Most people assume that if a drug is approved by the FDA, it’s completely safe to use. But here’s the truth: drug interactions that can cause serious harm - even death - are often only discovered after millions of people have already taken the medicine.
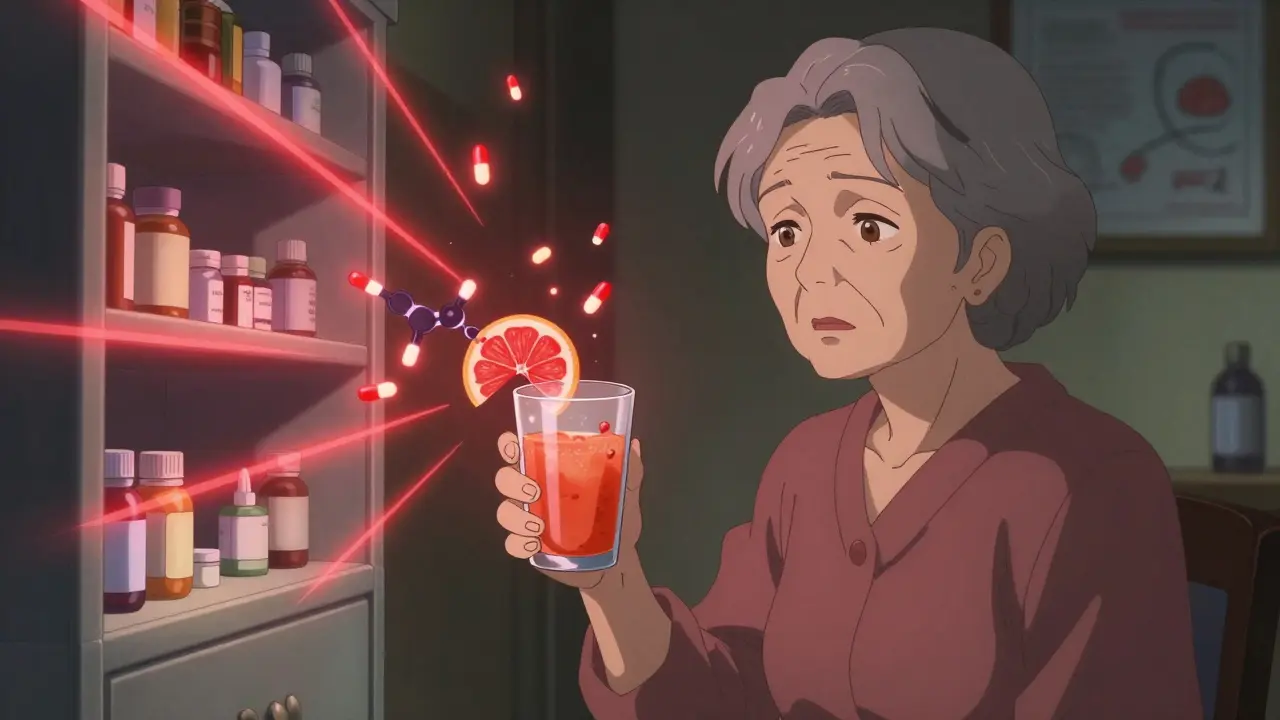
Think about it. Clinical trials for new drugs usually involve a few thousand people over six to twelve months. That’s not enough time or variety to catch every possible problem. What happens when a 78-year-old with kidney disease, diabetes, and high blood pressure takes that same drug for five years while also using herbal supplements, antibiotics, or even grapefruit juice? That’s where things go wrong - and that’s exactly what post-market surveillance is designed to find.
Why Clinical Trials Miss Dangerous Interactions
Clinical trials are tightly controlled. Participants are generally healthy, younger, and have few other medical conditions. They’re monitored closely, and they don’t usually take more than one or two other medications. Real life? Totally different.
Real patients take multiple prescriptions. They use over-the-counter painkillers. They drink grapefruit juice because they’ve heard it’s healthy. They start taking St. John’s Wort for low mood. None of that is captured in trials. And that’s why some of the most dangerous drug interactions slip through.
Take simvastatin (Zocor), a common cholesterol drug. During trials, it looked fine. But after millions of people started using it, doctors noticed a spike in rhabdomyolysis - a condition where muscle tissue breaks down and can lead to kidney failure. The culprit? Common antifungal drugs like fluconazole (Diflucan). These drugs block the liver enzyme CYP3A4, which normally breaks down simvastatin. When that enzyme is blocked, simvastatin builds up to toxic levels - up to 10 times higher than normal. That’s not a small risk. It’s life-threatening.
Same story with atorvastatin (Lipitor) and grapefruit juice. One glass can raise blood levels of the drug by 15 times. That’s not a myth. That’s science. And it wasn’t clear until after the drug hit the market.
What Gets Missed in Trials - And What Shows Up Later
There are three main types of drug interactions that only show up after a drug is widely used:
- Drug-drug interactions: One medication changes how another works. Like warfarin (a blood thinner) interacting with antibiotics - leading to dangerous bleeding.
- Drug-condition interactions: A health condition makes a drug more dangerous. For example, giving certain heart drugs to someone with severe kidney disease can cause sudden heart rhythm problems.
- Drug-food interactions: Food or drink alters how the drug is absorbed. Grapefruit juice is the classic example, but even high-fiber meals can delay absorption of some antidepressants.
According to a 2020 study in PMC, nearly 20% of new drugs got a black box warning - the FDA’s strongest safety alert - after they were already on the market. Four percent were pulled entirely. That’s not rare. That’s the norm.
One of the most shocking cases was benfluorex (sold as Mediator in France). It was prescribed for weight loss and diabetes for over 30 years. Five million people took it. Then researchers found it caused severe heart valve damage. It was pulled in 2009. By then, hundreds had died.
Another example: pergolide, a Parkinson’s drug. After about a million patient-years of use, it was linked to heart valve damage. It was withdrawn in 2007. The problem? It wasn’t obvious in trials because the patients were younger and didn’t take it long enough for the damage to show up.
How We Catch These Problems After Approval
The FDA didn’t wait for disasters to happen. After the thalidomide tragedy in the 1960s, they built systems to track problems after drugs hit the market. Today, that system is called FAERS - the FDA Adverse Event Reporting System. It collects over 2 million reports a year from doctors, pharmacists, patients, and drug companies.
But here’s the catch: only 1% to 5% of actual adverse events get reported. That means for every one report you see, there could be 20 more that never made it in. That’s why the FDA also uses the Sentinel Initiative - a network that tracks health records from over 300 million Americans. It looks for patterns: sudden spikes in hospitalizations for muscle pain, liver failure, or irregular heartbeats after a new drug is prescribed.
AI is now helping too. In January 2023, the FDA approved its first AI-powered system that can scan 10,000 adverse event reports daily and spot hidden patterns. In pilot studies, it cut signal detection time from 18 months to just 45 days.
Pharmacists are on the front lines. Tools like GoodRx and Epocrates now flag dangerous interactions in real time when a prescription is entered. One Reddit user shared how their pharmacist stopped them from taking ciprofloxacin with their blood pressure meds - a combo that could cause fatal heart rhythm issues. That’s the kind of safety net that only exists because of post-market data.
The Real Cost - Lives and Billions
This isn’t just about science. It’s about money and lives.
The Institute of Medicine estimated that adverse drug events cost the U.S. system $3.5 billion a year. About one-third of that - over $1 billion - comes from drug interactions. That’s not just hospital bills. It’s lost workdays, long-term disability, and families shattered by preventable mistakes.
And it’s getting worse. The global pharmacovigilance market - the industry that tracks these risks - grew from $5.8 billion in 2020 to $7.3 billion in 2022. Why? Because regulators now require drug companies to run post-approval studies for nearly half of all new drugs. For 22% of them, that means specifically studying drug interactions.
Big companies like Pfizer and Merck have entire departments dedicated to this. Smaller biotechs often outsource it to firms like Parexel, which made $1.2 billion from pharmacovigilance services in 2022.
What You Can Do to Stay Safe
You can’t rely on your doctor to know every interaction. Even the best clinicians miss things. Here’s what you can do:
- Keep a full list of everything you take - prescriptions, OTC meds, vitamins, herbs, even supplements like melatonin or turmeric. Bring it to every appointment.
- Ask your pharmacist every time you pick up a new prescription. They’re trained to spot interactions and often have more time than your doctor.
- Use free tools like GoodRx, Medscape, or the FDA’s Drug Interaction Checker. Type in your meds and see what pops up.
- Don’t assume natural = safe. St. John’s Wort can reduce the effectiveness of birth control, antidepressants, and even some cancer drugs. One FDA report described a 78-year-old who bled uncontrollably after mixing apixaban (Eliquis) with St. John’s Wort.
- Report side effects. If you feel something off after starting a new drug, report it to the FDA. Your report could save someone else’s life.
The Future: Better, Faster, Smarter
The system is improving. The FDA now requires real-world evidence for 100% of new cancer drugs and 75% of all new therapies within two years of approval. The European Medicines Agency is using machine learning to detect signals faster. And the NIH is launching pharmacogenomics studies to see how your genes affect how you respond to drugs.
By 2025, many drug companies plan to use blockchain to track adverse events - making reporting more secure and accurate. That could cut underreporting from 95% to under 50%.
But here’s the problem: even with all this tech, drug labels still don’t clearly warn patients. Many interaction warnings are buried in tiny print or listed as "rare" when they’re actually common in older adults or people on multiple meds.
Until labels improve, you’re still your own best defense.
Final Thought: The Drug Doesn’t End When It’s Approved
The real test of a drug doesn’t happen in a lab or in a clinical trial. It happens when a grandmother takes it with her grapefruit juice. When a college student mixes it with energy drinks. When a veteran on pain meds starts using CBD oil because he’s tired of side effects.
That’s when the truth comes out. And that’s why post-market surveillance isn’t just bureaucracy - it’s the last line of defense between you and a preventable disaster.
Know your meds. Ask questions. Report what you see. Because the system works - but only if you help it.
How common are drug interactions discovered after a drug is approved?
About one-third of new drugs approved over the past decade had a major safety event after launch - like a black box warning, recall, or safety alert. Nearly 20% received a black box warning, and 4% were pulled from the market entirely. These numbers come from FDA and peer-reviewed studies tracking drug safety over 10+ years.
Can grapefruit juice really make my medication dangerous?
Yes. Grapefruit juice blocks an enzyme in your liver (CYP3A4) that breaks down many drugs. This can cause dangerous buildups. For example, it can raise atorvastatin (Lipitor) levels by up to 15 times, increasing the risk of muscle damage and kidney failure. It affects over 85 medications, including some blood pressure pills, statins, and anti-anxiety drugs. Even one glass can have an effect - and it lasts over 24 hours.
Why don’t drug labels warn about all interactions?
Because many interactions are only discovered after millions of people use the drug. Labels are written based on pre-market data - which is limited. Also, drug companies often downplay risks to protect sales. The FDA can require label updates, but it takes time. That’s why checking interactions yourself with tools like GoodRx or asking your pharmacist is essential.
Are herbal supplements safe to take with prescription drugs?
No - not without checking. St. John’s Wort can make birth control, antidepressants, and blood thinners like Eliquis ineffective. Garlic and ginkgo can increase bleeding risk with warfarin. Turmeric can interfere with diabetes meds. These aren’t rare cases - they’re documented in FDA reports and hospital records. Just because something is "natural" doesn’t mean it’s safe with your prescriptions.
What should I do if I think I’m having a drug interaction?
Stop the suspected drug immediately and call your doctor or pharmacist. If you have symptoms like muscle pain with weakness, unexplained bruising, irregular heartbeat, confusion, or dark urine - go to the ER. Then report it to the FDA through MedWatch. Your report helps improve drug safety for everyone.