Every year in the U.S., more than 400,000 patients suffer preventable harm from medication errors in hospitals. That’s not a statistic from decades ago-it’s what’s happening today. These aren’t rare mistakes. They’re systemic failures that happen because the system is overloaded, under-resourced, and often poorly designed. But here’s the good news: most of these errors can be stopped before they reach the patient. It’s not about blaming nurses or pharmacists. It’s about fixing the systems they work in.
What Counts as a Medication Error?
A medication error isn’t just giving the wrong pill. It’s any preventable mistake that happens while a drug is under the care of a healthcare provider. That includes prescribing the wrong dose, giving a drug to the wrong patient, mixing up similar-sounding names like methotrexate and metoprolol, or failing to catch a dangerous interaction. The American Society of Health-System Pharmacists defines it clearly: if it’s preventable and it causes harm-or could have-it’s an error.One of the most dangerous examples is intrathecal administration of vinca alkaloids. These are cancer drugs meant for IV use only. If they’re accidentally injected into the spinal fluid, they cause irreversible nerve damage or death. That’s not a myth. It’s happened. And it’s happened because labels looked too similar, syringes weren’t color-coded, and no one stopped to double-check.
The Big Players in Medication Safety
There are two major frameworks guiding hospitals today: the ISMP Targeted Medication Safety Best Practices and the Joint Commission’s National Patient Safety Goals. They’re not the same, and knowing the difference matters.ISMP’s list is specific, technical, and brutally practical. It doesn’t say “be careful.” It says: “Hard-stop all daily methotrexate orders unless the prescriber confirms it’s for cancer treatment.” Methotrexate is used weekly for autoimmune diseases. If given daily by mistake, it can kill. Since 2020, hospitals that implemented this hard stop have seen a 37% drop in serious errors. One pharmacy director in Ohio said they stopped three near-misses in the first month alone.
The Joint Commission’s goals are broader. They require hospitals to do medication reconciliation-making sure a patient’s home meds match what’s ordered in the hospital. That’s important. But it doesn’t tell you how to do it. ISMP does. It tells you to use electronic health records with built-in alerts, require double-checks for high-risk drugs, and eliminate glacial acetic acid from patient care areas (yes, that’s a real thing-it’s been confused with saline).
High-Alert Medications: The Silent Killers
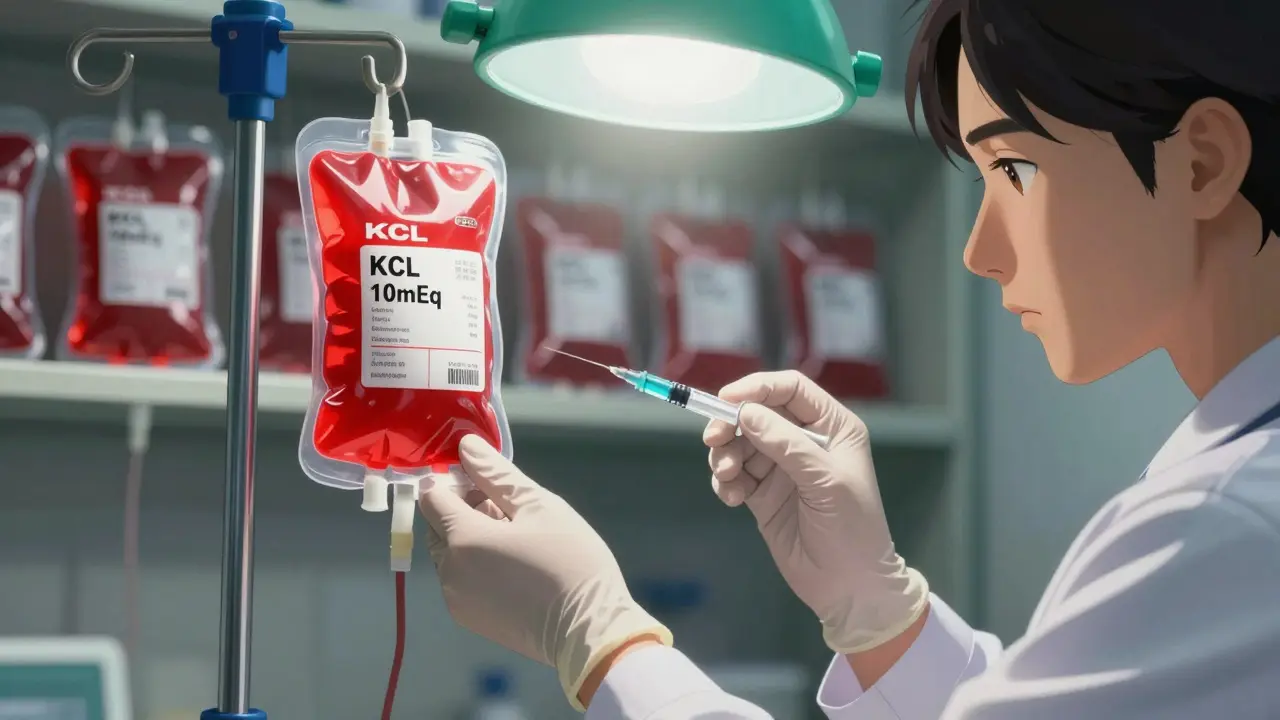
Some drugs are so dangerous that even a small mistake can be fatal. These are called high-alert medications. The ISMP list includes insulin, opioids, anticoagulants, IV potassium chloride, and neuromuscular blocking agents. These aren’t rare drugs-they’re used every day in every hospital.Here’s what works: independent double-checks. Not just one nurse verifying. Two different people, independently, checking the drug, dose, route, and patient. Standardized concentrations. No more “add 10 mL of this to 100 mL of saline.” Use pre-mixed bags. Automated dose range checking. If someone tries to order 500 mg of morphine, the system should scream.
At a community hospital in Iowa, nurses started using color-coded labels for IV potassium. Before, it looked like saline. After, it was bright red. Within six months, zero errors. Simple. Cheap. Life-saving.
Technology Can Help-But Only If It’s Used Right
Barcode medication administration (BCMA) systems are now standard in most large hospitals. Nurses scan the patient’s wristband and the drug barcode before giving anything. It sounds obvious. But in 2022, only 54% of small hospitals had it. Why? Cost. Training. Frustration with clunky systems.Here’s the catch: BCMA only works if you don’t disable it. I’ve heard stories of nurses taping barcodes to their badges so they don’t have to scan. That’s not innovation. That’s defeat. The system is there to protect you-not to slow you down. If your EHR is making it harder to do your job, you’re not the problem. The system is.
Electronic health records with clinical decision support are the backbone. They should flag interactions, allergies, duplicate orders, and renal dosing issues. But 63% of hospitals say their vendor systems won’t let them build hard stops for high-risk meds. That’s a vendor problem. Not a staff problem.
Where It Breaks Down: Staffing, Training, and Culture
No amount of technology fixes a tired nurse working a 12-hour shift with no breaks. No software prevents a mistake when someone’s overwhelmed. The biggest failure isn’t in the code-it’s in the culture.A nurse in a rural clinic posted online: “We’re supposed to give both written and verbal discharge instructions for methotrexate. But we have one pharmacist for 200 patients a day. We skip it. We’re not lazy-we’re broken.” That’s not negligence. That’s systemic failure.
Training needs to be real. Not a 20-minute PowerPoint. Eight to twelve hours of hands-on practice with mock scenarios. Pharmacists walking floors with nurses. Doctors sitting in on med reconciliation rounds. And most importantly: no punishment for reporting errors. If you’re afraid to speak up, mistakes will keep happening.
One hospital in Seattle started a “Safety Huddle” before every shift. Five minutes. One question: “What’s the one thing that could go wrong today?” It didn’t fix everything. But it made people think. And that’s half the battle.

What’s Changing in 2025?
Medication safety isn’t standing still. The FDA just required new labeling for high-concentration electrolytes by the end of 2024. ISMP is expanding its best practices to outpatient clinics-because 40% more errors are happening there since 2019. AI is coming. By 2025, 75% of U.S. hospitals will use algorithms to flag dangerous orders in real time.At Mayo Clinic, they’re testing a new tool: patients report their own meds through a secure app. That data feeds into the EHR. Early results show 32% more errors caught before they happen. Why? Patients remember what they’re really taking. Doctors don’t always.
What You Can Do-Even If You’re Not a Doctor
You don’t have to be a pharmacist to help prevent errors. If you’re a patient or family member:- Always bring a list of every medication you take-including vitamins and supplements.
- Ask: “What is this for? What happens if I miss a dose?”
- Check your wristband before any drug is given. Name. Birth date. All correct?
- If something looks wrong-speak up. Even if you’re not sure.
That’s not being difficult. That’s being smart. And it works. A 2022 survey by the National Council on Aging found 68% of seniors felt safer when staff verified their identity before giving meds.
Final Thought: Safety Is a System, Not a Checklist
Medication safety isn’t about adding more rules. It’s about designing a system where mistakes are nearly impossible. Where the right thing to do is also the easiest thing to do. Where a nurse doesn’t have to choose between saving time and saving a life.The tools exist. The evidence is clear. The cost of doing nothing? Billions in waste. Thousands of lives lost. The question isn’t whether we can afford to fix this. It’s whether we can afford not to.












Vikrant Sura
December 22, 2025 AT 06:58 AMYeah sure, another list of buzzwords. Hard stops, color-coded labels, BCMA - we’ve heard it all. The system’s still broken because nobody’s fixing the staffing crisis. Nurses are drowning, and you want them to scan barcodes while juggling 12 patients? Good luck with that.
Gabriella da Silva Mendes
December 22, 2025 AT 22:28 PMOMG this is why America is falling apart 😭 We spend billions on fancy tech but can’t even hire enough nurses?! My cousin’s nurse forgot to check her meds and she got the wrong insulin dose. Like… come ON. We need to fire the vendors who make clunky EHRs and hire REAL people. Also, why is no one talking about how the FDA lets these dangerous labels slide?? 🇺🇸 #FixHealthcareNow
Sai Keerthan Reddy Proddatoori
December 23, 2025 AT 12:06 PMThis whole thing is a government scam. They want you to trust barcodes and apps instead of God-given common sense. In my village back home, we don’t need scanners - we just ask the patient, check the name, and pray. Now they say if you don’t scan, you’re negligent. But who scans when the machine crashes? Who’s to blame then? The nurse? The system? Or the elites who profit from all this tech?
Johnnie R. Bailey
December 25, 2025 AT 05:56 AMWhat’s missing here is the human architecture of care. We treat safety like a checklist, not a culture. The real innovation isn’t in the barcode scanner - it’s in the moment a senior nurse stops and says, ‘Wait, that dose doesn’t feel right.’ That’s intuition honed by years of watching, listening, and caring. Technology should amplify that, not replace it. And yes - we need to pay nurses enough to think, not just survive their shifts.
Tony Du bled
December 25, 2025 AT 23:57 PMMy mom got a wrong IV once. Turned out the nurse thought ‘KCl’ was ‘KCl’ - same spelling, different bag. No one checked. No one cared. Just another Tuesday. We need better labels, sure. But we also need to stop pretending this is just a tech problem. It’s a ‘we don’t care enough’ problem.
Art Van Gelder
December 27, 2025 AT 08:19 AMLet’s be real - we’re not talking about medication errors. We’re talking about the slow collapse of public trust in institutions. Every time a patient dies because a label looked like another, it chips away at the idea that hospitals are safe places. And it’s not just the nurses or the pharmacists. It’s the administrators who cut corners to hit quarterly targets. It’s the vendors who sell half-baked software and call it ‘compliant.’ It’s the policymakers who write guidelines but never step into a unit at 3 a.m. We’re not fixing systems. We’re just rearranging deck chairs on the Titanic.
Kathryn Weymouth
December 29, 2025 AT 06:54 AMThe point about patients reporting their own medications through an app is the most underappreciated idea here. Patients are the only ones who know exactly what they’re taking - including OTCs, herbs, and supplements that providers never ask about. This isn’t just a safety tool; it’s a shift in power. It acknowledges that patients aren’t passive recipients - they’re essential partners in care. Why isn’t this mandatory everywhere?
Herman Rousseau
December 30, 2025 AT 13:26 PMLove the safety huddle idea. Five minutes. One question. That’s all it takes to wake people up. I work in a small ER - we started doing it last year. We caught a wrong-dose morphine order because a tech said, ‘Wait, that’s 10x what we usually give.’ No one yelled. No one got fired. We just fixed it. That’s the culture we need. Not blame. Not tech. Just people talking to each other.