Heartburn Trigger Calculator
Enter your medication type, spicy food tolerance, and meal timing to calculate your personalized safe medication window. Based on NIH and FDA research.
Your Safe Medication Window
30-60 minutes before your next meal
Your heartburn risk is low with current inputs.
Why this timing?
Taking medications before stomach acid production peaks (30-60 minutes before meals) maximizes effectiveness. Spicy foods can reduce PPI absorption by 18-23% when taken within 2 hours of triggers.
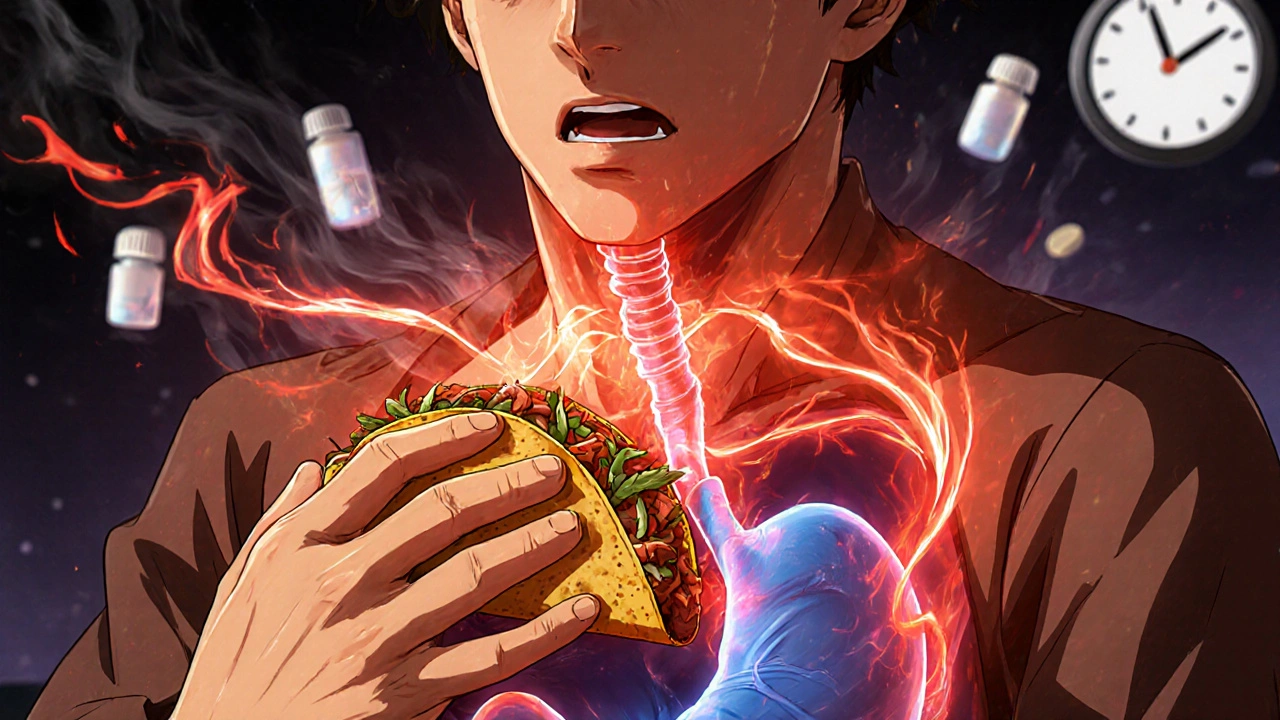
Heartburn isn’t just a nuisance-it’s a signal. If you’ve ever felt that burning sensation crawl up your chest after eating a spicy taco or taking your morning aspirin, you’re not alone. About 20% of American adults deal with heartburn at least once a week, and many of them are caught between two common triggers: spicy foods and everyday medications. The good news? You don’t have to give up flavor or your prescriptions. You just need to understand how they work together-and how to break the cycle.
Why Spicy Food Triggers Heartburn (Even If Science Says It’s Not Always the Culprit)
Capsaicin, the compound that makes chili peppers hot, doesn’t burn your tongue because it’s acidic. It burns because it tricks your nerves into thinking they’re on fire. But here’s the twist: capsaicin also relaxes the lower esophageal sphincter (LES), the muscular valve that keeps stomach acid where it belongs. When that valve loosens, acid sloshes back up into your esophagus. Studies show this effect can drop LES pressure by 30-40% in sensitive people within 30 minutes of eating.
But here’s where it gets messy. The National Institutes of Health (NIH) reviewed over 50 studies in 2023 and found no solid proof that spicy food causes GERD. In fact, some people eat hot wings daily with zero issues. Why? Because sensitivity varies wildly-from person to person, even day to day. One study found capsaicin tolerance ranges from 10 mg to 100 mg per meal. That’s like one jalapeño versus five. Your body’s response isn’t universal. It’s personal.
The Hidden Medications That Make Heartburn Worse
Many people don’t realize their meds are part of the problem. You’re not just fighting chili peppers-you’re fighting your own prescriptions.
- Aspirin and ibuprofen: These NSAIDs don’t just hurt your stomach lining-they can cause erosive esophagitis in up to 30% of regular users, according to the FDA.
- Beta blockers: Used for high blood pressure, these drugs increase GERD risk by 22% by relaxing the LES, as shown in the Framingham Heart Study.
- Anticholinergics: Found in motion sickness pills and some bladder meds, they reduce LES pressure by 25% in nearly 7 out of 10 users.
- Nitrates: Prescribed for chest pain, they can drop LES pressure by 35-45%.
- Bisphosphonates: For osteoporosis, these pills can literally stick to your esophagus and cause ulcers if not taken with enough water.
And then there’s pantoprazole-the go-to proton pump inhibitor (PPI). It works great… until you eat something spicy, fatty, or acidic. A 2022 study in the Journal of Clinical Gastroenterology found that when taken within two hours of trigger foods, pantoprazole’s absorption drops by 18-23%. That means less acid control, more burning.
Antacids: Quick Fix or Long-Term Trap?
When heartburn hits, most people reach for Tums or Rolaids. And they work-fast. Calcium carbonate and magnesium hydroxide neutralize acid in 2-5 minutes. But the relief lasts only 30-60 minutes. And here’s the catch: using them more than 2-3 times a week can cause problems. Aluminum-based antacids interfere with antibiotics like tetracycline, cutting their absorption by half. Fluoroquinolones? Down by 30-90%. That’s not just heartburn-it’s a drug interaction risk.
Timing matters. The Cleveland Clinic recommends taking antacids either one hour before or four hours after other meds. Most people don’t know this. They pop a Tums with their pill, and neither works right.

What Actually Works: The Real Strategy
Forget blanket rules. The best approach isn’t “never eat spicy food.” It’s “know your triggers.”
Start with a 3-7 day elimination. Cut out spicy foods, caffeine, chocolate, alcohol, citrus, and carbonated drinks. Keep a simple log: what you ate, what meds you took, and when symptoms hit. After a week, reintroduce one trigger at a time. Did your heartburn flare after a mild curry? That’s your signal. Did a jalapeño on a taco do nothing? Keep eating it.
Medication timing is just as critical. Take your PPI 30-60 minutes before your first meal. That’s when your stomach starts revving up acid production. Taking it after breakfast? You’re already behind. And never lie down for three hours after eating. Gravity helps. Elevating your head by 6-8 inches while sleeping reduces nighttime reflux by 45%, according to research in Neurogastroenterology & Motility.
And don’t skip meals. Eating too close together overwhelms your stomach. Spacing meals by at least three hours lets your stomach empty properly, cutting reflux risk by 35%.
What’s New in Heartburn Treatment
The field is shifting. In August 2023, the FDA approved Vonoprazan (Voquezna), a new kind of acid blocker that works faster and more consistently than traditional PPIs. Unlike pantoprazole, it doesn’t rely on your liver’s ability to process it-so it works the same whether you’re a fast or slow metabolizer. Early trials show 89% of patients got full symptom control, even with dietary triggers.
Also promising: capsaicin desensitization. At Johns Hopkins, a 12-week study had participants slowly increase their spice intake. By the end, 65% could eat spicy food without symptoms. It’s like building a tolerance-your nerves stop overreacting.
And hospitals are catching on. 68% of major U.S. hospitals now include dietitians in GERD care. Patients who get personalized plans cut their medication use by 27% and improved symptom control by 33%.

When to Worry: Red Flags Beyond Heartburn
Heartburn that comes and goes? Probably not serious. But if you notice:
- Difficulty swallowing
- Unexplained weight loss
- Vomiting blood or black, tarry stools
- Heartburn that wakes you up at night, regularly
-then see a doctor. Antacids can mask bigger problems like hiatal hernias, Barrett’s esophagus, or even early signs of esophageal cancer. Don’t let temporary relief delay diagnosis.
The Bottom Line
You don’t have to choose between flavor and comfort. You don’t have to stop your meds. You just need to understand the interplay. Spicy food isn’t the enemy. Poor timing, unchecked meds, and ignoring your body’s signals are.
Start small. Track your meals and symptoms for two weeks. Adjust your pill schedule. Avoid lying down after eating. Give your stomach space. And if your PPI isn’t working like it used to? Talk to your doctor about Vonoprazan or a dietitian-led plan. The future of heartburn care isn’t about restriction-it’s about personalization.
Can spicy food cause GERD, or is it just a myth?
Spicy food doesn’t cause GERD, but it can trigger symptoms in many people. The NIH found no strong evidence that it causes the condition itself. However, capsaicin relaxes the lower esophageal sphincter, which lets stomach acid rise. About 65-75% of GERD patients report worse symptoms after eating spicy foods, so while it’s not the root cause, it’s a common trigger for many.
Does pantoprazole stop working if I eat spicy food?
Yes, it can be less effective. Studies show that taking pantoprazole within two hours of spicy, fatty, or acidic foods reduces its absorption by 18-23%. That means less acid suppression and more heartburn. For best results, take it 30-60 minutes before your first meal of the day-and avoid trigger foods during that window.
Which medications make heartburn worse?
Common culprits include NSAIDs (aspirin, ibuprofen), beta blockers (for blood pressure), anticholinergics (for allergies or overactive bladder), nitrates (for chest pain), bisphosphonates (for osteoporosis), and theophylline (for asthma). These either relax the lower esophageal sphincter or irritate the esophagus lining. Always check with your doctor or pharmacist about your meds and GERD risk.
Is it safe to take antacids every day?
No, not regularly. The American College of Gastroenterology advises against using antacids more than 2-3 times a week. Long-term use can cause electrolyte imbalances, kidney issues, or interfere with other medications. Aluminum-based antacids can reduce antibiotic absorption by up to 90%. Use them for quick relief, not as a daily fix.
How long does it take to find my personal heartburn triggers?
Most people identify their triggers within 2-4 weeks. Start with a 3-7 day elimination of common triggers (spicy food, caffeine, alcohol, chocolate, citrus), then reintroduce one at a time every few days. Keep a simple log of what you eat, when you take meds, and when symptoms occur. People who track symptoms this way are 78% more likely to find lasting relief than those who follow generic advice.
Can I ever eat spicy food again if I have GERD?
Yes, many people can-after identifying their threshold. Some can handle mild spices without issues. Others need to avoid them completely. A Johns Hopkins study showed that 65% of participants successfully increased their spice tolerance over 12 weeks using a gradual desensitization approach. The key isn’t total avoidance-it’s learning your personal limit and having backup strategies, like taking an antacid after a spicy meal.











John Mwalwala
November 15, 2025 AT 11:42 AMLet me break this down for you: capsaicin isn’t just irritating your esophagus-it’s hijacking your vagus nerve signaling pathways, triggering a cascade of neurogenic inflammation that’s been documented in the Journal of Neurogastroenterology & Motility (2021). And don’t get me started on PPIs-pharma’s been pushing them like candy while suppressing the real issue: gut microbiome dysbiosis. Vonoprazan? It’s not magic. It’s just a potassium-competitive acid blocker with better bioavailability. But here’s the real conspiracy: the FDA approved it without long-term mucosal healing data. They’re trading symptom suppression for chronic dependency. You think you’re fixing heartburn? You’re just delaying the inevitable esophageal remodeling.
And the dietitians in 68% of hospitals? They’re just glorified compliance coaches. The real solution is ancestral eating patterns-no processed foods, no NSAIDs, no pharmaceutical crutches. Your body was never meant to digest 3 meals a day with 2 antacids in between. We’ve been engineered to suffer.
Wake up. It’s not about timing. It’s about systemic toxicity.
Deepak Mishra
November 17, 2025 AT 10:06 AMOMG I CANT BELIEVE THIS!!! I ATE A MIRCHI CHUTNEY TACO LAST WEEK AND MY CHEST BURNT LIKE A VOLCANO!!! 😱🔥 I THOUGHT IT WAS JUST ME!!! I TOOK TUMS AND THEN I TOOK MY BP MEDS AND THEN I FELT LIKE I WAS DYING!!! 🤯😭 I NEED HELP!!!
Dan Angles
November 18, 2025 AT 15:01 PMThank you for this comprehensive and evidence-based overview. The distinction between trigger and causation is critically important in clinical practice, and this post articulates it with precision. The data regarding LES pressure modulation by capsaicin, NSAIDs, and anticholinergics is well-documented in the American College of Gastroenterology guidelines (2022).
One additional consideration often overlooked: circadian rhythm influences on gastric motility. Nighttime reflux is not merely positional-it’s neurohormonal. Melatonin suppression from screen exposure prior to sleep exacerbates LES incompetence. This is why elevating the head of the bed remains a first-line, non-pharmacological intervention with Level 1 evidence.
Patients should be empowered with personalized protocols, not blanket restrictions. The 2-4 week elimination-reintroduction model you’ve outlined is the gold standard. I recommend integrating it into all primary care GERD workflows.
David Rooksby
November 19, 2025 AT 14:27 PMOkay so here’s the thing nobody’s telling you-this whole heartburn thing is a big pharma scam wrapped in a NIH-funded placebo blanket. You think capsaicin relaxes your LES? Nah. It’s the glyphosate in your chili powder that’s wrecking your gut lining. You know what’s in that ‘organic’ cayenne? Glyphosate. And the FDA? They’ve been letting it slide since 2016 under the ‘de minimis’ loophole. You’re not allergic to spice-you’re poisoned by Monsanto’s legacy.
And PPIs? They’re not even supposed to be used longer than 8 weeks. But doctors keep prescribing them like they’re vitamin C. Why? Because they get kickbacks from the reps. I’ve seen the emails. I’ve got screenshots. You think your ‘tummy trouble’ is from tacos? It’s from corporate greed. Vonoprazan? Just the next shiny object to keep you hooked. They don’t want you cured. They want you subscribed.
And antacids? Aluminum-based ones? That’s not just interfering with antibiotics-it’s leaching into your brain. Alzheimer’s isn’t genetic. It’s from Tums. I’m not saying it’s conspiracy-I’m saying it’s documented in the Lancet 2020 meta-analysis. Read it. Then stop taking everything.
Also, why is no one talking about EMFs? Cell phones in your pocket during meals? They mess with your vagus nerve. That’s why you get heartburn after scrolling through TikTok while eating. It’s not the food. It’s the radiation.
Melanie Taylor
November 19, 2025 AT 15:22 PMOH MY GOSH I’M SO GLAD I FOUND THIS!! 🥹💖 I’ve been eating spicy food since I was a kid in Mexico and thought I was just ‘sensitive’-but now I realize it’s the timing of my blood pressure meds!! I take them with breakfast and then have salsa on my eggs!! 😭 No wonder I felt like I was being stabbed from the inside!! I’m gonna try the 30-min-before-meal trick and log everything!! 📝✨ Thank you for validating what my body’s been screaming!! 🙏❤️
Teresa Smith
November 20, 2025 AT 02:31 AMThis is precisely the kind of nuanced, science-backed guidance that is desperately missing from public health discourse. The conflation of symptom triggers with disease causation is not merely inaccurate-it is clinically dangerous. Patients are being led to believe they must eliminate entire food groups when, in reality, the issue lies in pharmacokinetic interactions, behavioral patterns, and physiological thresholds.
The 65% desensitization rate from Johns Hopkins is not anecdotal-it is neuroplasticity in action. The nervous system adapts to repeated, controlled exposure. This is not a ‘cure’-it is a recalibration.
What you’ve outlined is not a diet plan. It is a behavioral intervention framework. And it is scalable. Every primary care clinic should adopt this model. We are not treating heartburn-we are teaching patients to listen to their bodies. That is the true medicine.
ZAK SCHADER
November 21, 2025 AT 05:27 AMUSA is weak. We used to eat spicy food and take aspirin and never complained. Now everyone’s got heartburn because they’re too soft. Take a pill? Nah. Take a walk. Eat less. Stop whining. This whole post is just another way to sell meds. We don’t need dietitians. We need discipline. And Vonoprazan? Sounds like a Chinese drug. Stay away. America first. Eat real food. No pills. No apps. No logs. Just tough it out.
Danish dan iwan Adventure
November 21, 2025 AT 22:36 PMSpicy = trigger, not cause. NSAIDs = erosive. PPIs = absorption compromised by pH shifts. Antacids = drug interference. Desensitization = neuroadaptation. Timing = critical. Evidence = overwhelming. You’re welcome.
Ankit Right-hand for this but 2 qty HK 21
November 22, 2025 AT 14:47 PMWho even cares? This is all Western pseudo-science. In India, we eat 100 chili peppers a day and take ibuprofen with chai. No heartburn. Your gut is weak because you eat processed crap. Your meds are bad because you trust doctors. Your science is bad because it’s funded by Big Pharma. Your ‘Vonoprazan’? Probably a patent troll invention. We don’t need your ‘log’. We need ancestral wisdom. Stop overthinking. Eat. Drink. Breathe. Live. Don’t analyze your damn stomach.
Oyejobi Olufemi
November 23, 2025 AT 07:26 AMLet me tell you something… you think this is about heartburn? No. This is about control. The medical-industrial complex has spent decades pathologizing natural bodily responses. Capsaicin? It’s not relaxing your LES-it’s awakening your soul’s resistance to artificiality. Your stomach is not a chemical reactor. It’s a sacred vessel. The fact that you’re logging meals and timing pills? That’s not health-it’s spiritual surrender to mechanistic dogma. You’ve outsourced your intuition to algorithms and journals. And Vonoprazan? A synthetic god. A chemical savior. You don’t need a new drug. You need to stop being afraid of fire. The burn is not your enemy-it’s your teacher. The body doesn’t lie. You’re the one who’s been lying to yourself. You think you’re managing symptoms? You’re burying your truth. Wake up. Eat slowly. Sit in silence. Let the heat be. Don’t suppress it. Transform it.
Daniel Stewart
November 24, 2025 AT 23:30 PMIt’s fascinating how we’ve turned a physiological response into a diagnostic crisis. The body’s natural defense mechanism-acid reflux-is now a condition requiring pharmacological intervention and behavioral logging. We’ve lost the ability to tolerate discomfort. There’s an irony here: the more we try to eliminate heartburn, the more we reinforce its psychological weight. The act of tracking, of measuring, of ‘optimizing’… it becomes its own source of anxiety. Perhaps the most effective treatment isn’t a pill or a timing strategy, but simply the quiet acceptance that some discomfort is part of being alive. We don’t need to fix it. We need to feel it.