Medication Label Converter
Convert Medication Instructions
Enter any medication dosing instruction to convert it to clear, patient-friendly language using the Universal Medication Schedule (UMS)
How It Works
This tool converts vague instructions into the Universal Medication Schedule (UMS) using:
- "Morning" instead of "twice daily"
- "Noon" and "evening" for more precise timing
- Clear unit indicators (ml, mg, tsp)
- Prevention of common dosage errors
Converted Instructions
Why You Can’t Trust How Your Medication Label Looks
You pick up your prescription. The label says: "Take 1 tablet by mouth twice daily." Sounds simple, right? But if you’re tired, stressed, or not a native English speaker, that phrase can mean anything. Maybe you think "twice daily" means morning and night. Maybe you think it means every 12 hours. Maybe you misread "mg" as "ml" and accidentally take five times the dose. You’re not alone. Nearly half of all adults misinterpret at least one medication instruction. And the worst part? It’s not your fault.
The problem isn’t you. It’s the label.
Most prescription and over-the-counter labels were written for pharmacists, not patients. They use medical jargon, complex sentences, and vague timing like "as needed" or "with meals." A 2009 study found that 47% of patients misunderstood standard labels. Even when instructions were rewritten to be clearer, patients with low literacy were still 2.3 times more likely to make dangerous mistakes. That’s not a small risk. That’s a public health crisis.
What Health Literacy Really Means - And Why It Matters
Health literacy isn’t about how many degrees you have. It’s about whether you can read, understand, and act on health information. The U.S. Department of Education found in 2004 that only 12% of adults had proficient health literacy. That means 88% either struggled or couldn’t understand basic medical instructions. Fast forward to 2023, and the CDC confirms: people with low health literacy are 2.5 times more likely to mess up their doses.
It’s not just about reading. It’s about numbers. It’s about knowing the difference between "take every 12 hours" and "take twice daily." It’s about realizing that "5 mL twice daily" means 5 milliliters each time, not 5 total. One parent told researchers they thought "give 5 mL twice daily" meant give 5 mL total over two doses. That’s the kind of mistake that lands kids in the ER.
And it’s not just pills. Liquid medications, inhalers, patches, even eye drops - all have labels that assume you know what you’re doing. A 2012 review of top-selling children’s cough syrups found that 63% used confusing charts instead of clear instructions. Only 8% used pictures. That’s not an accident. That’s negligence.
The Four Simple Words That Fix Most Dosing Mistakes
There’s a fix. It’s not expensive. It doesn’t need new technology. It just needs four words: morning, noon, evening, bedtime.
This is called the Universal Medication Schedule (UMS). Instead of "twice daily," it says: "Take 1 tablet in the morning and 1 tablet at bedtime." No guessing. No math. No confusion.
When Wisconsin Health Literacy rolled this out in 2022, dosing confusion dropped by 47% among older adults taking five or more medications. One 72-year-old patient said: "I finally understood when to take my pills after they switched to morning/noon/evening/bedtime labels." That’s not a statistic. That’s a life changed.
It works because it matches how people live. Most people don’t think in "every 8 hours" or "q8h." They think: "When I wake up," "When I eat lunch," "When I get home," "When I go to bed." UMS speaks their language.
Pictures Save Lives - And They’re Not Just for Kids
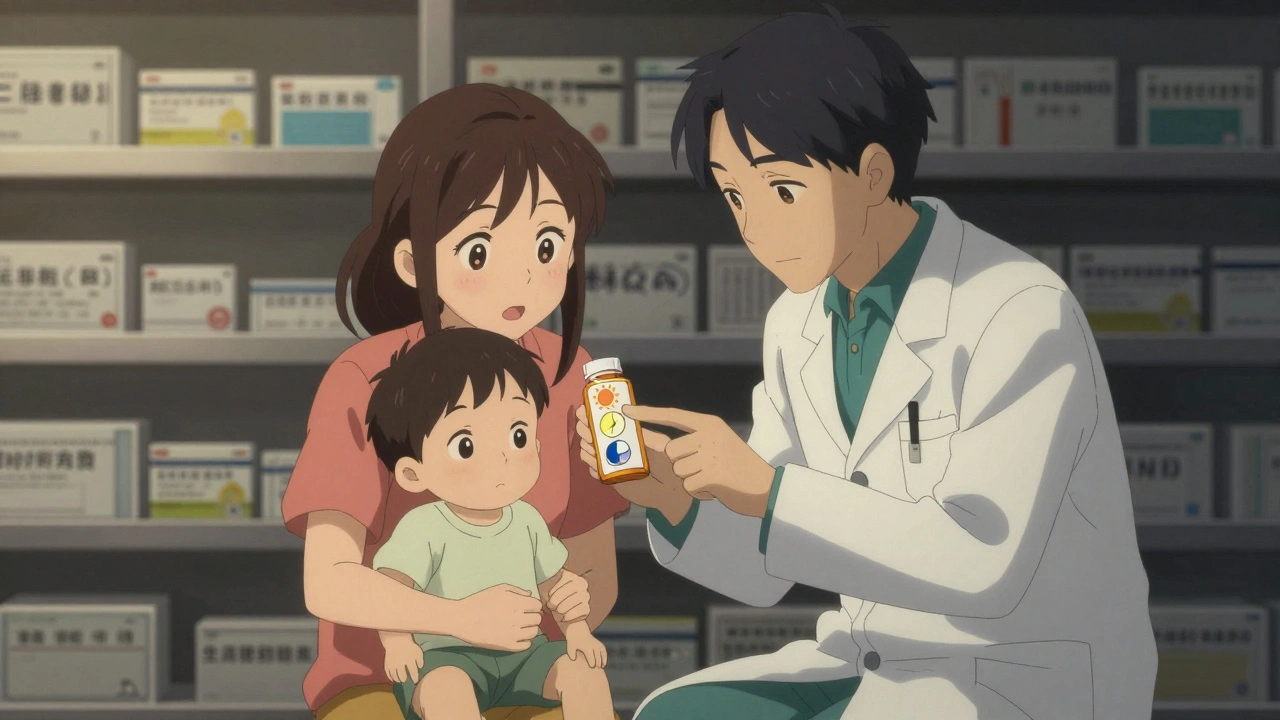
Ever seen a pill bottle with a little drawing of a sun, a clock, and a moon? That’s a pictogram. And it’s not cute decoration. It’s science.
Research shows that adding simple pictures to labels improves understanding by 28% among people with low literacy. A sun means morning. A clock means noon. A moon means bedtime. A hand holding a glass of water means "take with food." No words needed.
One patient described how she drank albuterol from the plastic bottle because she thought it was a "syringe." The label didn’t say "inhale." It didn’t have a picture of an inhaler. She didn’t know what to do with it. That’s not her fault. That’s a labeling failure.
Starting in May 2025, U.S. Pharmacopeia (USP) will require all prescription labels to follow new design rules - including pictograms. This isn’t optional anymore. It’s law.
What You Can Do Right Now - No Doctor Needed
You don’t have to wait for pharmacies to fix their labels. You can protect yourself today.
- Ask for UMS language. If your label says "twice daily," ask: "Can you write it as morning and bedtime?" Most pharmacists will do it.
- Use the teach-back method. After the pharmacist explains, say: "Just to make sure I got it - can you have me repeat it?" Then say it back in your own words. This cuts misunderstanding by 33%.
- Check the units. Is it "mg" or "ml"? Is it "5 mL" or "5 tsp"? Write it down. Use a measuring spoon or syringe - never a kitchen spoon. A teaspoon holds 5 mL, but a tablespoon holds 15 mL. Mistake that, and you overdose.
- Take a picture. Snap a photo of your label. If you’re unsure, send it to a family member or friend who can help you read it.
- Use free tools. The CDC and ISMP offer printable label templates in plain language. Download them. Tape them to your pillbox.
Why Pharmacies Don’t Always Do This - And What’s Changing
You might wonder: if this works so well, why isn’t everyone doing it?
Because it takes time. Training staff, redesigning labels, updating computer systems - it adds 2 to 3 minutes per patient. In a busy pharmacy, that’s a lot of time. Some pharmacists resist. Some doctors don’t know about it.
But things are shifting. The FDA now requires drug companies to test label comprehension with real patients - including those with low literacy. CMS (Medicare) is starting to penalize hospitals with high readmission rates tied to medication errors. That means hospitals now have a financial reason to fix this.
Large health systems like Kaiser and UW Health have already adopted health literacy strategies. They’ve seen 22% fewer readmissions and 15% fewer malpractice claims. That’s not just better care - it’s cheaper care. Every dollar spent on clear labels saves $3.75 in avoided hospital visits.
What’s Coming Next - And How to Stay Ahead
The future of medication safety is here. In 2024, the FDA plans to require standardized pictograms on all prescription labels. Merck is developing an AI tool that can scan your label and tell you if you’re likely to misunderstand it. The CDC is building a national test to measure how well people understand their meds.
But you don’t need to wait. Start today.
Ask your pharmacist: "Is this label written for someone with a 5th-grade reading level?" If they don’t know, ask for a simpler version. Demand pictures. Use a pill organizer labeled with morning, noon, evening, bedtime. Teach back every new prescription. Write down your meds in your own words.
Medication errors are not inevitable. They’re designed. And they can be undone.
Common Mistakes People Make With Medication Labels
- Thinking "take every 4-6 hours" means "take 4 to 6 pills"
- Using a kitchen spoon to measure liquid medicine
- Believing "as needed" means "whenever I feel like it"
- Confusing "take with food" with "take after food" - they’re not the same
- Assuming "twice daily" and "every 12 hours" are identical (they’re not - one allows flexibility, the other doesn’t)
- Not checking the active ingredient - taking two meds with the same drug (like acetaminophen) and overdosing
What does "take with food" really mean?
"Take with food" means take your pill while you’re eating or right after you finish a meal. It doesn’t mean before, or hours later. Some medications need food to be absorbed properly. Others can upset your stomach if taken empty. If you’re unsure, ask: "Should I take it during my meal or right after?"
Can I trust the dosage on over-the-counter medicine labels?
Not always. A 2012 study found that 18.5% of top-selling children’s liquid medicines didn’t list active ingredients on the front. Many used confusing charts instead of clear dosing instructions. Always check the active ingredient - especially if you’re giving medicine to a child. Never combine two meds with the same active ingredient (like acetaminophen) unless a doctor says it’s safe.
Why do different pharmacies use different words for the same instruction?
There’s no national standard - yet. Some pharmacies still use old templates. Others are starting to adopt health literacy guidelines. That’s why you might see "twice daily" at one pharmacy and "morning and bedtime" at another. Ask for the clearer version. If they refuse, go to a different pharmacy. Your safety matters more than loyalty.
How do I know if I’m taking too much of a medicine?
Check the active ingredients. Acetaminophen (Tylenol), ibuprofen (Advil), and diphenhydramine (Benadryl) are in hundreds of cold, flu, and pain meds. Taking two of them together can lead to overdose. For acetaminophen, never take more than 3,000 mg per day. If you’re unsure, write down every medicine you take - including vitamins - and show it to your pharmacist. They can spot overlaps.
Is there a free tool to help me understand my prescriptions?
Yes. The CDC and Institute for Safe Medication Practices (ISMP) offer free printable medication lists and label templates in plain language. Search for "ISMP medication safety tools" or "CDC health literacy resources." You can download them, print them, and tape them to your fridge or pillbox. Some pharmacies even offer them at the counter - just ask.
What to Do If You’re Still Confused
If you’ve tried everything - asked questions, used pictures, wrote it down - and you’re still unsure, don’t guess. Call your pharmacy. Call your doctor. Text a family member. Wait until you’re certain.
It’s better to be late taking a pill than to take too much. Missing one dose won’t hurt you. Taking too much could send you to the hospital.
Medication safety isn’t about being perfect. It’s about being careful. And you’re already ahead of most people just by reading this. Now go protect yourself - one label at a time.









Erin Nemo
December 2, 2025 AT 23:47 PMI used to take my blood pressure pill at 8am and 8pm until my pharmacist switched it to 'morning and bedtime' - game changer. No more guessing. I actually sleep now.
Bonnie Youn
December 4, 2025 AT 16:43 PMYES YES YES this is everything!! I’ve been screaming about this for years - pictograms, plain language, no more ‘twice daily’ nonsense. My grandma finally stopped mixing up her insulin and now she’s thriving. Someone should make this mandatory on ALL meds - like seatbelts. 🙌
Rachel Stanton
December 5, 2025 AT 21:14 PMThe teach-back method is clinically proven to reduce errors by 33%, yet most providers still don’t use it. Why? Because they’re rushed. But here’s the thing - if you’re a patient, you can demand it. Say: 'I want to make sure I understand this correctly - can I repeat it back to you?' It’s not rude. It’s your right. And if they roll their eyes? Find a new provider. Health literacy isn’t optional - it’s survival.
Edward Hyde
December 7, 2025 AT 14:05 PMPharmacies are lazy. They print labels like they’re printing coupons for laundry detergent. I once got a bottle that said 'take as needed for pain' with no max dose. I asked the pharmacist - she shrugged and said 'you know what that means.' I didn't. I almost killed myself with ibuprofen because I thought 'as needed' meant 'as often as I feel like it.' This isn't healthcare. It's Russian roulette with pills.
Suzanne Mollaneda Padin
December 8, 2025 AT 07:43 AMAs a bilingual nurse who works with immigrant families, I see this daily. A mother once gave her 2-year-old 15 mL of cough syrup because the label said '5 mL three times a day' and she thought it meant 5 mL total, three times - she didn’t realize each dose was separate. She didn’t know mL from tsp. We had to rush her to the ER. The label wasn’t wrong - it was cruel. UMS isn’t a suggestion. It’s a moral imperative. We owe it to people who don’t speak English fluently, who are tired, who are scared.
Amber-Lynn Quinata
December 9, 2025 AT 05:29 AMI’m so tired of people acting like this is a 'new idea.' My mom’s been using morning/noon/evening/bedtime labels since 2010. She printed them out, laminated them, taped them to her pill organizer. She didn’t wait for the FDA. She didn’t wait for a 'system.' She just did it. So why are we still talking about this like it’s revolutionary? Because we’re not doing enough. And you? You’re still using kitchen spoons. 🤦♀️
ariel nicholas
December 9, 2025 AT 20:52 PMThis whole thing is a government overreach disguised as 'help.' Who gave anyone the right to dictate how I read a label? I’m an adult. I can figure it out. If you can’t understand 'twice daily,' maybe you shouldn’t be taking pills. And pictograms? Next they’ll be putting emojis on heart medication: 😵💫 = 'don’t drive.' This is infantilization. Not education. And don’t get me started on 'teach-back' - that’s just a fancy way of saying 'prove you’re not dumb.'
Charlotte Collins
December 11, 2025 AT 19:11 PMThe real problem isn’t the labels. It’s the systemic devaluation of low-literacy populations. The fact that we’re still debating whether to use pictures or plain language proves that healthcare is designed for the educated elite. The 88% who struggle? They’re not 'non-compliant.' They’re excluded. And now, with USP mandating changes, the system is finally being forced to acknowledge that its failures aren’t patient failures - they’re design failures. But it took 15 years. And too many ER visits. And too many dead.