Mupirocin Allergy Symptom Checker
This tool helps you assess your symptoms based on key differences between normal irritation and mupirocin allergy. Click "Check My Symptoms" to get a result.
When it comes to treating minor skin infections, Mupirocin is a topical antibiotic ointment that targets gram‑positive bacteria such as Staphylococcus aureus. It’s a go‑to for athletes, parents, and anyone with a small cut that might get infected. But like any medication, it can trigger an allergic response in a small percentage of users. If you ever wonder whether your rash is a normal irritation or a true mupirocin allergy, this guide walks you through the clues, the tests, and the steps to take so you can stop the discomfort fast.
What Exactly Is a Mupirocin Allergy?
A Mupirocin allergy is an immune‑mediated reaction that occurs when your body mistakenly identifies the drug’s active ingredient or one of its excipients as a threat. Most often, the response falls under contact dermatitis, a type‑IV hypersensitivity reaction that shows up hours to days after exposure. Unlike a simple irritation, an allergic response involves immune cells releasing inflammatory chemicals, leading to redness, swelling, and sometimes blistering.
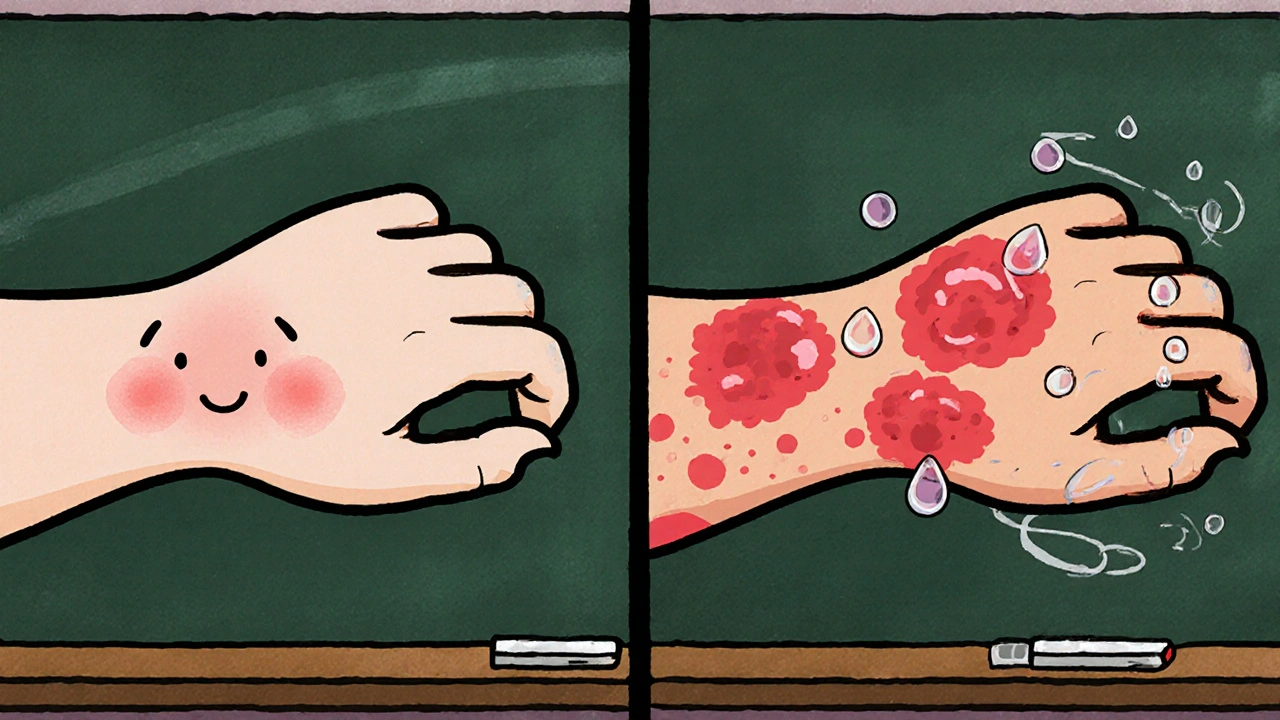
How to Spot the Difference: Typical Irritation vs. Allergy
Everyone who uses mupirocin gets a little warmth or mild redness at the application site-that’s the drug doing its job. An allergy, however, brings extra red flags:
- Onset timing: Irritation appears within minutes, while an allergic rash often shows up 24‑48hours later.
- Spread: A simple irritation stays where you applied the ointment. An allergic reaction can spread to surrounding skin or even distant areas.
- Itchiness: Normal use may feel slightly tingly, but a true allergy is intensely itchy, sometimes with a burning sensation.
- Lesion type: Look for small raised bumps (papules), fluid‑filled blisters (vesicles), or a rash that weeps clear fluid.
- Systemic signs: Though rare, severe reactions can produce fever, swelling of the face or lips, or difficulty breathing-signs you need emergency care.
If you notice any of these, it’s worth investigating further.
Confirming the Allergy: What Tests Do Doctors Use?
Healthcare providers have two main tools to confirm a mupirocin allergy:
- Skin prick test: A tiny drop of diluted mupirocin is placed on the forearm, then the skin is pricked. A positive result shows a raised wheal within 15‑20minutes.
- Patch test: Here, mupirocin is applied to a patch and left on the back for 48hours. The patch is removed and the site is examined after 48 and 72hours for a delayed reaction.
Both tests are safe, low‑risk, and performed by a dermatologist or an allergist. The patch test is especially helpful for type‑IV reactions, which are the most common with topical antibiotics.
First‑Aid Steps When You Suspect an Allergy
Don’t panic, but act quickly to limit the reaction:
- Stop using mupirocin immediately. Wash the area with gentle soap and lukewarm water to remove any leftover ointment.
- Apply a cool compress. A wetted washcloth for 10‑15minutes can soothe itching and reduce swelling.
- Take an over‑the‑counter antihistamine. Cetirizine 10mg or diphenhydramine 25‑50mg can calm the itch.
- Use a mild corticosteroid cream. Hydrocortisone 1% applied two to three times daily helps calm inflammation.
- Monitor for escalation. If the rash spreads rapidly, develops large blisters, or you notice facial swelling, seek emergency care.
Treatment Options for Confirmed Mupirocin Allergy
Once a diagnosis is confirmed, management focuses on symptom relief and preventing future exposure.
- Topical steroids. For moderate reactions, prescription‑strength steroids like triamcinolone 0.1% or betamethasone 0.05% work faster than over‑the‑counter options.
- Systemic antihistamines. For widespread itching, a non‑sedating antihistamine taken twice daily can be more effective.
- Immune‑modulating creams. In chronic cases, calcineurin inhibitors (tacrolimus ointment) may be prescribed.
- Alternative antibiotics. If you still need a topical antibiotic, your doctor might recommend fusidic acid, bacitracin, or a gentamicin‑based cream-agents with different chemical structures and lower cross‑reactivity.
Always keep a written record of the allergy and share it with any future prescribers.
Preventing Future Reactions
Preventing another episode is mostly about awareness:
- Medical alert bracelet. List "Mupirocin allergy" alongside any other drug sensitivities.
- Update your health records. Add the allergy to your electronic medical record (EMR) and ask your pharmacy to flag it.
- Read labels carefully. Some compounded creams may contain mupirocin as a hidden ingredient.
- Discuss alternatives with your clinician. If you need a topical antibiotic for a future wound, ask for a non‑mupirocin option outright.
When to See a Dermatologist or Emergency Care
Most mild reactions settle within a few days with home care, but you should see a professional if:
- The rash covers more than 10% of your body surface.
- Blisters are large, painful, or start oozing pus.
- You develop fever (>100.4°F) or chills.
- Swelling involves the lips, tongue, or throat (possible anaphylaxis).
- Symptoms persist beyond a week despite OTC treatment.
Emergency departments can administer intramuscular epinephrine and IV steroids for severe cases, while dermatologists can run patch testing and prescribe stronger topical agents.
Quick Checklist: What to Do If You Suspect a Mupirocin Allergy
- Stop using the product.
- Wash the area with mild soap.
- Apply cool compresses.
- Take an OTC antihistamine.
- Use hydrocortisone 1% cream.
- Monitor for spreading or systemic symptoms.
- Schedule a skin‑prick or patch test with a dermatologist.
- Document the allergy and share with all healthcare providers.
Comparison Table: Typical Irritation vs. Mupirocin Allergy
| Feature | Normal Irritation | Mupirocin Allergy |
|---|---|---|
| Onset | Minutes to a few hours | 24‑48hours after application |
| Spread | Localized to application site | Can spread beyond site, sometimes distant areas |
| Itch intensity | Mild to moderate | Severe, often described as burning |
| Lesion type | Redness, mild swelling | Papules, vesicles, weeping blisters |
| Systemic signs | None | Fever, facial swelling, shortness of breath (rare) |
Frequently Asked Questions
Can I develop a mupirocin allergy after using it only once?
Yes. Allergic sensitization can occur after a single exposure if your immune system is primed to react to a component of the ointment.
Is a rash after mupirocin always an allergy?
No. Mild redness or a stinging sensation is common and usually not allergic. Look for the timing, spread, and intensity clues described above.
Do I need a prescription to get a skin‑prick or patch test?
A referral from your primary‑care doctor is typical, but many dermatology clinics accept self‑referrals for contact‑dermatitis testing.
Can I use over‑the‑counter antibiotic ointments as a substitute?
OTC options like bacitracin or polysporin contain different active ingredients and are generally safe for someone allergic to mupirocin, but check the label for other potential allergens.
What should I do if I develop swelling of the lips or tongue?
That’s a possible anaphylactic reaction. Call 911 or go to the nearest emergency department immediately; epinephrine is life‑saving.
Is there a way to test for mupirocin allergy at home?
Home testing isn’t reliable. Only a dermatologist can perform a skin‑prick or patch test that accurately identifies the allergy.
Will I need to avoid all antibiotics if I’m allergic to mupirocin?
No. The allergy is specific to mupirocin’s chemical class (monoxycarb‑pyrrolidone). Other antibiotic families, like macrolides or fluoroquinolones, are typically safe unless you have a documented cross‑reactivity.











Beverly Pace
October 16, 2025 AT 14:47 PMWe all have a duty to treat our bodies like temples, and that means taking drug reactions seriously. If you suspect a mupirocin allergy, stop the ointment immediately and wash the area with mild soap. Keep a detailed log of the symptoms, timing, and any over‑the‑counter meds you used. Share that log with your dermatologist so they can decide whether a patch test is warranted. Ignoring early signs can lead to bigger problems down the line.
RALPH O'NEIL
October 16, 2025 AT 16:30 PMIt's useful to remember that not every rash after applying a cream is an allergy; the timing and spread are key clues. A localized redness that shows up within minutes is usually harmless, while a delayed, spreading itch warrants a closer look. Documenting those details helps the clinician differentiate irritation from a true hypersensitivity.
Mark Wellman
October 16, 2025 AT 20:40 PMOkay, so here's the thing: I was using mupirocin on a small cut on my knee and thought everything was fine until, like, two days later, my skin started acting up big time. First, there was this mild itch that I brushed off, but then the area turned bright red and started to swell, and I could feel this weird burning sensation that just wouldn't quit. By the third day, I noticed tiny blisters forming around the original spot, and they were oozing clear fluid, which was both gross and concerning. I tried washing it with gentle soap and even slapped on a cheap hydrocortisone cream I had at home, but the rash just kept spreading to the surrounding thigh. I read up that a real mupirocin allergy is a type‑IV hypersensitivity, meaning the immune system is overreacting to the drug itself or one of its additives, and that can take 24‑48 hours to manifest, which totally matches what I experienced. The itching got so intense that I started scratching, and that only made it worse, turning the rash into a patchwork of raised bumps and painful vesicles. I also felt a low‑grade fever kicking in, which is a red flag that the reaction might be systemic, not just a local irritant. I was lucky enough to get an appointment with a dermatologist who performed a patch test: they stuck a small piece of mupirocin‑infused tape on my back for 48 hours and then checked the spot for any delayed reaction. Sure enough, the test site was inflamed, confirming the allergy. The doc prescribed a stronger topical steroid, and I was also told to avoid all mupirocin‑containing products moving forward, even those that might be in compounded creams. They suggested alternatives like bacitracin or fusidic acid for future infections, which have a different chemical structure and are less likely to cause cross‑reactivity. I now carry a medical alert card that lists my mupirocin allergy, and I've updated my pharmacy profile so they flag the medication. Bottom line: if you notice a rash that appears a day or two after applying mupirocin, especially if it spreads, it’s time to act fast-stop the ointment, wash the area, use an antihistamine, and see a professional for testing.
Carl Boel
October 17, 2025 AT 02:13 AMFrom a clinical pharmacology perspective, the immunogenic potential of mupirocin is mediated by its methyl‑propionic acid moiety, which can act as a hapten when conjugated with dermal proteins, precipitating a delayed‑type hypersensitivity cascade. Such mechanistic insight underscores the necessity of precise diagnostic modalities like epicutaneous patch testing to delineate true allergic sensitization from mere irritant dermatitis.
Shuvam Roy
October 17, 2025 AT 13:20 PMThank you for sharing this comprehensive guide. It is reassuring to know that simple first‑aid steps-discontinuing the ointment, gentle cleansing, and applying a cool compress-can alleviate many symptoms while awaiting professional evaluation. I appreciate the emphasis on documenting the reaction and informing all healthcare providers to prevent future exposure.
Jane Grimm
October 18, 2025 AT 03:13 AMIt is advisable to document any adverse reaction promptly.
Eve Perron
October 18, 2025 AT 17:06 PMWhen assessing a potential mupirocin allergy, one must consider both the clinical presentation and the sociocultural context of the patient. The timing of symptom onset-typically 24 to 48 hours post‑application-distinguishes it from an immediate irritant reaction; however, patients from diverse backgrounds may interpret itching differently based on cultural norms. Moreover, the language used in medical documentation should reflect precision without alienating the individual; for instance, describing "papular eruptions" rather than "rashes" can convey a more exact dermatologic picture. It is also essential to recognize that access to patch testing facilities varies globally, and tele‑dermatology may serve as an interim solution for those in underserved regions. By integrating these considerations, clinicians can foster a more inclusive, accurate, and patient‑centered approach to allergic assessment.
Danielle Flemming
October 19, 2025 AT 20:53 PMHey folks, just wanted to say great post! If you ever get a weird rash from mupirocin, don’t freak out-stop using it, slap on some cool water, and hit up a doc if it gets worse. You’ll be back to feeling awesome in no time.
Anna Österlund
October 20, 2025 AT 02:26 AMHonestly, if you’re scared of a little rash, just pull the plug on the ointment and move on-no need to over‑dramatize it.
Erynn Rhode
October 21, 2025 AT 00:40 AMGreat rundown! 😊 I’d add that keeping a photo diary of the skin changes can be super helpful when you finally see a dermatologist-visual evidence often speeds up the diagnosis. Also, for those who prefer natural soothing, a colloidal oatmeal bath can provide additional itch relief alongside the standard OTC antihistamines.
Anuj Ariyo
January 3, 2026 AT 13:47 PMInteresting points. The patch test you described is indeed the gold standard for confirming delayed hypersensitivity, and it’s reassuring that the procedure is low‑risk and straightforward.