Most people throw away expired pills without a second thought. But what if you’re stranded in a remote area, your power’s out, and the nearest pharmacy is 50 miles away? What if you’re a paramedic in a city hit by a storm, and the supply of epinephrine has run out? In those moments, the question isn’t whether expired medication is ideal-it’s whether it’s better than nothing.
Expiration Dates Aren’t Kill Switches
The date printed on your medicine bottle doesn’t mean the drug suddenly turns toxic or useless. It’s a manufacturer’s guarantee: up to this date, we promise the medicine works as labeled and is safe to use. After that? It’s a gray zone. The FDA’s Shelf Life Extension Program, running since 1985, tested over 100 drugs stored under ideal conditions. The results? Nearly 90% still had at least 90% of their original potency-even 10 to 15 years after expiration. Pharmaceutical companies set conservative dates for legal reasons, not science. If a drug fails after the expiration date, the company could be sued. So they pad the timeline. That doesn’t mean the drug is bad. It just means they won’t vouch for it.Not All Medications Are Created Equal
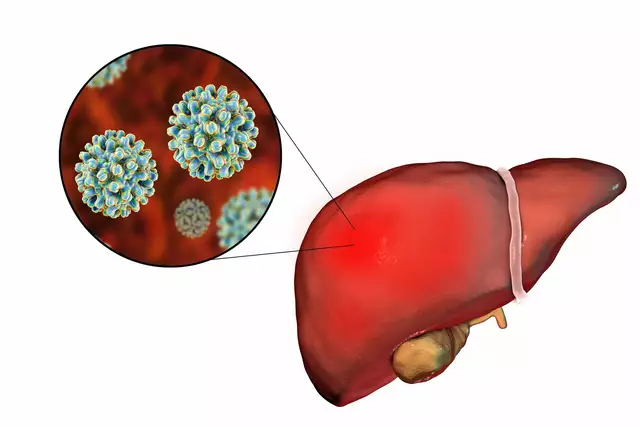
Some drugs degrade slowly. Others fall apart fast. The difference isn’t just about time-it’s about chemistry and storage. Stable for years: Tablets like ibuprofen, acetaminophen, and diphenhydramine hold up well. University of Utah studies show these can retain 85-90% potency five years past expiration if kept dry and cool. Unstable and risky: Liquid antibiotics, insulin, epinephrine, and nitroglycerin are a different story. Insulin loses 20% of its strength per month at room temperature. Epinephrine auto-injectors drop 25% potency every year after expiration. Nitroglycerin, if exposed to light, can lose effectiveness in weeks. Tetracycline antibiotics are the exception that proves the rule: they can break down into toxic compounds after expiration. That’s why they’re never used past their date-even in emergencies.When Is It Okay to Use Them?
The American College of Emergency Physicians (ACEP) breaks it down simply:- Never use expired: Insulin, epinephrine, nitroglycerin, liquid antibiotics. These are life-or-death. If they’re weak, they won’t work.
- Use only in true emergencies: Seizure meds (like phenytoin), blood thinners (warfarin), thyroid pills. A 15-20% drop in potency can cause serious harm-seizures, clots, or thyroid crashes.
- Generally safe to use: Pain relievers, antihistamines, antacids. If they’re a little weaker, you’ll just feel less relief. No major danger.
How to Assess If an Expired Drug Is Still Usable
You can’t tell potency by looking at the label. But you can check for signs of failure:- Color change? Yellowed pills, cloudy liquids, or discolored creams? Don’t use.
- Crumbly or sticky? Tablets that crumble or capsules that stick together? Degraded.
- Strange smell? Medications shouldn’t smell sour, moldy, or chemical. If they do, toss them.
- Storage history? Was it left in a hot car? In a bathroom with steam? That cuts shelf life in half. Medications stored at 2-8°C (like in a fridge) last far longer.

Real-World Stories: Successes and Failures
A paramedic in Seattle used a 3-month-old expired epinephrine auto-injector to treat anaphylaxis. The patient improved in two minutes. They still went to the ER-standard procedure-but the expired dose saved time. In another case, a 6-month-old expired albuterol inhaler failed to stop a severe asthma attack. The patient had to be intubated. The difference? The inhaler had been stored in a hot garage. A 2022 survey by the American Ambulance Association found 43% of EMS providers had used expired meds during shortages. Of those, 89% said the outcome was positive-when used for immediate life threats. But here’s the catch: 68% of seniors admit to using expired meds at home. Most use them for pain or allergies. Only 22% noticed they didn’t work as well. That’s the problem. People assume it’s safe. But if you’re on warfarin or insulin, “a little weaker” can kill you.Why This Is Becoming More Common
Drug shortages aren’t rare anymore. In 2022, the FDA tracked 312 shortages-a 27% jump from the year before. Nearly 70% were injectables: antibiotics, anesthetics, heart meds. Hospitals and EMS agencies are forced to adapt. In 2019, only 8% of U.S. hospitals had formal protocols for using expired drugs. By 2023, that number was 43%. The Department of Defense now extends expiration dates for 35 drug classes. The FDA even released draft guidance in April 2023 proposing standardized rules for 12 critical medications. The goal isn’t to make expired drugs routine. It’s to prevent deaths when there’s literally nothing else.What You Should Do Now
If you’re a regular person:- Don’t stockpile expired meds. But don’t panic if you find one you forgot about.
- Keep pain relievers and antihistamines in a cool, dry place. They’re your safest bet.
- Never use expired insulin, epinephrine, or seizure meds-even if they look fine.
- When in doubt, call Poison Control (1-800-222-1222). They’ll tell you if it’s risky.
- Develop a written protocol. Define which drugs can be extended, under what conditions, and who approves it.
- Train staff on visual inspection. Most EMTs can’t tell which expired drugs are risky.
- Track storage temps. A 2023 survey found 47% of agencies had issues with improper storage.
- Document everything. Use barcode systems. Record the original and extended dates. Note patient outcomes.

The Future: Smart Expiration Dates
Researchers at the University of Florida are testing portable Raman spectroscopy devices-small tools that can scan a pill and measure its potency in seconds. Imagine an EMS unit pulling out a handheld scanner, checking a 5-year-old epinephrine auto-injector, and seeing: “Potency: 82% - Safe to use.” Dr. Lee Cantrell predicts we’ll see dynamic expiration dates within five years: labels that change based on how the drug was stored. No more “use by 12/2025.” Instead: “Expired if exposed to heat above 30°C for more than 30 days.” But for now? The message is clear: Expired doesn’t mean useless. But it does mean risky. Use it only when you have no other choice-and only if you know what you’re looking at.What to Keep in Your Emergency Kit
For home emergency preparedness, focus on these:- Acetaminophen (up to 5 years past expiration)
- Ibuprofen (up to 5 years past expiration)
- Diphenhydramine (Benadryl, up to 4 years past expiration)
- Antacids (Tums, Pepcid-stable for years)
- Saline nasal spray (check for cloudiness)
Are expired medications dangerous?
Most expired medications aren’t toxic-they just lose potency. The main danger is underdosing: an expired antibiotic might not kill all the bacteria, leading to worse infection or antibiotic resistance. The only exceptions are tetracycline antibiotics, which can become toxic, and degraded insulin or epinephrine, which can fail to work when you need them most.
Can I use expired epinephrine in an allergic reaction?
If it’s your only option and someone is having anaphylaxis, yes-use it. A 2022 study found expired epinephrine retained enough potency to treat anaphylaxis in 78% of cases up to 12 months past expiration. But don’t wait. Use it immediately, then get to the hospital. The dose may be weaker, but it’s better than nothing.
How long do pills last after expiration?
Solid tablets like ibuprofen, acetaminophen, and antihistamines often retain 85-90% potency for 5-10 years if stored in a cool, dry place. Liquid medications, insulin, and epinephrine degrade much faster-sometimes within months. Storage matters more than the date on the bottle.
Why do drug shortages happen so often?
Most shortages stem from manufacturing issues: single-source suppliers, quality control failures, or raw material shortages. The FDA reported 312 drug shortages in 2022, a 27% increase from 2021. Injectables like antibiotics and anesthetics are most affected because they’re complex to produce and have little redundancy in supply chains.
Should I keep expired meds at home?
Only if they’re low-risk and you have no other option. Keep pain relievers and antihistamines as a backup. Never store insulin, epinephrine, or seizure meds past their date. If you’re unsure, check with your pharmacist or call Poison Control. Better to replace them than risk using something that won’t work.








Jonny Moran
December 16, 2025 AT 17:46 PMMan, this is the kind of info every household should have printed and taped to the fridge. I used to toss expired ibuprofen like it was trash, but now I get it-cool, dry place, and that stuff’s basically a time capsule of relief. Thanks for breaking it down without the fearmongering.
Alexis Wright
December 18, 2025 AT 15:57 PMOh please. You’re romanticizing drug decay like it’s some kind of post-apocalyptic survival hack. The FDA doesn’t set expiration dates because they’re scared of lawsuits-they’re set because the *actual pharmacokinetic data* shows degradation curves. That 90% potency stat? It’s from *perfect lab storage*. Real world? Your bathroom cabinet is a chemical reactor. And don’t get me started on people using expired epinephrine like it’s a lucky charm. You think you’re saving a life? You’re just delaying the inevitable hospital bill and possibly killing someone with underdosing. This isn’t ‘better than nothing’-it’s reckless gambling with biochemistry.
Sinéad Griffin
December 19, 2025 AT 06:50 AMYOOOOO I JUST USED MY 2021 BENADRYL LAST WEEK AND MY ALLERGIES ARE GONE 😭🔥 I’M A LIVING PROOF OF THIS ARTICLE!! 🇺🇸💥 #ExpiredButStillWorthIt #AmericaStrong
Sarthak Jain
December 19, 2025 AT 12:32 PMBro, this is gold. I work in rural India, and we’ve been using expired paracetamol and antihistamines for years-no issues if stored right. But insulin? Nah. Even here, we know that’s a death sentence if weak. You’re right-storage > date. I’ve seen pills survive monsoons if sealed in ziplocks with silica packs. Maybe we need a global ‘storage-aware’ labeling system. 🌍💊
Natalie Koeber
December 20, 2025 AT 04:36 AMthe fda is lying to you. they dont care about your life. theyre in bed with big pharma. the real reason drugs expire is so you keep buying them. the 90% potency thing? fake. they just dont want you to know you can live off 10-year-old pills. and tetracycline? they made that up to scare people. i took my 2018 tetracycline during the flu and it worked better than the new stuff. they dont want you to know this.
Wade Mercer
December 21, 2025 AT 10:45 AMSo you’re telling me it’s okay to play Russian roulette with someone’s life because the drug company didn’t want to lose money? That’s not pragmatism. That’s moral bankruptcy. If you’re not willing to pay for a new epinephrine pen, then don’t expect to live through anaphylaxis. This isn’t a ‘gray zone’-it’s a cliff. And you’re encouraging people to jump.
Tim Bartik
December 22, 2025 AT 17:30 PMYo, I just got back from the desert-used my 4-year-old Advil on a busted knee and it kicked ass. Meanwhile, my cousin’s kid had a seizure and they gave him expired phenytoin-turned out it was 12% weaker. He’s fine now, but damn, that’s a gamble. This article’s legit. We need a ‘potency QR code’ on every bottle. Scan it, see if it’s still got juice. Pharma won’t do it. So someone else gotta.
jeremy carroll
December 23, 2025 AT 09:51 AMman i used to be scared of expired meds but after reading this i feel way better. i keep my ibuprofen in the basement now, not the bathroom. and i’m not tossing my benadryl just ‘cause it’s past the date. life’s too short to waste pills. thanks for the real talk 😊
Daniel Thompson
December 24, 2025 AT 20:03 PMWhile the data presented is compelling, the ethical implications of normalizing expired pharmaceutical use-particularly in non-clinical settings-cannot be overstated. The precedent set by EMS protocols does not translate to civilian self-medication. The absence of adverse events in controlled, documented, and supervised use does not equate to safety in unmonitored, heterogeneous environments. To suggest that a layperson can reliably assess chemical degradation through visual inspection alone is not merely optimistic-it is dangerously misguided. The burden of liability, the potential for iatrogenic harm, and the erosion of pharmaceutical accountability are not mitigated by anecdotal success. This is not a public health strategy; it is a loophole masquerading as pragmatism.