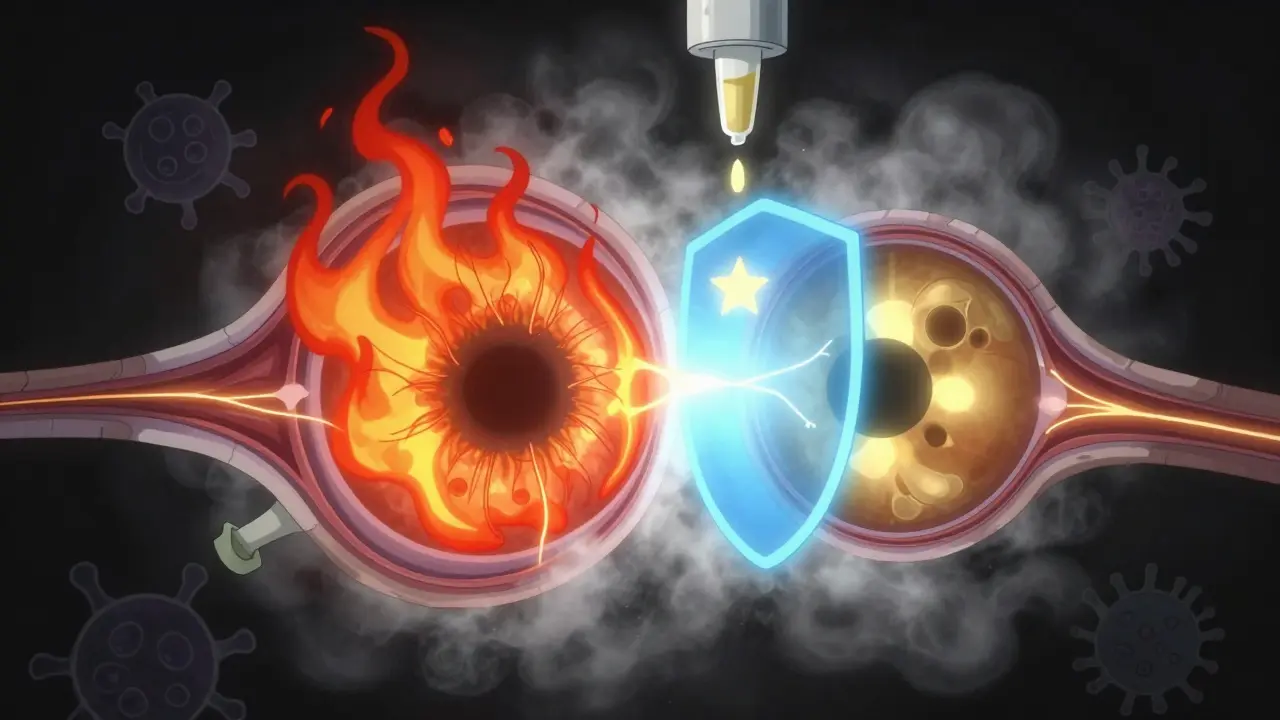
Uveitis is not just a red eye. It’s inflammation deep inside the eye - in the uvea, the middle layer that feeds the retina and iris. Left untreated, it can destroy vision in weeks. Many people mistake it for a simple irritation or pink eye, but uveitis is a medical emergency. If you have sudden eye pain, light sensitivity, or floaters that won’t go away, you need to see an eye specialist now.
What Exactly Is the Uvea?
The uvea isn’t one part - it’s three. The iris (the colored part), the ciliary body (which helps focus the lens), and the choroid (a layer rich in blood vessels behind the retina). Together, they supply oxygen and nutrients to critical eye structures. When inflammation hits any of these, it’s uveitis. The location determines the symptoms, treatment, and risk of vision loss.Four Types of Uveitis - And Why It Matters
Uveitis is classified by where the inflammation lives. Each type behaves differently.- Anterior uveitis (iritis or iridocyclitis) affects the front - iris and ciliary body. It’s the most common, making up 75-90% of cases. Symptoms come on fast: intense redness, sharp pain (worse when reading), light sensitivity, and blurry vision. It often affects just one eye.
- Intermediate uveitis (pars planitis) hits the vitreous, the jelly-like fluid in the middle. Floaters are the main sign - dark spots or squiggles floating across your vision. Blurred vision follows. Pain is mild or absent. This type often lasts months or years and can recur.
- Posterior uveitis attacks the retina and choroid at the back. It’s rare but dangerous. Vision loss can creep in slowly, often without pain. It usually affects both eyes. Many cases are found during routine exams because symptoms are subtle until damage is done.
- Panuveitis means all layers are inflamed. It’s the most severe. Symptoms combine all types: redness, pain, floaters, blurred vision, and rapid vision decline. It’s often linked to serious systemic diseases.
What Causes Uveitis?
In about one-third of cases, doctors can’t find a cause. That’s called idiopathic uveitis. But when there is a trigger, it usually falls into three buckets.- Autoimmune diseases: These are the big ones. Ankylosing spondylitis, multiple sclerosis, rheumatoid arthritis, sarcoidosis, and lupus can all turn the immune system against eye tissue. If you have one of these and develop eye symptoms, uveitis is a major red flag.
- Infections: Viruses like herpes simplex, herpes zoster (shingles), and cytomegalovirus (CMV) can trigger inflammation. Bacterial infections like syphilis or tuberculosis, and even fungi like histoplasmosis, are known culprits. Toxoplasmosis, a parasite often carried by cats, is a leading cause of posterior uveitis.
- Trauma or surgery: A blow to the eye, a penetrating injury, or even eye surgery can spark inflammation. Sometimes the body’s healing response goes too far.
There’s no single test for uveitis. Diagnosis comes from a detailed exam - including a slit-lamp to see inside the eye, and often imaging like OCT scans to check for swelling in the retina.
Steroid Therapy: The First Line of Defense
Steroids are the cornerstone of treatment. They don’t cure the cause - but they stop the inflammation before it destroys vision.How you get them depends on where the inflammation is.
- Anterior uveitis: Steroid eye drops are the go-to. Prednisolone acetate 1% is common. You might start with drops every hour, then taper over weeks. Pupil-dilating drops are often added to prevent the iris from sticking to the lens.
- Intermediate uveitis: Eye drops don’t reach deep enough. Injections around the eye (periocular) or oral steroids like prednisone are used. Sometimes, a slow-release implant is placed inside the eye.
- Posterior uveitis: Oral steroids are standard. For severe or recurrent cases, intravitreal steroid implants (like Ozurdex or Iluvien) deliver medication directly to the back of the eye for months.
- Panuveitis: Usually requires oral steroids from the start, sometimes with immune-suppressing drugs added right away.
Timing matters. The sooner you start steroids, the less likely you are to develop complications like macular edema (swelling in the central retina) or synechiae (scar tissue sticking the iris to the lens). Both can lead to permanent vision loss or glaucoma.
The Hidden Risk: Steroid Side Effects
Steroids work - but they come with costs. Long-term use can cause cataracts (clouding of the lens) and steroid-induced glaucoma (high eye pressure). About 30-40% of people on oral steroids for more than three months develop one or both.This is why doctors don’t just prescribe steroids and walk away. They monitor eye pressure every few weeks. They check for cataracts during follow-ups. And if uveitis keeps coming back, they move to steroid-sparing drugs - like methotrexate, mycophenolate, or biologics. These target the immune system more precisely, letting you reduce or stop steroids altogether.
When to Seek Help - And What to Watch For
Don’t wait. If you have any of these, call your eye doctor the same day:- Red eye that doesn’t improve in 24 hours
- Pain that gets worse when reading or focusing
- Seeing new floaters - especially if they’re sudden or numerous
- Blurred vision that doesn’t clear up with glasses
- Extreme sensitivity to light - even normal daylight hurts
Uveitis can strike anyone. It’s not just older adults. Young, healthy people with no history of illness can develop it after a virus or injury. And it doesn’t always hurt. Posterior uveitis can sneak up silently.

Why Early Treatment Changes Everything
The difference between quick treatment and delay? Vision. A case of anterior uveitis treated within days usually clears with no lasting damage. But if you wait weeks, you risk permanent scarring, glaucoma, or macular edema.Studies show that patients who see a specialist within 72 hours of symptoms have a 90%+ chance of full vision recovery. Those who wait longer than two weeks often face irreversible damage.
There’s no home remedy for uveitis. Ice packs won’t help. Over-the-counter drops won’t touch it. This isn’t a scratch or an allergy. It’s an internal fire - and it needs prescription firepower to put out.
What Happens After Treatment?
Even if your eye looks normal, follow-ups are critical. Uveitis can flare again - sometimes months or years later. If you’ve had it once, you’re at higher risk for another episode.Your doctor will likely recommend:
- Regular eye exams (every 3-6 months if you’ve had chronic uveitis)
- Blood tests to check for underlying autoimmune or infectious causes
- Monitoring for glaucoma and cataracts, even years after treatment
If you’ve been on steroids for more than three months, your doctor may refer you to a rheumatologist or infectious disease specialist to find the root cause and manage long-term immune health.
Can uveitis go away on its own?
Sometimes, yes - but it’s risky. Anterior uveitis may seem to improve after a few days, but inflammation can still be active under the surface. Without treatment, it can lead to scarring, glaucoma, or cataracts. Never assume it’s gone just because symptoms fade.
Is uveitis contagious?
No. You can’t catch uveitis from someone else. But if it’s caused by an infection like herpes or syphilis, those infections are contagious. The eye inflammation itself isn’t spreadable.
Can kids get uveitis?
Yes. Juvenile idiopathic arthritis is a leading cause of uveitis in children. Kids often don’t complain of pain or vision changes. That’s why routine eye screenings are critical for children with autoimmune conditions.
Do I need blood tests if I have uveitis?
Usually, yes. Especially if it’s recurrent, affects both eyes, or doesn’t respond quickly to steroids. Tests can check for autoimmune diseases, infections like syphilis or Lyme, or sarcoidosis. Finding the cause helps prevent future flares and protects other organs.
Can I wear contact lenses if I have uveitis?
No. Contacts can trap bacteria and irritate the eye further. Your doctor will tell you when it’s safe to resume wearing them - usually only after inflammation is fully controlled and the eye surface is healed.
Are there alternatives to steroids?
Yes - but not as a first step. Steroids are still the fastest way to stop inflammation. But if you need long-term treatment, doctors use steroid-sparing drugs like methotrexate, azathioprine, or biologics (like adalimumab). These reduce reliance on steroids and lower the risk of cataracts and glaucoma.
What’s Next?
If you’ve been diagnosed with uveitis, your next step is clear: follow your treatment plan exactly. Don’t stop steroid drops just because your eye looks better. Don’t skip follow-ups. And if you notice any new symptoms - even mild ones - call your eye doctor immediately.Uveitis doesn’t always come back - but when it does, it’s often more aggressive. Early, aggressive treatment now gives you the best shot at keeping your vision for life.










Peyton Feuer
January 4, 2026 AT 07:54 AMman i thought my red eye was just from staying up too late gaming... turned out to be uveitis. doc said if i waited another day i mightve lost part of my vision. holy crap. dont ignore it, folks.
Siobhan Goggin
January 5, 2026 AT 15:46 PMThis is such an important post. I’ve seen too many people brush off eye symptoms as ‘just tired’-and it’s terrifying how quickly things can spiral. Early detection saves sight. Period.
Jay Tejada
January 6, 2026 AT 10:19 AMso you’re telling me my ‘weird floaters’ after that viral conjunctivitis weren’t just ‘eye gunk’? guess i’ll be scheduling that appointment after all. thanks for the kick in the pants, OP.
Allen Ye
January 6, 2026 AT 16:25 PMWhat fascinates me here isn’t just the clinical breakdown-it’s the philosophical implication: the human body is a self-regulating ecosystem, and when it turns on itself, the line between ‘internal’ and ‘external’ dissolves. Uveitis isn’t just an eye disease; it’s a mirror held up to our immune system’s existential crisis. We treat the inflammation, but rarely ask why the system decided to attack its own architecture. Is it genetic? Environmental? Emotional? The answer lies beyond the slit-lamp, in the quiet, unspoken history of the body’s long-term stress. And yet, we still reach for steroids like a bandage on a ruptured dam.
mark etang
January 7, 2026 AT 16:29 PMIt is imperative that individuals experiencing ocular discomfort seek immediate consultation with a qualified ophthalmologist. Delayed intervention may result in irreversible visual impairment. Adherence to prescribed therapeutic regimens is non-negotiable for optimal outcomes.
josh plum
January 8, 2026 AT 14:31 PMbet the pharmaceutical companies love this. steroids? sure. but what about the real cause? why are so many people’s immune systems going haywire? glyphosate? 5g? vaccines? they don’t want you to know it’s not the eye-it’s the system. they profit off the drops, not the cure. wake up.
John Ross
January 10, 2026 AT 02:07 AMPosterior uveitis often presents as a chorioretinitis with vitritis, typically driven by infectious etiologies like Toxoplasma gondii or CMV in immunocompromised hosts. The use of intravitreal implants (Ozurdex, Iluvien) provides sustained release of dexamethasone or fluocinolone acetonide, respectively, achieving therapeutic concentrations in the posterior segment while minimizing systemic exposure. However, the risk-benefit calculus must account for intraocular pressure spikes and cataractogenesis-hence the necessity for steroid-sparing immunomodulators like mycophenolate mofetil or anti-TNF biologics in refractory cases.
jigisha Patel
January 11, 2026 AT 13:12 PMYou neglected to mention that idiopathic uveitis accounts for only 30% of cases in Western populations, not one-third. The remaining 70% are attributable to identifiable systemic conditions, with HLA-B27-associated anterior uveitis being the most common. Furthermore, your assertion that ‘ice packs won’t help’ is misleading-cold compresses may reduce discomfort, though they do not alter disease progression. Precision matters.