When you pick up your prescription, the label on the bottle isn’t just a piece of paper-it’s your first and most reliable line of defense against dangerous medication errors. Every name, number, and phone number printed there exists for one reason: to keep you safe. But most people glance at it, toss it in their bag, and move on. That’s a mistake. Verifying the prescriber and pharmacy information on your label takes less than a minute, but it can stop a life-threatening error before it starts.
Why This Step Isn’t Optional
Every year, over 1.3 million people in the U.S. are injured because of medication mistakes, and more than 7,000 die. About 12% of those errors come from incorrect or unclear prescriber information on the label. That means nearly one in eight of these preventable harms happens because someone didn’t check who ordered the medicine or where it came from. The FDA and the Institute for Safe Medication Practices (ISMP) have been clear: if you don’t verify the prescriber name and pharmacy details, you’re skipping the most basic safety check in the entire medication process. A 2023 study found that patients who consistently checked their labels reduced their risk of medication errors by 32%. That’s not a small number. It’s the difference between taking your heart pill and accidentally getting a blood thinner meant for someone else.What to Look For on the Label
Your prescription label has to include specific information by law. Don’t assume it’s right-check it. Here’s what you need to confirm:- Prescriber’s full name - This should match exactly who you saw. If your cardiologist prescribed it, the label shouldn’t say “Dr. James Wilson” when your doctor is “Dr. Lisa Wilson.” Misspellings happen, especially with electronic prescriptions.
- NPI number - This is a unique 10-digit identifier for every licensed provider. It’s usually printed near the prescriber’s name. If you’re unsure, call the pharmacy and ask them to read it back to you.
- Prescription number - This is the number you’ll use when calling for refills. Write it down in your phone or a notebook. If the number doesn’t match what your doctor’s office gave you, ask why.
- Pharmacy name and address - Make sure it’s the pharmacy you intended to use. If you ordered from a mail-order service, the label should say so clearly. If it says “CVS Pharmacy” but you picked it up at Walgreens, that’s a red flag.
- Pharmacy phone number - This is your lifeline. If something feels off, call this number. Don’t wait. Pharmacists are trained to catch these errors.
- Pharmacist’s name - In 42 states, this is required by law. Seeing a name you recognize adds another layer of trust.
When to Verify - Three Critical Moments
Don’t wait until you’re ready to take your pill. Check the label at three points:- When you first receive it - Right at the counter. Don’t leave the pharmacy until you’ve confirmed the details. If you’re unsure, ask the pharmacist to walk you through it.
- Before your first dose - Even if you thought everything looked right, take another look. Fatigue, stress, or distractions can make you miss small errors.
- Every time you refill - Prescriptions can get mixed up in the system. A refill might come from a different pharmacy, or the prescriber info might auto-fill wrong. Always check.
Common Mistakes and Real Cases
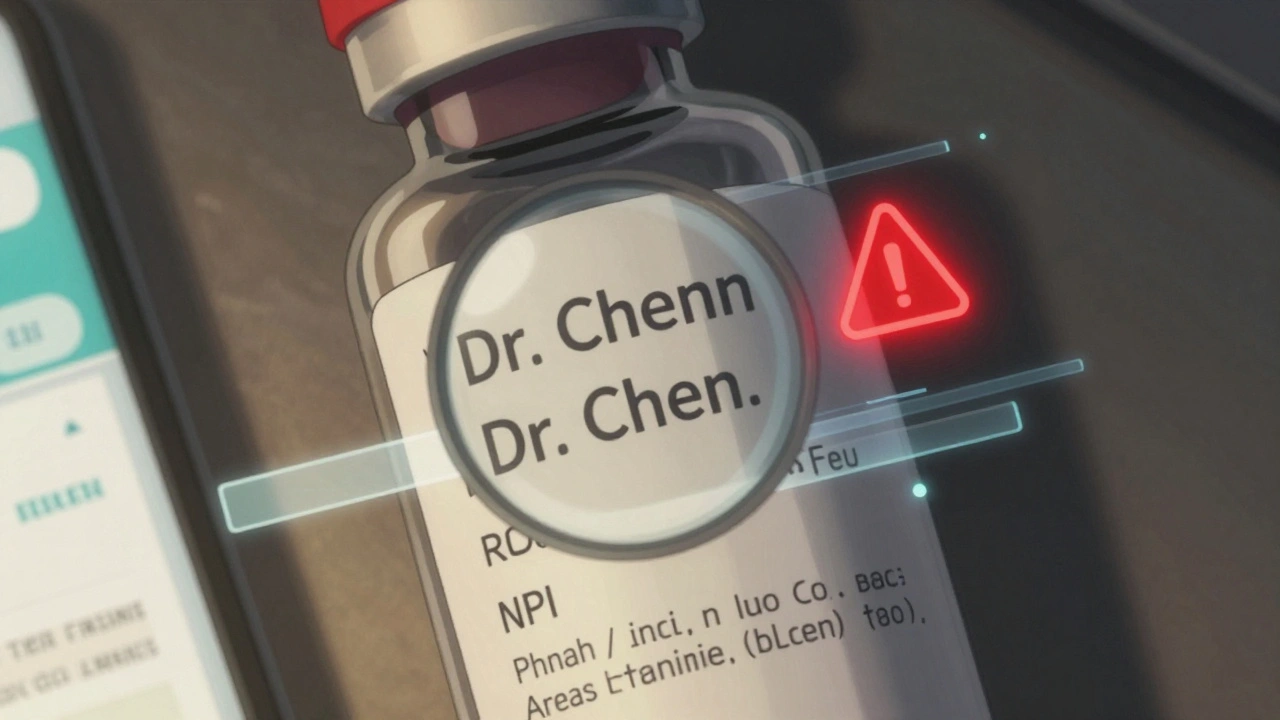
Errors aren’t rare. A Reddit thread with over 1,200 comments from patients revealed that 68% of people who regularly checked their labels caught at least one mistake in the past year. The top two issues:- Misspelled prescriber names - 42% of reported errors. “Dr. Chen” becomes “Dr. Chen” with an extra ‘n’ or “Dr. Chenn.” Sounds harmless, but if you’re on a controlled substance, a mismatch can trigger a pharmacy hold or even a DEA alert.
- Wrong prescriber specialty - 28% of errors. A patient got a Schedule II opioid prescribed by a dentist, but the label listed their primary care doctor. That’s a red flag-dentists don’t usually prescribe long-term opioids, and the system flagged it as a possible mix-up.
Why Digital Tools Aren’t Enough
Pharmacy apps, QR codes, and online portals are convenient. But they’re not foolproof. A 2023 study in the Journal of the American Pharmacists Association found that patients using mobile apps to verify their prescriptions had a 7.2% error rate. Those who checked the physical label had only a 2.1% error rate. Why? Because apps can glitch. They can show outdated info. They can auto-fill the wrong provider. And if your phone dies or you’re in a hurry, you can’t use them. The paper label? It’s always there. It doesn’t need Wi-Fi. It doesn’t need a battery. It’s your backup system. The FDA’s 2024 pilot program is testing QR codes on labels that link to digital verification pages. Early results show a 19% improvement in accuracy-but they still recommend patients double-check the printed info. Technology helps. It doesn’t replace you.What to Do If Something’s Wrong
If you spot a mismatch:- Don’t take the medication. Even if it looks right, don’t risk it.
- Call the pharmacy immediately. Use the number on the label. Ask to speak to the pharmacist, not a technician.
- Ask for the original prescription record. They’re required to keep it on file. You have the right to see it.
- Call your prescriber’s office. Confirm they sent the prescription to that pharmacy for that medication.
- Report it. If the error wasn’t your fault, report it to the pharmacy’s customer service and to the FDA’s MedWatch program. Your report helps fix system-wide problems.

Tools to Help You Stay on Track
You don’t have to remember everything. Use these simple tools:- Personal Medication Record (PMR) - Keep a list of all your meds, dosages, prescribers, and pharmacy info. Update it every time something changes. Most major pharmacies like CVS and Walgreens offer free digital PMRs in their apps.
- Magnifying glass or phone flashlight - If the print is too small (a problem for 37% of people over 65), ask your pharmacy for a magnifier. Over 80% of pharmacies give them out for free.
- Ask for help spelling names - If you’re not sure if “Dr. Kwan” is spelled right, ask the pharmacist to say it out loud. They’re used to it.
Who’s Responsible?
Some people think, “It’s the pharmacy’s job to get this right.” And yes, they’re legally required to. But the FDA, ISMP, and The Joint Commission all say: the patient is the last line of defense. Pharmacies make mistakes. Systems glitch. Prescribers get misidentified in electronic records. You’re not being difficult-you’re being smart. A 2023 survey of 5,000 patients found that those who verified their labels had 27% fewer medication errors and 31% higher adherence rates. They didn’t just avoid harm-they took their meds correctly more often because they felt confident they had the right one.Final Reminder
You don’t need to be a doctor or a pharmacist to protect yourself. You just need to pause. Look. Read. Question. It takes 60 to 90 seconds per label. That’s less time than it takes to scroll through one social media post. The next time you get a prescription, don’t rush. Sit down. Hold the label up to the light. Read every word. If anything feels off, call. You’re not being paranoid. You’re being safe.What if the prescriber name on my label is misspelled?
Even a small misspelling-like “Dr. Smith” instead of “Dr. Smyth”-can signal a mix-up in the system. Don’t ignore it. Call the pharmacy right away and ask them to verify the original prescription record. It’s a common error with electronic prescribing, and pharmacists are trained to fix it quickly. Never take the medication until you’re sure the name matches who prescribed it.
Can I trust the pharmacy’s mobile app instead of the label?
Apps are helpful for reminders and refills, but they’re not a replacement for checking the physical label. A 2023 study showed that 7.2% of users relying only on apps missed errors, compared to just 2.1% who checked the printed label. Apps can show outdated info, have glitches, or auto-fill the wrong prescriber. Always compare the app to the label before taking your medicine.
Why does my label show a different pharmacy than the one I went to?
This usually happens if your prescription was filled by a mail-order pharmacy or a partner pharmacy contracted by your insurance. It’s not always a mistake-but you should still verify the name, address, and phone number match the service you signed up for. If it doesn’t, call your insurance provider and your prescriber’s office to confirm the prescription was sent correctly.
Is it normal for the pharmacist’s name to be missing from the label?
In 8 out of 50 states, the pharmacist’s name is not required on the label. But in 42 states, it is. If you’re in a state that requires it and the name is missing, contact the pharmacy. It doesn’t mean the prescription is wrong-but it’s a sign the label may not have been fully reviewed. Ask to speak to the pharmacist directly before taking the medication.
How often should I update my personal medication record?
Update your record every time you start, stop, or change the dose of any medication-even over-the-counter drugs or supplements. Keep it in your phone, wallet, or with a family member. Many pharmacies offer free digital versions through their apps. Having this record makes verifying your label much easier and helps you communicate with doctors during emergencies.








Eddie Bennett
December 11, 2025 AT 15:25 PMJust picked up my blood pressure med today and caught that the prescriber name was misspelled. Called the pharmacy right away-they fixed it in 2 minutes. Seriously, take 30 seconds to look. It’s not paranoia, it’s survival.
Kristi Pope
December 13, 2025 AT 05:11 AMI used to skip this step too-until my grandma almost took someone else’s chemo pill. Now I check every label like it’s a bomb defusal. It’s not a hassle, it’s a habit. And if you’re too busy, ask the pharmacist to walk you through it. They don’t mind. Seriously, they’ve seen it all.
Courtney Blake
December 14, 2025 AT 04:12 AMOf course the FDA wants you to check labels. They don’t want you to trust the system because the system is broken. Pharmacies are understaffed, EHRs are garbage, and the whole thing’s a money-driven circus. But hey, at least you can feel good about reading tiny print while your insurance hikes your copay again.
Kaitlynn nail
December 15, 2025 AT 10:28 AMReality is just a label away, man. The paper is the only truth left in a digital lie.
Jack Appleby
December 16, 2025 AT 05:51 AMIt’s amusing how this post treats checking a label like some revolutionary act. The FDA and ISMP have been screaming this for two decades. The real issue is that pharmacies still use 1990s barcode systems that swap NPI numbers like it’s a game of musical chairs. You’re not a hero for reading text-you’re just not a statistic yet.
Michelle Edwards
December 17, 2025 AT 00:05 AMMy mom’s 78 and she does this every time. I used to roll my eyes. Now I do it with her. We even keep a little checklist taped to the medicine cabinet. It’s not about being paranoid-it’s about being together. Small things keep us safe.
Lisa Stringfellow
December 18, 2025 AT 18:55 PMSo let me get this straight-you’re telling me I need to verify a 10-digit number on a tiny label that’s printed by a machine that’s been running since the Bush administration… and if I don’t, I’ll die? Wow. What a shock. Next you’ll tell me to check the expiration date on my toothpaste too.
Frank Nouwens
December 20, 2025 AT 05:40 AMWhile the sentiment expressed herein is commendable, one must acknowledge the structural inefficiencies inherent in the current pharmaceutical distribution model. The onus placed upon the layperson to perform quality control functions traditionally within the purview of licensed professionals represents a systemic abdication of responsibility. One may verify, but one should not be required to.
Rebecca Dong
December 21, 2025 AT 03:16 AMWhat if the label is fake? What if the whole pharmacy system is a front for the government to track what meds you’re taking? I read a guy on YouTube who said the NPI number is actually a chip that sends your DNA to the CIA. I checked my label last week-my pharmacist’s name was ‘Agent Smith.’ Coincidence? I think not.
Katherine Liu-Bevan
December 22, 2025 AT 13:56 PMI work in pharmacy administration. We get 3-5 mislabeled prescriptions a day. Most are due to EHR auto-fill errors or duplicate patient records. We catch most before they leave the counter, but not all. The ones that slip through? They’re usually the ones where the patient didn’t look. If you’re reading this and you’ve never checked your label-start today. It’s not about trust. It’s about verification. And if you’re ever unsure, ask. We’re here to help, not judge.
Doris Lee
December 24, 2025 AT 05:56 AMMy dad had a stroke last year. We found out his blood thinner was switched to a diabetes med because the label said ‘Dr. Tran’ instead of ‘Dr. Tran.’ Same last name, different person. He’s fine now. But I’ll never not check again. Seriously, just look. It’s free. It’s easy. It’s everything.