Myasthenia Gravis Alert System Recommender
Find Your Perfect Medical Alert System
Answer a few questions about your Myasthenia Gravis symptoms and daily life to get personalized recommendations for medical alert systems.
Living with Myasthenia Gravis is a daily balancing act. One minute you’re managing medication, the next a sudden muscle weakness can leave you vulnerable. Being at home should feel safe, but the unpredictable nature of MG means you need extra layers of protection. That’s where a medical alert system steps in - a simple device that can summon help the moment you need it, even when you can’t pick up the phone.
What Is Myasthenia Gravis?
Myasthenia Gravis is a chronic autoimmune disorder that weakens the skeletal muscles, especially those that control eye movement, swallowing, and breathing. The immune system attacks acetylcholine receptors at the neuromuscular junction, causing rapid fatigue after even brief activity. Common symptoms include drooping eyelids, double vision, difficulty chewing, and in severe cases, a respiratory crisis that requires immediate medical attention.
Because the disease can swing from mild to life‑threatening without warning, staying prepared at home isn’t optional - it’s essential.
Why Home Safety Is Critical for MG Patients
- Fatigue can strike suddenly. Simple tasks like reaching for a glass can exhaust the muscles needed to stand or speak.
- Respiratory weakness. A respiratory crisis is a medical emergency where the diaphragm and intercostal muscles fail, leading to low oxygen levels.
- Fall risk. Weakness in the legs or sudden muscle collapse makes falls a real danger, especially on stairs or slippery floors.
- Medication side effects. Drugs like pyridostigmine and immunosuppressants can cause dizziness or low blood pressure, increasing the need for immediate help.
These factors combine to make a reliable way to call for assistance a non‑negotiable part of daily life.
What Is a Medical Alert System?
Medical alert system is a wearable or stationary device that connects you to a 24/7 monitoring center with a single button press. Modern versions go beyond a simple pendant - they incorporate fall detection, two‑way voice communication, GPS location tracking, and even smart‑home integration.
When you press the button, the system sends an emergency signal that includes your location and, if needed, a brief health summary. Trained operators can then contact family, caregivers, or local emergency services.
Choosing the Right System for Myasthenia Gravis
Not all alert devices are created equal. Here’s a quick checklist to keep in mind:
- Fall detection. Automatic alerts when the device senses a sudden impact or lack of movement.
- Two‑way voice. Ability to speak with the dispatcher without needing a separate phone.
- Battery life. Long‑lasting batteries (at least 48hours) are crucial if a power outage occurs.
- Water resistance. You’ll want a device you can wear while bathing or washing hands.
- Smart‑home compatibility. Integration with lights, locks, or voice assistants can help you stay independent.
- Cost and contract terms. Look for transparent monthly fees and optional no‑contract plans.
For MG patients, fall detection and two‑way voice are especially valuable because a sudden weakness can leave you unable to speak or move.

Top Three Medical Alert Systems for MG Patients
| System | Device Type | Fall Detection | Two‑Way Voice | Battery Life | Monthly Cost |
|---|---|---|---|---|---|
| LifeAlert Classic | Pendant + Base Station | No | Yes (via base) | 20 days (pendant) | $39.95 |
| Bay Alarm Medical | Bracelet + Mobile App | Yes (accelerometer) | Yes (direct) | 3 days (bracelet) | $29.95 |
| Apple Watch + Emergency SOS | Smartwatch | Yes (built‑in) | Yes (cellular) | 18 hours (active use) | $0 (requires iPhone & data plan) |
All three meet the core needs of MG patients, but each has trade‑offs. LifeAlert offers the longest battery life but lacks automatic fall detection. Bay Alarm balances fall detection with an affordable price, though you’ll need to charge the bracelet frequently. The Apple Watch provides the most advanced tech - GPS, fall detection, and cellular calls - but you must stay on a data plan and keep the watch charged.
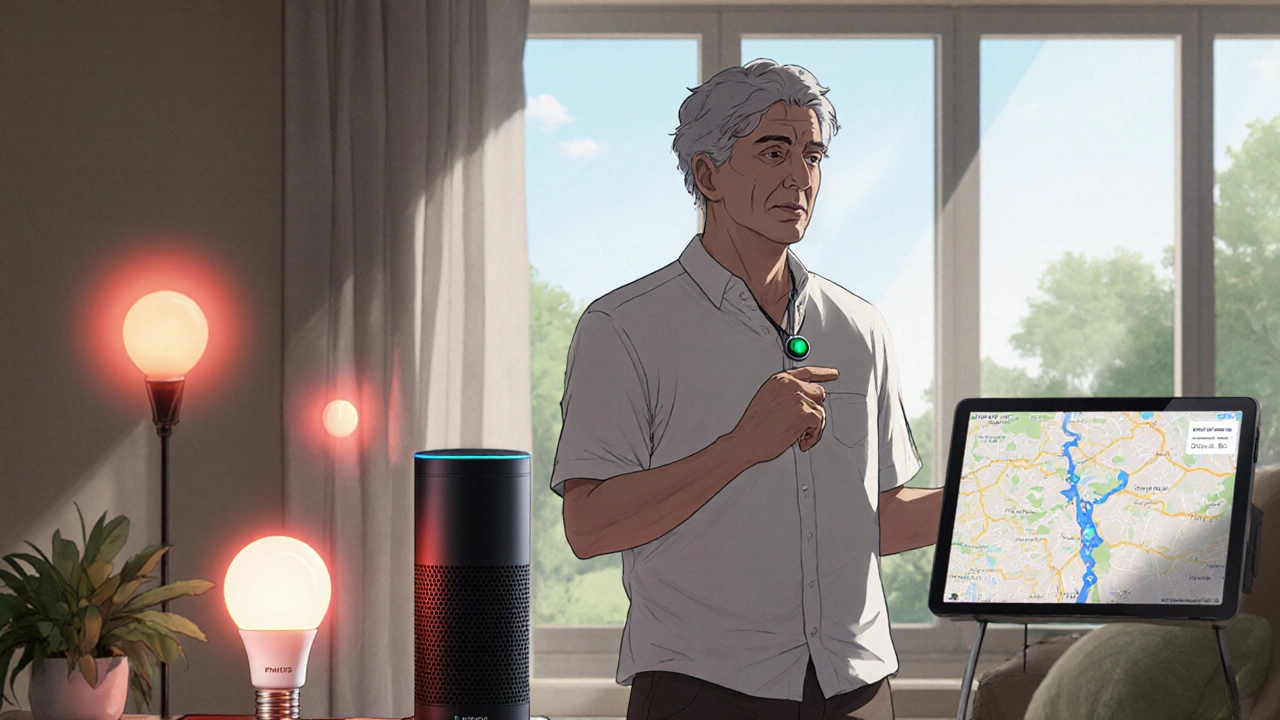
Integrating Alert Systems with Other Home Tech
Modern homes can become a safety network when you link your alert device to smart assistants (Alexa, Google Assistant) or home‑monitoring cameras. Here are a few practical combos:
- Smart lights. Connect the alert base station to Philips Hue so a red light flashes the moment an emergency is triggered - a visual cue for hearing‑impaired family members.
- Voice assistants. Program Alexa to call your caregiver when you say, “Help me now,” if you can still speak but can’t reach the button.
- Door sensors. Pair a door‑open sensor with the alert system so you get a reminder if you try to leave the house while experiencing muscle weakness.
When you set up these integrations, test them weekly. A simple “what if” drill can reveal missed connections before a real emergency.
Practical Steps to Set Up Your System
- Assess your risk profile. Talk to your neurologist about typical weakness patterns - does fatigue hit you in the evenings? Are you prone to nighttime breathing issues?
- Choose a device. Use the checklist above to match features with your daily routine.
- Register health information. Most monitoring centers let you enter a brief health summary - include MG diagnosis, current meds (pyridostigmine, immunosuppressants), and known allergies.
- Teach caregivers. Show family members how to use the base station, how to locate you via GPS, and how to reset the device after an alert.
- Test the system. Press the button once a week. Verify that you hear a clear voice prompt and that the monitoring center logs the call.
- Plan for power outages. Keep a spare battery pack or a backup mobile hotspot so the device stays online.
Following these steps gives you a reliable safety net without feeling like you’re living in a bunker.
Common Pitfalls & How to Avoid Them
- Ignoring battery alerts. Many devices beep when the battery is low, but you might miss the sound during a fatigue episode. Set a calendar reminder to check battery status daily.
- Not updating the health summary. If your medication changes (e.g., a new immunosuppressant dose), update the monitoring center so responders have the latest info.
- Relying on a single device. Have both a wearable pendant and a stationary base station. If you drop the pendant, the base can still call for help.
- Overlooking fall detection sensitivity. Some systems let you adjust the sensitivity. Too low and they miss falls; too high and you get false alarms. Test and fine‑tune.
When to Call a Professional
If you notice any of the following, contact your neurologist or an emergency service immediately:
- Increasing difficulty swallowing or speaking.
- Shortness of breath, especially when lying flat.
- Sudden loss of limb strength that doesn’t improve with rest.
- Repeated false alarms - could indicate device malfunction.
Prompt medical attention can prevent a full‑blown respiratory crisis, which in MG patients sometimes requires temporary ventilation.
Frequently Asked Questions
Will a medical alert system replace my regular doctor visits?
No. The system is an emergency backup that connects you to help fast. It doesn’t provide routine check‑ups, medication adjustments, or diagnostic testing.
Do I need a landline for the alert system to work?
Most modern systems use cellular or Wi‑Fi, so a landline isn’t required. If you choose a cellular plan, make sure you have good coverage in your home and backyard.
Can my caregiver receive alerts on their own phone?
Yes. Many providers let you add secondary contacts who receive SMS or app notifications the moment you press the button.
Is fall detection reliable for sudden muscle weakness?
Fall detection uses accelerometers to sense rapid movement changes. It works well for most trips and collapses, but you should still wear the device during high‑risk activities for manual alerts.
What should I do if the device triggers a false alarm?
Tell the monitoring center it was a false alarm; they’ll log it and can adjust sensitivity if needed. Test the device afterward to confirm it still works.












Nickolas Mark Ewald
October 17, 2025 AT 17:33 PMA medical alert system can be a real lifesaver for anyone dealing with unpredictable weakness. Make sure the battery is always charged and keep a spare at hand.
Tom Green
October 26, 2025 AT 18:33 PMChoosing the right system is a personal decision, but consider the checklist: fall detection, two‑way voice, battery life, water resistance, and cost. Share your experience with the community so we all can learn.
Emily Rankin
November 5, 2025 AT 00:46 AMLiving with Myasthenia Gravis is like walking on a tightrope in a storm, where every muscle twitch can decide the next step. Yet, the very existence of a simple button on your wrist can turn that peril into a promise of hope. Imagine the quiet moments when a sudden fatigue sweeps over you, the world dimming, and you press that button, knowing help is already rushing. The whisper of a monitoring center answering your call becomes a lifeline stitched into the fabric of daily life. Such devices remind us that vulnerability does not equate to helplessness, but rather invites community to step in. When the alert rings, caregivers feel the surge of responsibility morph into relief, as they know they are not alone. Technology, in this case, functions as a bridge between the silent struggle inside the body and the external world willing to listen. Every beep, every vibration, carries the echo of countless patients who have learned to trust machines as allies. The fall detection algorithms, though not perfect, act as an extra set of eyes when our own muscles betray us. Even if the device misfires once, the habit of testing it weekly hones our preparedness. Integration with smart lights or voice assistants adds a layer of redundancy that can be the difference between a swift rescue and a missed cue. Think of the moment when a red hue flashes in the hallway, signaling an emergency to a deafened family member. Or the calm voice that guides you through the process, assuring you that help is on its way. These moments reinforce the philosophy that safety is a collective construct, built from technology, routine, and compassion. In the end, the medical alert system does not cure Myasthenia Gravis, but it empowers us to live with dignity, confidence, and a safety net that catches us when we stumble.
Rebecca Mitchell
November 14, 2025 AT 07:00 AMI keep my own alert on my wrist just in case
Roberta Makaravage
November 23, 2025 AT 13:13 PMYou think you know everything about safety, but your advice often forgets the moral responsibility we all share 🌟🔔. Remember, a device is only as good as the compassion behind it 😊.
Lauren Sproule
December 2, 2025 AT 19:26 PMi love how many ppl forget to test their alert monthly reminder its real important dont skip it
CHIRAG AGARWAL
December 12, 2025 AT 01:40 AMI could just say the whole thing is overhyped but hey i guess some folks need it
Patricia Echegaray
December 19, 2025 AT 16:33 PMDon't be fooled by the glossy ads selling these gadgets; they're part of a larger scheme to keep us dependent on corporate surveillance, disguised as safety, while the real danger lurks in unchecked data collection.