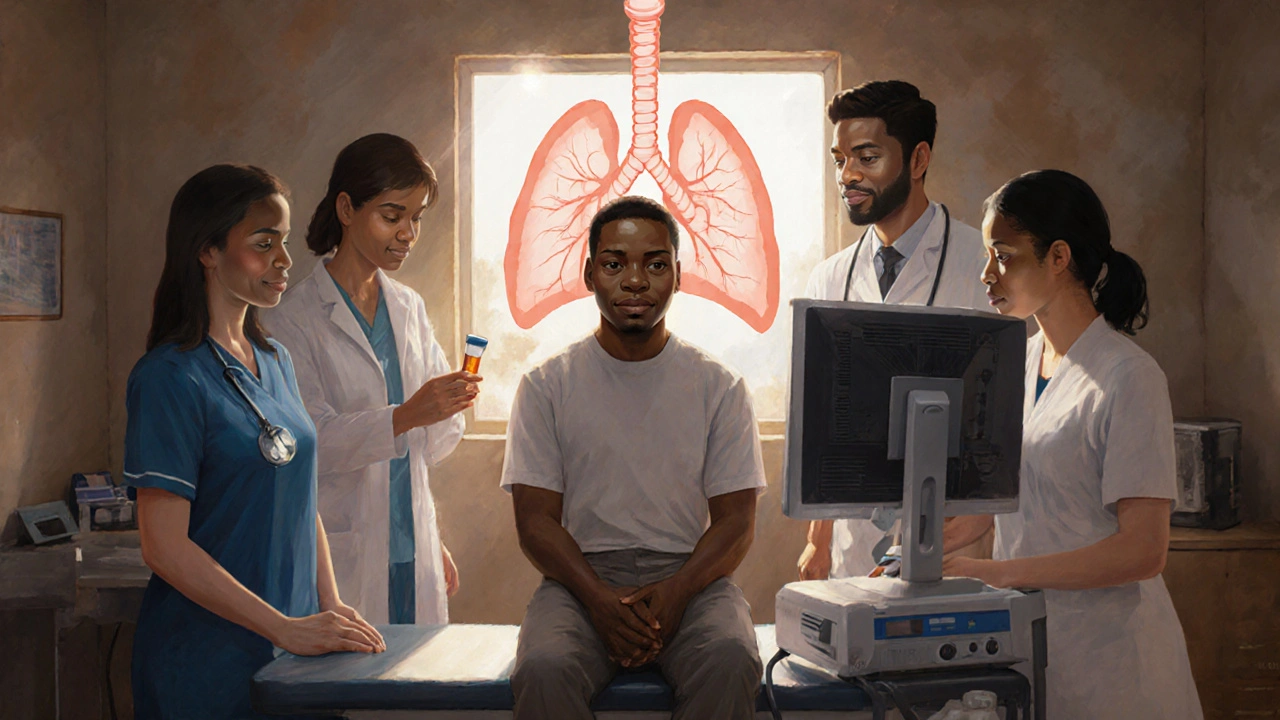
Clinical Picture of Co‑infection
Symptoms often overlap: persistent cough, night sweats, fever, and weight loss appear in both diseases. However, co‑infected patients tend to present with more diffuse lung infiltrates, higher bacteriological load, and extra‑pulmonary manifestations (e.g., meningitis, pericarditis). Mortality data illustrate the gravity-WHO estimates a 20‑30% case‑fatality rate for untreated co‑infection versus <5% for TB alone.
Key clinical markers to watch for include:
- CD4 count < 200 cells/µL
- Positive sputum smear or GeneXpert MTB/RIF test
- Elevated viral load (>100,000 copies/mL) indicating uncontrolled HIV
Diagnosis and Screening Strategies
Early identification hinges on integrated screening. The WHO recommends that every person diagnosed with HIV be screened for TB symptoms at each clinic visit, and vice‑versa. Tools include:
- GeneXpert MTB/RIF (a rapid molecular test that detects TB DNA and rifampicin resistance)
- Chest radiography, interpreted with AI‑assisted algorithms to spot atypical patterns in immunocompromised hosts
- CD4 count and viral load assessment to gauge immune status
For pregnant women living with HIV, sputum induction and urine lipoarabinomannan (LAM) testing have shown higher sensitivity, helping catch TB before it spreads.
Treatment: Balancing Two Complex Regimens
Standard TB therapy (the “short‑course” regimen) consists of isoniazid, rifampicin, pyrazinamide, and ethambutol for two months, followed by isoniazid and rifampicin for four months. Meanwhile, antiretroviral therapy (ART) (a combination of drugs that suppress HIV replication) is life‑saving.
The major drug‑interaction challenge is rifampicin’s induction of cytochromeP450 enzymes, which can lower plasma levels of certain ART agents (e.g., protease inhibitors). Preferred strategies include:
- Starting ART within two weeks of TB therapy for patients with CD4 < 50 cells/µL (to reduce mortality)
- Using efavirenz‑based ART, which tolerates rifampicin
- Switching to dolutegravir once patients stabilize, as recent studies show safe co‑administration
For drug‑resistant TB (MDR‑TB), the regimen expands to include fluoroquinolones and newer agents like bedaquiline. Co‑administration with ART demands close therapeutic drug monitoring to avoid additive toxicity (e.g., peripheral neuropathy from linezolid plus zidovudine).

Public‑Health Response and WHO Guidelines
The WHO’s End TB Strategy (aiming to reduce TB deaths by 95% by 2035) places integrated TB‑HIV services at its core. Key policy pillars are:
- Universal HIV testing for all TB patients and vice‑versa
- Implementation of directly observed therapy (DOT) to improve adherence alongside ART adherence counseling
- Scaling up preventive therapy: a six‑month course of isoniazid (IPT) for HIV‑positive individuals without active TB reduces incidence by up to 33%
Funding gaps remain a hurdle. In 2022, donor contributions covered only 65% of the estimated $28billion needed for global TB‑HIV programs. Advocacy groups argue that integrating services into existing HIV clinics can cut costs by 20%.
Emerging Challenges: Drug Resistance and the COVID‑19 Era
Multi‑drug‑resistant TB (MDR‑TB) is on the rise in sub‑Saharan Africa, partly due to interrupted treatment during the COVID‑19 pandemic. A 2024 meta‑analysis reported a 12% increase in MDR‑TB incidence among HIV‑positive patients compared to pre‑pandemic levels.
COVID‑19 also compounded diagnostic delays: lockdowns reduced clinic visits, and overlapping respiratory symptoms led to misdiagnosis. Programs that adopted tele‑health triage and community‑based sputum collection managed to keep co‑infection detection rates stable.
Related Concepts and Further Reading
Understanding TB‑HIV co‑infection opens doors to exploring several adjacent topics, such as:
- Immune reconstitution inflammatory syndrome (IRIS)
- Latent TB infection (LTBI) screening in people living with HIV
- Impact of nutritional supplementation on treatment outcomes
- Role of rapid molecular diagnostics in low‑resource settings
Each of these areas deepens the picture of how infectious diseases intersect with immune health and health‑system resilience.
Quick Reference Comparison
| Attribute | Tuberculosis (TB) | HIV/AIDS |
|---|---|---|
| Cause | Mycobacterium tuberculosis (bacterium) | Human Immunodeficiency Virus (retrovirus) |
| Transmission | Airborne droplets | Blood, sexual fluids, mother‑to‑child |
| Incubation period | Weeks to months (latent phase possible) | Weeks (acute infection) to years (AIDS) |
| Primary treatment | 6‑month antibiotic regimen (HRZE) | Life‑long antiretroviral therapy (ART) |
| Effect on immune system | Can cause granuloma formation; immune evasion | CD4+ T‑cell depletion, systemic immunosuppression |
Next Steps for Clinicians and Policy Makers
If you’re a clinician, embed routine TB screening into every HIV visit, and vice‑versa. Use rapid molecular tests like GeneXpert to cut diagnostic lag. For policy makers, earmark funds for integrated supply chains-ensuring ART and TB drugs arrive together reduces stock‑outs.
Finally, keep an eye on emerging data. The 2025 WHO update on TB‑HIV co‑infection is expected to refine recommendations around dolutegravir use and shorter MDR‑TB regimens. Staying current saves lives.

Frequently Asked Questions
Why are people with HIV more likely to develop active TB?
HIV destroys CD4+ T cells, which are essential for containing the dormant Mycobacterium tuberculosis. Without enough CD4 cells, the immune system cannot form effective granulomas, allowing latent TB to become active.
Can TB treatment cure HIV?
No. TB antibiotics target the bacterium and have no effect on the virus. However, successful TB treatment reduces inflammation and may slow HIV progression, while ART is needed to control HIV.
What is the best timing to start ART in a TB‑HIV co‑infected patient?
If the CD4 count is below 50 cells/µL, start ART within two weeks of TB therapy to lower mortality. For higher CD4 counts, initiating ART after the intensive TB phase (2weeks) balances efficacy and reduces the risk of IRIS.
How does rifampicin affect HIV medication?
Rifampicin induces liver enzymes that lower the levels of several antiretrovirals, especially protease inhibitors and some non‑nucleoside reverse transcriptase inhibitors. Using efavirenz‑based regimens or adjusting doses of newer agents like dolutegravir avoids this interaction.
What preventive measures exist for people living with HIV?
Isoniazid preventive therapy (IPT) for six months is recommended for HIV‑positive individuals without active TB. Additionally, vaccinating against TB (BCG) where appropriate, maintaining ART adherence, and regular TB screening are key strategies.








michael klinger
September 26, 2025 AT 19:05 PMIt’s no coincidence that the same shadowy agencies pushing vaccine mandates also control the flow of TB‑HIV data, ensuring the public remains clueless about the true scale of the crisis.
Matt Laferty
October 3, 2025 AT 18:46 PMThe interplay between tuberculosis and HIV is a textbook example of how one pathogen can exploit the immunological vacuum created by another, leading to a cascade of clinical complications that are both predictable and devastating. When HIV depletes CD4+ T cells, the host loses the critical cellular scaffolding needed to wall off Mycobacterium tuberculosis, allowing the bacilli to proliferate unchecked. This unchecked growth not only increases bacterial load but also heightens the risk of dissemination to extrapulmonary sites such as the meninges and pericardium. On the flip side, active TB fuels chronic immune activation, releasing cytokines like TNF‑α and IL‑6 that inadvertently drive HIV transcription via NF‑κB pathways, accelerating viral replication. The resultant synergy shortens the window for effective ART intervention, often forcing clinicians to start antiretroviral therapy within a narrow two‑week period to curb mortality. However, initiating ART too early can precipitate immune reconstitution inflammatory syndrome (IRIS), where the recovering immune system launches an aggressive assault on residual mycobacterial antigens, causing severe tissue damage. Managing IRIS requires a delicate balance of corticosteroids and continued antimicrobial therapy, underscoring the importance of integrated care models. Diagnostic algorithms now recommend universal screening: every person diagnosed with HIV should be evaluated for TB symptoms at each visit, and vice‑versa. Molecular platforms like GeneXpert have revolutionized detection, offering rapid identification of TB DNA alongside rifampicin resistance, while urinary LAM tests provide a useful adjunct in advanced HIV disease. Treatment regimens must also navigate drug‑drug interactions; rifampicin induces CYP450 enzymes, lowering concentrations of many antiretrovirals, which is why efavirenz‑based ART remains the cornerstone in co‑infected patients. For those with multidrug‑resistant TB, newer agents such as bedaquiline and linezolid demand vigilant therapeutic drug monitoring to avoid additive toxicities. Public‑health strategies emphasize preventive therapy, with six months of isoniazid markedly reducing incident TB in HIV‑positive cohorts. Funding constraints, however, continue to hamper scale‑up, as donor contributions cover barely two‑thirds of the estimated global needs. The COVID‑19 pandemic further complicated matters, disrupting treatment continuity and amplifying MDR‑TB rates, especially in sub‑Saharan Africa. Telehealth initiatives and community‑based sputum collection have shown promise in maintaining diagnostic yields despite lockdowns. Ultimately, staying abreast of evolving WHO guidelines-particularly the anticipated 2025 updates on dolutegravir co‑administration-will be crucial for clinicians aiming to outpace this deadly partnership.
Genie Herron
October 10, 2025 AT 18:50 PMIt just hits me how heartbreaking this is.
Danielle Spence
October 17, 2025 AT 18:53 PMWe cannot sit idly by while the world allows a preventable syndemic to ravage vulnerable communities; the moral imperative is clear-universal screening and prophylaxis must become non‑negotiable standards of care.
Dhanu Sharma
October 24, 2025 AT 18:56 PMyeah the data pretty much says what it says – if you’re HIV+ get tested for TB and if you have TB get checked for HIV
simple as that.
Edward Webb
October 31, 2025 AT 18:00 PMFrom an ethical standpoint, the integration of TB and HIV services reflects a respect for patient autonomy, ensuring that individuals receive comprehensive care without the burden of navigating fragmented systems.
Snehal Suhane
November 7, 2025 AT 18:03 PMHonestly, if you read the WHO guidelines once you’ll realize the “big pharma” narrative is just a smokescreen for their profit‑driven agenda…
Ernie Rogers
November 14, 2025 AT 18:06 PMOnly in the US do we have the resources to even think about tackling TB‑HIV together, the rest of the world is just winging it.
Eunice Suess
November 21, 2025 AT 18:10 PMThere’s a typo in "countrys" and "definately" – please proofread before posting.
Anoop Choradia
November 28, 2025 AT 18:13 PMOne must consider that covert funding streams from undisclosed entities may subtly dictate which diagnostic tools are promoted, thereby shaping epidemiological outcomes to serve hidden interests.
bhavani pitta
December 5, 2025 AT 18:16 PMWhile many applaud the WHO’s recommendations, I contend that the emphasis on rapid molecular testing overlooks the nuanced socio‑cultural barriers that impede true adoption in rural settings.
Brenda Taylor
December 12, 2025 AT 18:20 PM🙄 this post is way too clinical, we need real stories from patients, not just stats lol
Taryn Thompson
December 19, 2025 AT 18:23 PMFor clinicians, it is essential to note that efavirenz‑based ART remains the preferred regimen in the presence of rifampicin due to its minimal pharmacokinetic interaction, simplifying the co‑treatment algorithm.
Lisa Lower
December 26, 2025 AT 18:26 PMHey team, let’s keep the momentum going!
Remember that early TB screening saves lives, especially in people living with HIV.
Stick to the protocol: symptom check at every visit, GeneXpert when possible, and never skip the isoniazid preventive therapy if the patient is eligible.
Together we can push down that case‑fatality rate – stay focused and keep supporting each other!
Dana Sellers
January 2, 2026 AT 18:30 PMIt’s just plain wrong to ignore the moral duty we have to protect the most vulnerable from this deadly combo of diseases.
nathaniel stewart
January 9, 2026 AT 18:33 PMStay hopeful – advances in dolutegravir co‑administration are already showing promising reductions in mortality rates.
Pathan Jahidkhan
January 16, 2026 AT 18:36 PMOne could argue that the entire discourse is a performance, a staged drama where the true actors are the funding bodies, and we are merely the audience watching a tragic play unfold.
Dustin Hardage
January 23, 2026 AT 18:40 PMIn practice, therapeutic drug monitoring becomes indispensable when combining linezolid with zidovudine, as overlapping hematologic toxicity can precipitate severe anemia if not carefully managed.
Dawson Turcott
January 30, 2026 AT 18:43 PMlol good luck finding a clinic that actually follows those guidelines 😂
Alex Jhonson
February 6, 2026 AT 18:46 PMLet’s celebrate the diversity of approaches across regions – each cultural insight adds a valuable layer to our collective understanding of TB‑HIV co‑infection.