When you’re living with rheumatoid arthritis, lupus, Crohn’s disease, or another autoimmune condition, the goal is simple: stop your immune system from attacking your own body. But the drugs that do this-immunosuppressants-come with a hidden cost. They don’t just quiet the bad actors in your immune system. They silence the good ones too. And that’s where the real danger lies.
What Immunosuppressants Actually Do
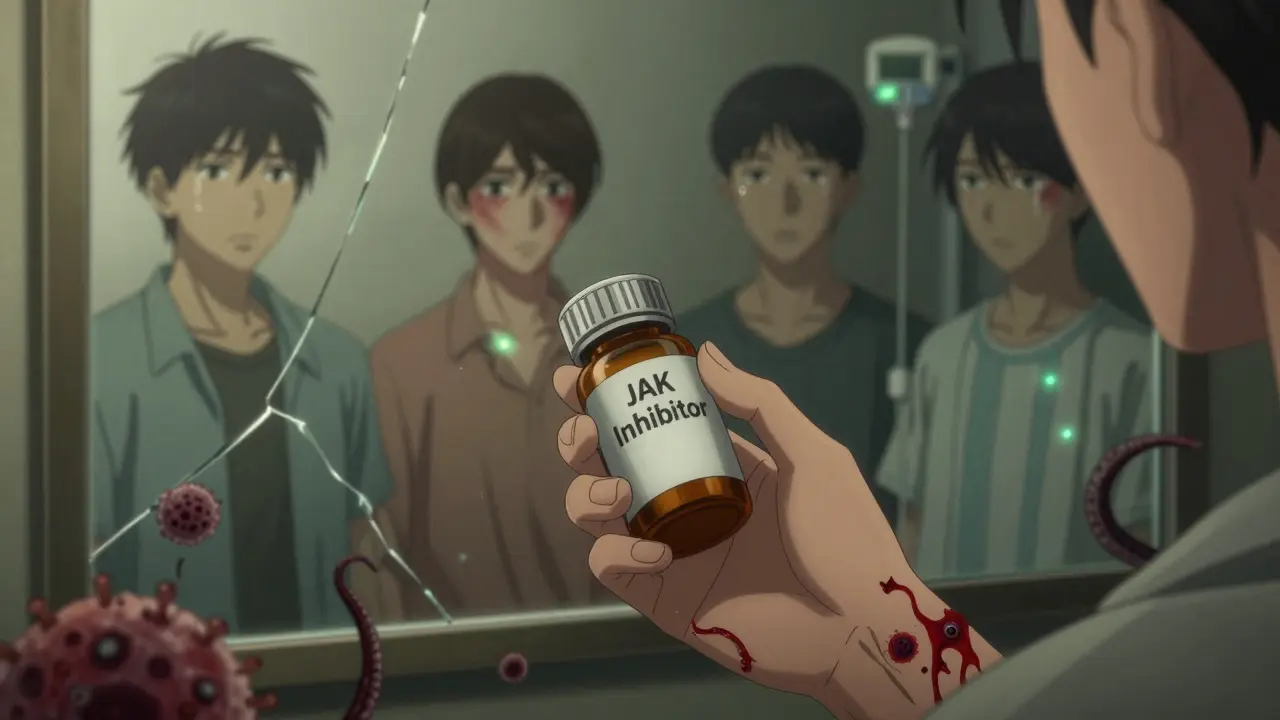
These medications aren’t just anti-inflammatories. They’re systemic dampeners. Drugs like prednisone, methotrexate, adalimumab, and tofacitinib work by targeting different parts of your immune response. Some block signaling proteins (TNF inhibitors). Others wipe out B cells (rituximab). Some shut down enzyme pathways inside immune cells (JAK inhibitors). The result? Less joint damage, fewer skin flares, less gut inflammation. But also, less ability to fight off infections.
Think of it like turning down the volume on an alarm system. It stops the false alarms-but now, when a real burglar breaks in, no one hears it. That’s why patients on these drugs get pneumonia, shingles, or even rare brain infections like PML. It’s not that the drugs are broken. It’s that they’re powerful-and broad.
The Big Five Complication Risks
Not all immunosuppressants are created equal. Their risks vary wildly depending on the class. Here’s what you’re actually up against:
- Corticosteroids (prednisone, budesonide): These are the oldest and most widely used. But they’re also the most indiscriminate. Taking more than 20 mg per day for over two weeks can leave you vulnerable to fungal, viral, and bacterial infections. Even after you stop, your immune system can stay suppressed for weeks. Studies show you’re 10-15% more likely to get an opportunistic infection than someone on a biologic at the same disease control level.
- JAK inhibitors (tofacitinib, baricitinib, upadacitinib): These are newer oral drugs, convenient and effective. But they come with a dark side. They triple your risk of shingles compared to older biologics. They also raise your chance of blood clots and, in people over 65 who smoke, increase lung cancer and lymphoma risk by up to 44%. The FDA added black box warnings in 2022 after data from the ORAL Surveillance study confirmed these dangers.
- B-cell depleters (rituximab, ocrelizumab): These drugs wipe out your B cells-the immune cells that make antibodies. It’s effective for lupus and MS, but it leaves you defenseless for months. After a single infusion, your body can’t respond to vaccines for up to a year. Hepatitis B can reactivate. Rare brain infections can sneak in. One patient on Reddit described shingles lasting four months after rituximab, even with antivirals. His doctor never warned him about the six-month window of highest risk.
- Calcineurin inhibitors (cyclosporine, tacrolimus): Common in transplant patients, these are also used for severe psoriasis and lupus. They’re tough on your kidneys. Up to 40% of long-term users develop measurable kidney damage within two years. Blood pressure spikes and tremors are common. They’re not first-line for most autoimmune diseases anymore-but when used, they need constant monitoring.
- IMDH inhibitors (azathioprine, mycophenolate, leflunomide): These hit the bone marrow. About 1 in 5 people on these drugs develop low white blood cell counts, low platelets, or anemia. Monthly blood tests aren’t optional-they’re life-saving. One patient on PatientsLikeMe switched from methotrexate to sulfasalazine after liver enzymes spiked. His GI doctor said sulfasalazine was safer long-term, but less effective for joints.
Who’s at Highest Risk?
Not everyone on immunosuppressants gets sick. But some people are far more vulnerable. Risk isn’t just about the drug-it’s about your age, your health, and your lifestyle.
- If you’re over 65, your immune system is already aging. Add a JAK inhibitor? Your risk of lymphoma jumps.
- If you smoke, your lungs are already damaged. A JAK inhibitor makes lung cancer more likely.
- If you’ve had hepatitis B before, even if it’s “cleared,” rituximab can wake it up. Testing before treatment isn’t optional-it’s mandatory.
- If you’re on multiple immunosuppressants-say, prednisone plus methotrexate-the risks stack. It’s not additive. It’s exponential.
Dr. Joan Merrill at the Oklahoma Medical Research Foundation says the biggest mistake doctors make is treating all immunosuppression as the same. It’s not. A patient on hydroxychloroquine has almost no increased infection risk. A patient on rituximab is in a completely different danger zone.
What You Can Do to Stay Safe
There’s no way to eliminate the risks-but you can drastically reduce them.
- Vaccinate early. Get all your vaccines-at least four weeks before starting any B-cell depleting drug. That includes flu, pneumonia, shingles, and COVID. Don’t wait. Once you’re on rituximab, your body won’t respond. A 2022 study found 68% of serious infections could’ve been prevented with timely vaccines.
- Test before you start. If you’re getting rituximab or similar drugs, you need a hepatitis B blood test. If you’ve ever had it, even decades ago, you’ll need antiviral protection during and after treatment.
- Monitor your blood. If you’re on azathioprine, mycophenolate, or methotrexate, you need a complete blood count every month. Low white cells? Your doctor needs to know now, not when you’re in the ER with sepsis.
- Watch for shingles. If you’re on a JAK inhibitor, get the recombinant shingles vaccine (Shingrix), even if you had chickenpox as a kid. It’s still effective. And if you get a rash that burns or tingles-don’t wait. Call your doctor immediately.
- Ask about alternatives. Hydroxychloroquine has the highest patient satisfaction rating (7.8/10) for safety. Methotrexate at low doses is safer than most biologics. For mild disease, you might not need the heavy artillery at all.
The Hidden Cost: Money, Time, and Stress
These drugs aren’t just risky-they’re expensive. Biologics cost $20,000 to $40,000 a year. Insurance now requires prior authorization for them, and Medicare won’t cover them unless you’ve documented infection prevention steps. That means extra blood tests, specialist visits, and paperwork.
And then there’s the emotional toll. A 2022 survey by the Arthritis Foundation found that 42% of patients stopped their biologics because they were scared of getting seriously sick. One nurse with RA wrote on HealthUnlocked: “I’ve seen colleagues on JAK inhibitors get recurrent shingles despite vaccination. Now I check my VZV titers every six months.” That’s not normal. That’s a life lived in constant vigilance.
Meanwhile, the U.S. healthcare system spends $4.2 billion a year treating infections in people on immunosuppressants. That’s 18% of all hospitalizations in this patient group.
The Future: Smarter Immunosuppression
The field is changing. New drugs in development aren’t trying to crush the entire immune system. They’re targeting specific pathways-like IL-23 or T-cell co-stimulation-with precision. The FDA’s 2023 REMS program now requires mandatory training for doctors prescribing JAK inhibitors. The NIH launched a $28 million project to find biomarkers that predict who’s most at risk for infection. Mayo Clinic’s AI tool, tested in a 2022 pilot, cut serious infections by 22% by analyzing EHR data to flag high-risk patients.
But the biggest shift? Doctors are finally moving away from the old binary: “immunosuppressed” or “not.” Now, they’re stratifying risk into four tiers. A patient on hydroxychloroquine? Low risk. Someone on rituximab? High risk. That’s not just better medicine-it’s safer medicine.
Bottom Line: Knowledge Is Your Best Defense
Immunosuppressants save joints, skin, and organs. But they also leave you exposed. The key isn’t avoiding them-it’s understanding exactly what you’re taking, how it affects your body, and what steps you need to take to protect yourself.
If you’re on one of these drugs, ask your doctor:
- Which class am I on, and what are its specific risks?
- Have I had all the right vaccines, and when was the last time I got them?
- Do I need regular blood tests? How often?
- Is there a safer alternative for my condition?
You’re not just a patient. You’re the manager of your own immune system. And in this case, the best treatment isn’t always the strongest drug. It’s the one that keeps you alive-and healthy-long after the inflammation is gone.
Can I still get vaccines while on immunosuppressants?
Yes-but timing matters. Live vaccines (like MMR, chickenpox, nasal flu) are dangerous if you’re on strong immunosuppressants like rituximab or high-dose steroids. Stick to inactivated vaccines: flu shot, pneumonia, shingles (Shingrix), and COVID. Get them at least 4 weeks before starting any B-cell depleting drug. Once you’re on treatment, your immune system may not respond well, so don’t wait. If you’re already on therapy, talk to your doctor about checking antibody levels after vaccination.
Are biologics safer than steroids for long-term use?
It depends. Steroids like prednisone cause broad, dose-dependent immunosuppression and carry risks of diabetes, bone loss, and cataracts over time. Biologics target specific immune pathways, so they’re less likely to cause those side effects. But they can still cause serious infections-especially B-cell depleters like rituximab. For long-term use, biologics are often preferred over steroids, but only if your infection risk is low and you’re monitored properly. Methotrexate at low doses is often a better middle ground than either.
Why do JAK inhibitors increase the risk of blood clots?
JAK inhibitors block signaling pathways involved in immune function-but they also affect platelets and clotting factors. The ORAL Surveillance trial found that tofacitinib caused 1.5 to 2.0 extra blood clots per 1,000 patient-years compared to TNF inhibitors. This risk is highest in people over 50 with heart disease or who smoke. That’s why the FDA added a black box warning in 2022. If you’re on a JAK inhibitor and have risk factors for clots, your doctor should consider alternatives.
Is hydroxychloroquine really the safest option?
For mild autoimmune conditions like lupus or early rheumatoid arthritis, yes. Hydroxychloroquine has minimal immunosuppressive effect. Studies show no significant increase in serious infections. In patient reviews across 12,450 users, it scored 7.8/10 for safety-higher than biologics (6.2) or JAK inhibitors (5.9). The main risk is eye toxicity with long-term use, which is why annual eye exams are required. But for low-risk patients, it’s often the best first choice.
What should I do if I get a fever while on immunosuppressants?
Don’t wait. Call your rheumatologist or go to urgent care immediately. A fever in someone on immunosuppressants can signal a serious infection-even if you feel fine otherwise. Don’t assume it’s just a cold. Your immune system can’t mount a normal response, so symptoms might be subtle. You may need blood cultures, chest X-rays, or even hospitalization. Delaying care increases the risk of sepsis or organ failure.
Can I stop my medication if I’m worried about side effects?
Never stop on your own. Abruptly stopping steroids can cause adrenal crisis. Stopping biologics suddenly can trigger a severe disease flare. If you’re concerned about side effects, talk to your doctor. There may be a safer alternative, a lower dose, or a different drug. Your goal isn’t just to survive the medication-it’s to live well with your condition. That means working together to find the right balance.












Adewumi Gbotemi
January 12, 2026 AT 05:54 AMMan this hit different. I'm from Nigeria and we don't have access to most of these drugs, but I know people who take steroids for lupus and just suffer in silence. No tests, no vaccines, just hope. It's scary how much privilege goes into just staying alive with these conditions.
Priya Patel
January 13, 2026 AT 22:17 PMOMG I JUST GOT SHINGLES ONCE WHILE ON METHOTREXATE 😭 I thought it was a bug bite for 3 days and then it was like fire on my skin. My doc never warned me. Now I get Shingrix every year like it's my job. Also, PLEASE get your blood work done. I almost died because I skipped my CBC for 'too busy'. Don't be me.
Sean Feng
January 15, 2026 AT 12:48 PMSo basically we're all just guinea pigs for Big Pharma and the doctors are too lazy to read the black box warnings
Michael Patterson
January 16, 2026 AT 08:57 AMLook i've been on prednisone for 12 years and i know what i'm talking about. You think the 10-15% infection risk is bad? Try living with the moon face the insomnia the weight gain the osteoporosis the cataracts the diabetes. And dont even get me started on how the insurance companies treat you like a criminal if you try to switch meds. I had to fight for 8 months to get off steroids and onto a biologic because my doctor was too lazy to write the letter. And now i'm on adalimumab and guess what i got pneumonia last winter. So yeah the drugs are dangerous but the system is worse. And dont even tell me to take hydroxychloroquine its useless for my RA. I tried it for 6 months and it did nothing except make me nauseous. So dont be one of those people who thinks its one size fits all. My body is not your blog post.
Also the FDA is a joke. They approved JAK inhibitors and then acted shocked when people got cancer. Like hello its in the damn trial data. And now they want us to get blood tests every month but dont pay for them. So i have to choose between paying for my rent or my labs. Thats the real choice. Not drug A or drug B. Its eat or survive.
And dont get me started on the vaccine timing. I got my shingles shot 3 weeks before starting rituximab and my titers were still zero after 6 months. So what do i do? Pay 2k for another shot? No thanks. My doctor says its still better than nothing. But its not. Its a placebo for guilt.
And yes i know i shouldnt smoke but i do. And i know i shouldnt drink but i do. And i know i shouldnt skip my meds but sometimes i do because i cant afford them. So dont judge me. Im trying. Im just tired. And i wish someone would fix the system instead of just telling me to be more responsible.
Also the AI tool at Mayo? Sounds cool but i live in rural Ohio. No internet. No specialists. Just me and my phone and a 3 hour drive to the nearest rheum. So yeah. Knowledge is power but power costs money. And i dont have any.
And for the love of god stop telling people to ask their doctor. Most of us have been seeing the same doc for 10 years and they dont even remember our names. So dont give me that advice. Its useless.
And yes i know im long winded. But if you think this is bad you should see my last email to my insurance company. 17 pages. 3 attachments. 27 calls. And they denied it anyway.
Priscilla Kraft
January 17, 2026 AT 10:20 AM❤️❤️❤️ This is so important. I was on tofacitinib for 18 months and had a blood clot at 42. My doctor didn't even mention the risk. Now I'm on hydroxychloroquine and I feel like I got my life back. Also got my Shingrix and pneumonia shots before starting. Do it. Your future self will thank you. And yes, monthly blood tests are annoying but they saved my life. You're not being paranoid-you're being smart. 💪
Roshan Joy
January 18, 2026 AT 13:40 PMInteresting read. I'm from India and we don't have access to most biologics here. Most people here are on methotrexate or steroids. But I've seen patients on azathioprine develop severe anemia because they didn't get regular CBCs. One guy ended up in ICU. I think the key point here is monitoring. No matter the drug, if you're not tracking your numbers, you're flying blind. Also, vaccines before starting treatment? Non-negotiable.
Madhav Malhotra
January 18, 2026 AT 16:52 PMFrom India too. We have this weird thing where people think if it's cheap, it's safe. My aunt took cyclosporine for psoriasis for 3 years and now has kidney failure. No one told her. No tests. Just a script. And she's 52. This isn't just a Western problem. The lack of awareness is global. We need more community health workers to explain this stuff. Not just doctors in fancy clinics.
Jason Shriner
January 18, 2026 AT 23:12 PMSo let me get this straight. We're supposed to get a vaccine, then wait a month, then take a drug that might kill us, then get blood tests every month, then pray we don't get shingles, then pay $30k a year, and if we do get sick, the system will blame us for not doing enough? Sounds like a dystopian sitcom. I'm just here for the popcorn.
Jennifer Littler
January 20, 2026 AT 00:00 AMAs a rheumatology nurse practitioner, I see this daily. The biggest gap isn't the drugs-it's the lack of coordinated care. Patients get prescribed JAK inhibitors, then get sent to a PCP for blood work, who doesn't know the protocol. No one's communicating. We need integrated care teams. Not just more education. Systems change. Not just patient compliance.
Alfred Schmidt
January 21, 2026 AT 08:03 AMTHIS. IS. A. TRAGEDY. I have a friend who lost her husband to PML after rituximab. He had hepatitis B. They didn't test him. The clinic said 'it's rare.' Rare? It's 1 in 250. And they didn't warn him. He was 47. He had two kids. Now she's alone. And the drug company? They made billions. And the FDA? They just added a black box. AFTER the deaths. AFTER the lawsuits. AFTER the families were broken. This isn't medicine. This is corporate manslaughter dressed in white coats. And you want me to 'ask my doctor'? My doctor works for the hospital that gets paid every time they prescribe it. Who do you think they're loyal to?
Vincent Clarizio
January 22, 2026 AT 02:16 AMLet’s be real. Immunosuppression isn’t the problem. The problem is that we treat autoimmune diseases like they’re all the same, when they’re not. It’s like using a sledgehammer to fix a watch. We’ve been doing this for 50 years. We keep reaching for the biggest gun because we’re too lazy to understand the nuances. The real innovation isn’t in new drugs-it’s in stratifying risk. Tiered risk models? That’s the future. Not another biologic. Not another JAK. But knowing who needs what, when, and why. And that’s not just science-it’s philosophy. It’s about respecting the individual. Not the algorithm. Not the profit margin. Not the protocol. But the person. The one who’s tired. The one who’s scared. The one who just wants to live without fear. And if we can’t do that? Then we’re not healers. We’re just pharmacists with better PR.
Also, hydroxychloroquine is underrated. It’s not sexy. It doesn’t have a fancy name. But it’s the quiet hero. And we’ve forgotten that sometimes the best medicine is the one that doesn’t try to change everything. Just calms it down. Gently. Like a lullaby. Not a bomb.
And yes, I know I’m dramatic. But when you’ve seen three patients die from preventable infections on drugs they were never properly warned about, you start to speak in paragraphs. And I don’t care if you think it’s too long. It’s not. It’s necessary.
Sam Davies
January 22, 2026 AT 09:23 AMOh wow, a 4.2 billion dollar problem. How quaint. I suppose the real tragedy is that none of this was ever discussed in med school. Or maybe it was, but the pharma reps made sure the slides were updated with the right brand names. How very corporate of us. Meanwhile, patients are left Googling 'can I get shingles from a JAK inhibitor' at 2am while their insurance denies the blood test. The irony is delicious.
Matthew Miller
January 23, 2026 AT 14:18 PMYou people are pathetic. You think this is hard? Try being a doctor trying to navigate this mess. You want safer drugs? Fine. But you also want them cheap. You want no side effects. You want no blood tests. You want no vaccines. You want to live forever on a pill. Guess what? Biology doesn't work that way. You want to live with a broken immune system? Then you accept the consequences. Stop whining. Get your shots. Get your labs. Stop blaming the doctors. The system is broken? Fix it. Or shut up and take your meds.
Priscilla Kraft
January 23, 2026 AT 15:14 PM@6731 I hear you. But the problem isn’t patients being ‘pathetic’-it’s that doctors are trained to prescribe, not to partner. I’ve had patients cry because their doctor said ‘just take it’ and walked out. That’s not medicine. That’s transactional. We need to fix the relationship, not just the meds.