Mood Stabilizer Interaction Checker
Check Interactions
Select your medications to see interaction risks.
When you're managing bipolar disorder, finding the right mood stabilizer isn't just about controlling highs and lows-it's about keeping your whole system balanced. Lithium, valproate, and carbamazepine have been the backbone of treatment for decades. But here’s the catch: they don’t play well with everything else you might be taking. A simple over-the-counter painkiller, a blood pressure med, or even another psychiatric drug can turn a stable dose into a dangerous one. These aren’t theoretical risks. Real people end up in the ER because of them.
Lithium: The Delicate Balance
Lithium is old-school, cheap, and effective-but it’s also the most finicky. Your body gets rid of it almost entirely through your kidneys. That means anything that changes how your kidneys work can cause lithium to build up to toxic levels. Common medications like ibuprofen, naproxen, and even some blood pressure drugs like lisinopril can increase lithium levels by 25% to 40% within days. One patient on Reddit described going from feeling fine to trembling and confused after starting ibuprofen for a headache. Their lithium level jumped from 0.8 to 1.3 mmol/L-right into the danger zone.
Thiazide diuretics are especially risky. They make you pee more, but they also make your kidneys hold onto lithium instead of flushing it out. A 1983 study showed lithium levels rising by up to 40% in patients on these drugs. Even mild dehydration-like from a hot day or skipping water-can push levels higher. That’s why doctors tell people on lithium to drink plenty of fluids and avoid extreme salt loss. If you’re on lithium and start a new medication, your doctor should check your blood level within 5 to 7 days. The goal? Keep it between 0.6 and 0.8 mmol/L when you’re on other drugs, not the usual 0.8 to 1.2.
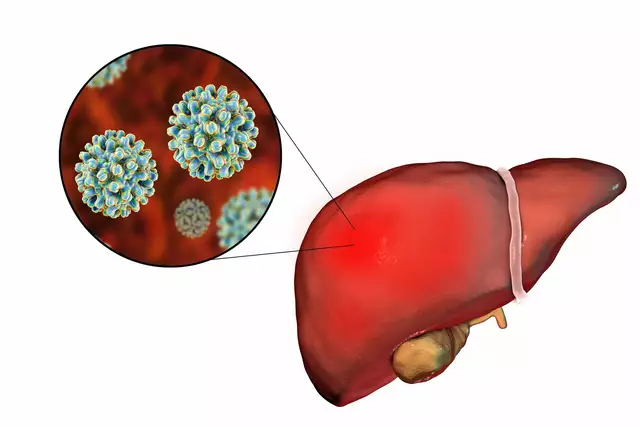
Valproate: The Hidden Triggers
Valproate (or valproic acid) works differently. It’s metabolized in the liver through multiple pathways, which makes it less likely to cause problems from single enzyme changes. But it’s still a troublemaker in two big ways: it boosts levels of other drugs and gets pushed down by others.
Take lamotrigine, a common mood stabilizer used with valproate. When you add valproate to lamotrigine, the lamotrigine level can double or even triple. That’s why doctors often cut lamotrigine doses in half when starting valproate. One patient on r/BipolarReddit shared that switching from carbamazepine to valproate forced their lamotrigine dose down from 400 mg to 200 mg. Without that adjustment, they could’ve had a serious rash or worse.
On the flip side, carbamazepine can slash valproate levels by 30% to 50%. That’s because carbamazepine turns on liver enzymes that break down valproate faster. So if you’re on both, your valproate might stop working. You might start feeling manic again-not because your illness is worsening, but because your drug level dropped. That’s why doctors monitor both drugs when they’re used together. And don’t forget: valproate carries a serious FDA warning. For women who could get pregnant, it raises the risk of birth defects by more than 10%-nearly 4 times higher than normal. That’s why many avoid it unless absolutely necessary.
Carbamazepine: The Enzyme Engine
Carbamazepine is like a metabolic bulldozer. It forces your liver to produce more of the CYP3A4 enzyme, which breaks down a whole list of drugs. Within 3 to 5 weeks of starting it, your body starts clearing other medications faster-sometimes way faster. That’s why people on carbamazepine often need higher doses of things like risperidone, haloperidol, or birth control pills. One study showed oral contraceptives became 50% to 70% less effective. That’s not a small risk.
But here’s the twist: when you add valproate to carbamazepine, things get weird. Valproate doesn’t lower carbamazepine levels-it actually makes its toxic metabolite, carbamazepine-epoxide, rise by 40% to 60%. This metabolite causes dizziness, nausea, and trouble walking. So even if your carbamazepine level looks fine, you could still feel awful. That’s why experts now recommend checking both the parent drug and the epoxide level when these two are combined. The target epoxide level? Below 3.5 mcg/mL. If it’s higher, you need to lower the carbamazepine dose by about 25%.
Carbamazepine also has a genetic side. Some people have a gene variation that makes them metabolize it poorly, leading to buildup and toxicity. Others have a version that breaks it down too fast, making it ineffective. That’s why more clinics are starting to test for these genes before prescribing it.
What Happens When You Mix Them?
Combining all three? That’s rare-and risky. Lithium and valproate together can be effective for rapid-cycling bipolar disorder, but only if levels are watched closely. One case study followed a patient for 18 months on both drugs without issues, but their lithium was kept low (0.8 mmol/L) and valproate was monitored weekly. That’s not typical.
Carbamazepine and lithium? Less common. Carbamazepine doesn’t directly affect lithium levels, but because it can cause dehydration or kidney stress, it indirectly raises lithium risk. And if you’re on carbamazepine and start lithium, your doctor needs to watch for signs of kidney strain-like low sodium or high creatinine.
Valproate and carbamazepine? The most documented combo, and the most complex. The epoxide buildup is real. Patients often report brain fog, unsteady walking, or nausea even when blood levels look normal. That’s why many psychiatrists avoid this combo unless no other option exists.
What You Need to Do
If you’re on one of these drugs, here’s what you must do:
- Keep a full list of every medication-prescription, OTC, supplements, even herbal teas. Bring it to every appointment.
- Never start or stop anything without talking to your prescriber. Even aspirin or ibuprofen can be dangerous with lithium.
- Know your warning signs. For lithium: tremors, confusion, nausea, frequent urination. For valproate: drowsiness, swelling, bruising. For carbamazepine: dizziness, double vision, rash.
- Get regular blood tests. Lithium: every 3-6 months. Valproate and carbamazepine: every 2-3 months when starting or changing doses.
- Ask about alternatives. Lamotrigine, lurasidone, or quetiapine have fewer interactions and are now first-line for many. Why stick with a drug that needs constant babysitting?

Why This Matters Now
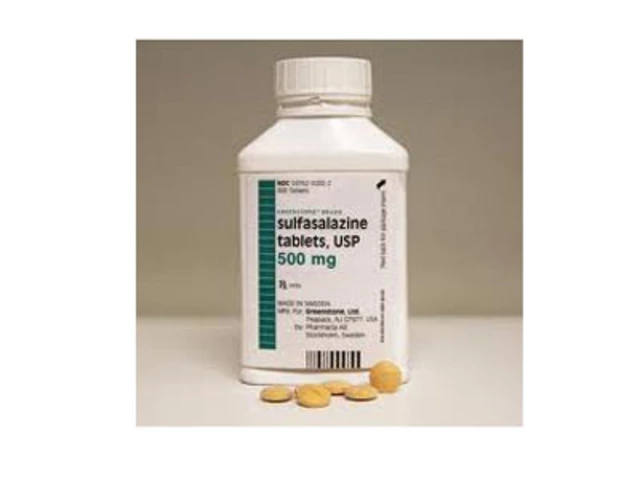
Prescriptions for lithium have dropped from 35% of new mood stabilizer starts in 2012 to just 15% today. Valproate’s use has fallen too-mostly because of pregnancy risks. Carbamazepine holds steady at 10%, but its reputation is shaky. Meanwhile, newer drugs like lamotrigine and lurasidone are climbing fast. Why? Because they don’t play musical chairs with your liver and kidneys.
But here’s the truth: many people still rely on these older drugs. They work. They’re affordable. Lithium costs $30 a month. Valproate is $150. Carbamazepine is $200. Brand-name versions cost more. For people without good insurance, the choice isn’t always about safety-it’s about what they can afford.
That’s why understanding these interactions isn’t just academic. It’s survival. A single missed blood test, a pharmacy mix-up, or a doctor’s oversight can lead to hospitalization. You don’t need to be a pharmacist to protect yourself. You just need to know what to ask for-and when to push back.
Can I take ibuprofen with lithium?
No-not without close monitoring. Ibuprofen and other NSAIDs can raise lithium levels by 25% to 30%, increasing the risk of toxicity. Symptoms include tremors, confusion, nausea, and dizziness. If you need pain relief, acetaminophen (Tylenol) is safer. If you must use ibuprofen, your doctor should check your lithium level within 5 to 7 days and may lower your lithium dose.
Why does valproate make lamotrigine levels go up?
Valproate blocks the enzyme (UGT) that breaks down lamotrigine. This causes lamotrigine to build up in your blood-sometimes doubling or tripling its level. That raises your risk of a serious skin rash called SJS. That’s why doctors usually cut lamotrigine doses in half when starting valproate. Never adjust this yourself.
Can carbamazepine and valproate be used together safely?
They can be used together, but it’s risky. Valproate increases the toxic metabolite of carbamazepine (CBZ-E) by 40% to 60%, even if carbamazepine levels look normal. This can cause dizziness, loss of coordination, and nausea. If you’re on both, your doctor should monitor both drugs and the CBZ-E level. Often, the carbamazepine dose is reduced by 25% when valproate is added. Many doctors avoid this combo unless other options have failed.
What’s the safest mood stabilizer with the fewest interactions?
Lamotrigine is generally the safest in terms of drug interactions. It doesn’t affect liver enzymes and isn’t affected by most other drugs-except valproate, which raises its levels. Lurasidone and quetiapine also have fewer interactions than lithium, valproate, or carbamazepine. But they’re more expensive. The safest choice depends on your medical history, gender, and other conditions-not just interaction risk.
Do I need blood tests if I feel fine?
Yes. Lithium toxicity can happen slowly. You might feel fine until your level hits 1.5 mmol/L-then you suddenly get seizures or kidney damage. Valproate and carbamazepine can cause liver damage or low platelets without symptoms. Regular blood tests are non-negotiable. For lithium, test every 3-6 months. For valproate and carbamazepine, test every 2-3 months when stable. More often if you’re starting a new drug.
Can I switch from carbamazepine to lamotrigine without problems?
Yes, but slowly. Carbamazepine speeds up how fast your body clears lamotrigine. If you stop carbamazepine too fast, your lamotrigine level will spike, raising your risk of a dangerous rash. Your doctor should gradually reduce carbamazepine while slowly increasing lamotrigine over weeks. Never switch cold turkey. This process takes 4 to 8 weeks.
What Comes Next
Research is moving fast. Genetic tests for CYP3A4 and EPHX1 genes are already being used in some clinics to predict how you’ll react to carbamazepine. New extended-release lithium formulations are reducing the peaks and valleys that make interactions worse. And by 2027, pharmacogenetic testing may become standard before prescribing carbamazepine.
But until then, the rules haven’t changed: know your drugs. Know your levels. Know your body. And never assume a new medication is safe just because it’s not psychiatric. The biggest dangers aren’t the big-name drugs-they’re the ones you pick up without thinking. A bottle of Advil. A new blood pressure pill. A friend’s suggestion to try melatonin.
Your brain is already working hard to stay balanced. Don’t let a simple interaction undo it.









Cecelia Alta
January 12, 2026 AT 13:48 PMOkay but like… why is lithium still a thing? I get it’s cheap, but my cousin went to the ER because she took ibuprofen for a cramp and ended up with tremors and confusion for three days. Her doctor didn’t even check her levels until it was too late. Why aren’t we just using lamotrigine for everyone? It’s not perfect but at least you don’t need a PhD in pharmacology to not kill yourself.
And don’t even get me started on valproate and pregnancy. I know it works, but if you’re a woman who could ever get pregnant, why risk it? Like, the FDA warning should be on the bottle in neon lights, not buried in a footnote.
Also, why do doctors still prescribe carbamazepine like it’s 2005? My neurologist switched me to lurasidone last year and I finally slept through the night without feeling like my brain was made of wet cardboard. It’s not magic, but it’s not a minefield either.
steve ker
January 14, 2026 AT 06:07 AMLithium is outdated. Valproate is dangerous. Carbamazepine is a mess. Lamotrigine is the only sane choice. End of story
George Bridges
January 14, 2026 AT 07:59 AMI appreciate how detailed this is. I’ve been on lithium for 12 years and honestly, the biggest thing I’ve learned is that consistency matters more than anything. Same salt intake. Same water. Same sleep schedule. Even small changes throw me off.
My doctor always says lithium isn’t the drug-it’s the routine around it. And that’s true. I’ve had friends switch to newer meds and still struggle because they didn’t build the same structure. It’s not just chemistry, it’s lifestyle.
Also, I never take NSAIDs. Not even aspirin. I keep Tylenol in my bag like it’s my lifeline. And I check my levels every 3 months like clockwork. No excuses.
Faith Wright
January 15, 2026 AT 03:20 AMOh honey. You think this is bad? Try being a woman on valproate and having your OB-GYN act like you’re trying to poison your future baby. I was on it for 5 years, stable as hell, and every time I mentioned wanting kids, I got the side-eye like I was planning a cult.
Meanwhile, my brother’s on carbamazepine and his doc just shrugs when he asks about birth control. Like, you’re fine. Until you’re not.
And don’t even get me started on how pharmacies mix up the names. I once got lamotrigine instead of lithium by accident. Took me 3 days to realize I was floating into a manic fog. That’s not a typo. That’s negligence.
Rebekah Cobbson
January 16, 2026 AT 20:34 PMThis is the kind of post I wish I’d read 10 years ago. I was on lithium and started a new blood pressure med without telling my psych. Thought it was ‘just a pill’. Two weeks later I was dizzy, nauseous, and couldn’t hold a spoon.
My doctor said I was lucky I didn’t have seizures. I didn’t even know lithium levels needed checking. I thought if I felt okay, I was fine.
Now I have a little notebook. Every med. Every supplement. Every change. I show it to every provider. Even the dentist. Because I learned the hard way that ‘just a little Advil’ can be a disaster.
If you’re on one of these meds, please, please, please don’t wait until you’re in crisis to learn this stuff. You’re not being paranoid. You’re being smart.
Audu ikhlas
January 17, 2026 AT 18:57 PMUSA always think they own medicine. In Nigeria we use traditional herbs and never get sick from pills. Lithium? Valproate? Too much science. Our ancestors knew better. You people are weak. Take ginger and be done
Sonal Guha
January 18, 2026 AT 07:30 AMLithium levels are a joke. Doctors check them once a year. People die. Valproate is a teratogen. Carbamazepine causes liver failure. Lamotrigine is the only viable option. Everything else is medical malpractice waiting to happen
Jay Powers
January 19, 2026 AT 16:29 PMI’ve been on carbamazepine for 8 years and honestly, I didn’t know about the epoxide thing until last year. My neurologist finally checked it and my levels were through the roof. No wonder I felt like I was walking through molasses.
They dropped my dose by 25% and I swear I got my brain back. I could focus again. No more dizziness. I didn’t even know it was a thing.
So if you’re on carbamazepine and feel off but your levels look fine? Ask for the epoxide test. It’s not standard, but it should be. And if your doctor doesn’t know what you’re talking about? Find someone who does.
Lawrence Jung
January 21, 2026 AT 01:03 AMThe real tragedy isn’t the drugs-it’s the system. We treat mental illness like a math problem. Take pill A, monitor level B, avoid drug C. But the person? The human? The one who’s scared, tired, broke? They’re just a variable in the equation.
Lithium costs $30. But the blood tests? The specialist visits? The time off work? That’s the real price. And if you’re poor? You’re not just at risk for toxicity-you’re at risk for being ignored.
We don’t need more science. We need more humanity.
Alice Elanora Shepherd
January 22, 2026 AT 09:55 AMThank you for this incredibly thorough breakdown. I’ve been a psychiatric nurse for 17 years, and I still learn something new every time I read a post like this.
One thing I’d add: when patients are on valproate + carbamazepine, the epoxide toxicity can be silent. They don’t feel ‘sick’-they just feel ‘off’. Slower. Foggy. Irritable. And they assume it’s their illness flaring. It’s not. It’s the drug combo.
Also-please, please, please: if you’re on lamotrigine and your doctor suddenly adds valproate, don’t assume the dose is fine. Double-check. Ask for a level. And if they say ‘it’s fine, you’re fine’-get a second opinion.
This isn’t paranoia. This is how people survive.
Christina Widodo
January 23, 2026 AT 21:23 PMWait so if I’m on lithium and I take ibuprofen, I need a blood test in 5-7 days? What if I can’t afford it? What if my insurance won’t cover it? What if my doctor’s office is closed? This isn’t just medical advice-it’s a privilege. Not everyone can afford to be this careful.
Prachi Chauhan
January 24, 2026 AT 13:57 PMPeople talk about drugs like they’re magic wands. But the truth? The brain doesn’t care about labels. It cares about balance. Lithium? It’s not the drug. It’s the rhythm. The water. The salt. The sleep. The quiet mornings.
I used to think I needed a new pill every time I felt off. Turns out, I just needed to drink more water and stop drinking coffee after 2pm.
Maybe the real medicine isn’t in the bottle. Maybe it’s in the routine. In the stillness. In the choice to not reach for the Advil.
Just saying.
Katherine Carlock
January 25, 2026 AT 03:21 AMI’ve been on lamotrigine for 6 years and honestly? It’s the first thing that didn’t make me feel like a lab rat.
My mom’s on lithium and she checks her levels religiously. She has a little calendar with red X’s. I thought it was overkill. Now I get it.
Also-my cousin took melatonin because she ‘wanted to sleep better’. Didn’t tell anyone. Got admitted for lithium toxicity. She was 24.
So yeah. Even ‘harmless’ stuff? Not harmless. Please, just talk to your doctor. Even if it’s embarrassing. Even if you think it’s stupid. It’s not.
Sona Chandra
January 27, 2026 AT 00:01 AMTHIS IS WHY PEOPLE DIE. EVERY SINGLE DAY. SOMEONE TAKES IBUPROFEN AND THINKS IT’S HARMLESS. THEN THEY’RE IN THE ER. THEN THEIR FAMILY BLAMES THEM. THEN THE DOCTOR SAYS ‘I DIDN’T KNOW’. NO. YOU DID. YOU KNEW. YOU JUST DIDN’T CARE ENOUGH TO TELL THEM.
Jennifer Phelps
January 27, 2026 AT 17:38 PMSo if I’m on carbamazepine and start lamotrigine… I have to wean off carbamazepine slowly? And ramp up lamotrigine slowly? Like… over weeks? Why isn’t this on the pill bottle? Why do I have to Google this? Why isn’t my pharmacist telling me?