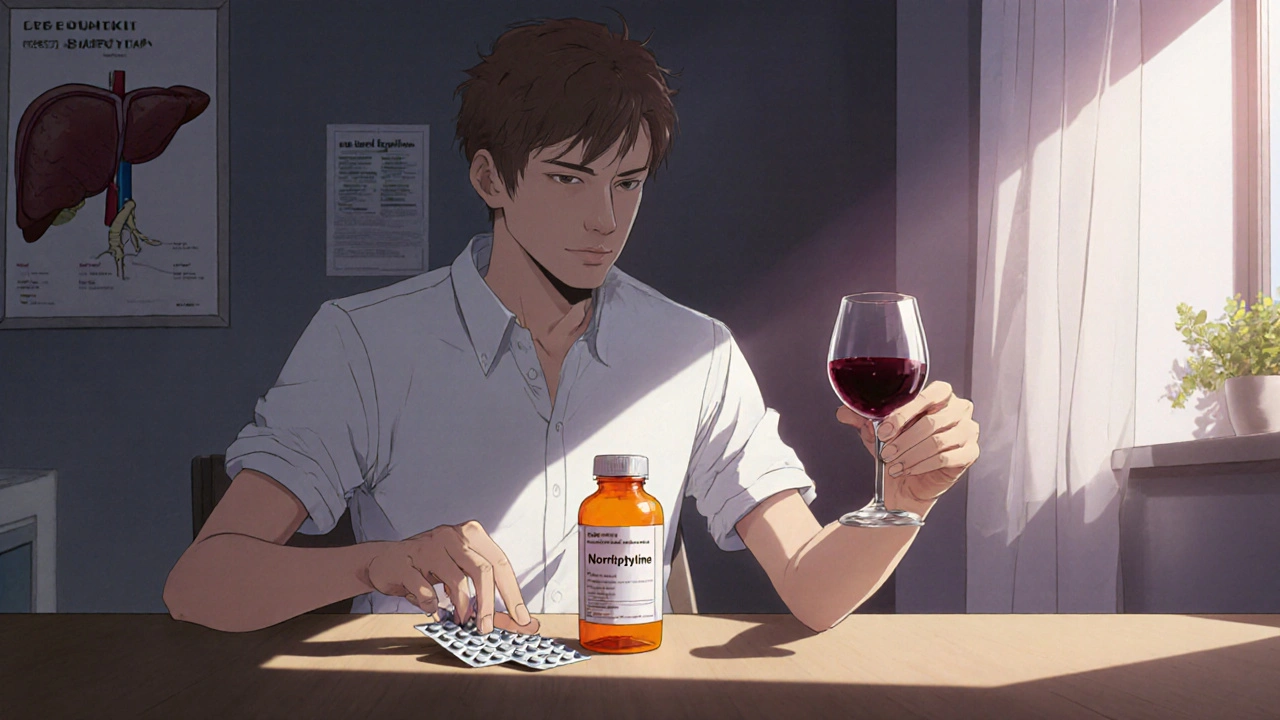
Understanding the risks of nortriptyline and alcohol is crucial for anyone taking this medication. Mixing the two can lead to a cascade of side effects, some of which may be life‑threatening. This guide walks you through how nortriptyline works, why alcohol complicates matters, and what you can do to stay safe.
What Is Nortriptyline?
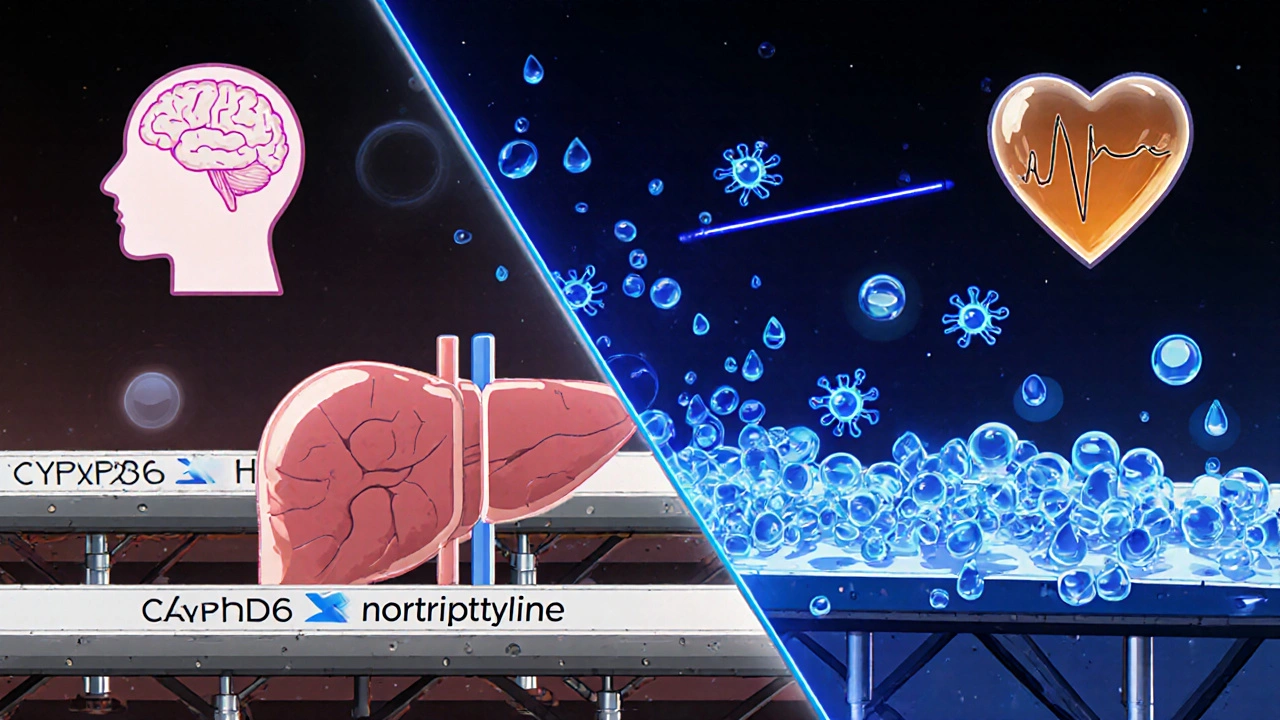
Nortriptyline is a tricyclic antidepressant (TCA) that increases levels of neurotransmitters such as norepinephrine and serotonin in the brain. It is commonly prescribed for major depressive disorder, chronic neuropathic pain, and sometimes for migraine prevention. The drug is absorbed well orally, reaches peak plasma concentrations in 2‑4 hours, and is metabolized primarily by the liver enzyme CYP2D6. Because its half‑life ranges from 18 to 44 hours, the medication stays in the system for days after the last dose.
How Alcohol Affects the Body
Alcohol is a central nervous system depressant that interferes with the balance of neurotransmitters, especially gamma‑aminobutyric acid (GABA) and glutamate. Even moderate drinking can lower blood pressure, impair motor coordination, and reduce the liver’s ability to metabolize other substances. When alcohol is consumed regularly, the liver's enzymatic pathways, including CYP2D6, become saturated or inhibited, slowing down the clearance of many medications.
Why Mixing Nortriptyline and Alcohol Is Problematic
The interaction stems from three overlapping mechanisms:
- Pharmacokinetic interference: Alcohol competes for the same liver enzymes that break down nortriptyline, leading to higher blood concentrations of the drug.
- Pharmacodynamic synergy: Both substances depress the central nervous system, amplifying sedation, dizziness, and impaired judgment.
- Cardiovascular strain: Nortriptyline can cause orthostatic hypotension; alcohol further lowers blood pressure, increasing the risk of fainting or falls.
Because nortriptyline also affects serotonin levels, combining it with alcohol’s impact on serotonin pathways can trigger serotonin syndrome in rare but serious cases.
Common Side Effects When Combined
The following symptoms appear more frequently or more intensely when alcohol is added to a nortriptyline regimen:
| Effect | Nortriptyline Alone | With Alcohol |
|---|---|---|
| Drowsiness | Moderate | Severe, may impair driving |
| Dizziness / Light‑headedness | Occasional | Often pronounced, risk of falls |
| Blood pressure drop | Possible orthostatic hypotension | Significant hypotension, fainting |
| Heart rhythm irregularities | Rare | Increased QT prolongation risk |
| Gastrointestinal upset | Mild nausea | Worsened nausea, vomiting |
| Serotonin syndrome signs | Very rare | Higher chance if binge drinking |
Who Is Most at Risk?
Not everyone experiences the same level of danger. Certain groups are more vulnerable:
- Older adults: Age‑related declines in liver function and balance make side effects more severe.
- People with liver disease: Conditions like hepatitis or fatty liver already compromise CYP2D6 activity.
- Individuals on multiple CNS depressants: Combining benzodiazepines, antihistamines, or opioids with nortriptyline and alcohol multiplies sedation.
- Fast or poor metabolizers: Genetic variations in CYP2D6 can cause unexpectedly high drug levels.
Safer Alternatives and Harm‑Reduction Tips
If you’re prescribed nortriptyline and enjoy an occasional drink, consider these strategies:
- Limit intake: Stick to one standard drink (12 oz beer, 5 oz wine, or 1.5 oz spirit) and avoid binge patterns.
- Schedule wisely: Take your dose early in the day, giving the drug time to reach steady state before any evening alcohol.
- Stay hydrated: Water helps the liver process both substances more efficiently.
- Monitor blood pressure: Use a home cuff or have regular checks; report any dizziness to your clinician.
- Consider a different medication: SSRIs or SNRIs have fewer sedative interactions with alcohol for many patients.
- Genetic testing: A simple CYP2D6 test can reveal whether you’re a rapid or poor metabolizer, guiding dose adjustments.
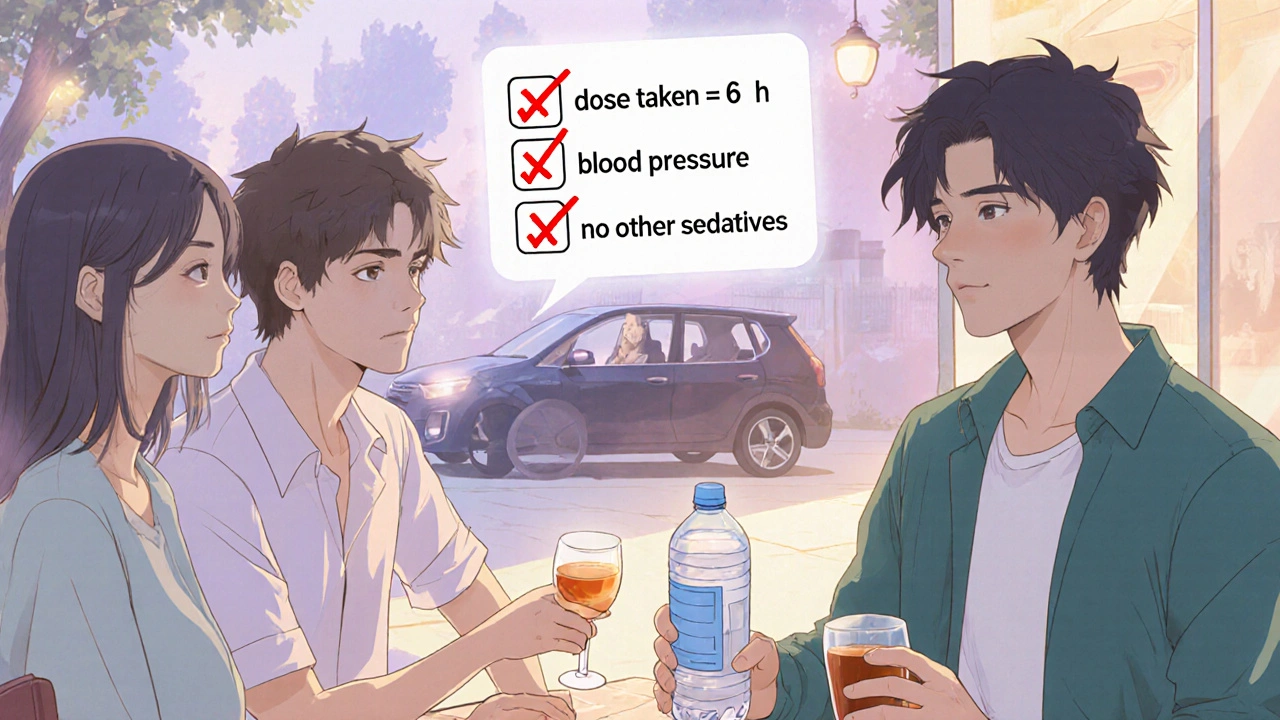
Quick Checklist Before You Drink
- Have you taken your dose within the past 6‑8 hours?
- Is your liver function normal (recent labs OK)?
- Do you feel any pre‑existing dizziness or low blood pressure?
- Are you mixing any other sedatives or antihistamines?
- Can you arrange a safe ride home?
If you answer “no” to any of these, it’s best to skip the drink.
When to Seek Medical Help
Immediate medical attention is warranted if you experience any of the following after mixing nortriptyline and alcohol:
- Severe confusion or hallucinations
- Rapid heart rate (>120 bpm) or irregular rhythm
- Chest pain or shortness of breath
- Severe vomiting that prevents you from keeping fluids down
- Unexplained sweating, shivering, or high fever (possible serotonin syndrome)
Call emergency services or go to the nearest emergency department. Mention both nortriptyline and alcohol so clinicians can assess for interaction‑related complications.
Frequently Asked Questions
Can I have a glass of wine while on nortriptyline?
A single glass of wine is less likely to cause serious problems, but you should still monitor for extra drowsiness or light‑headedness. If you notice any new symptoms, stop drinking and talk to your doctor.
Why does alcohol increase the risk of low blood pressure?
Alcohol dilates blood vessels, causing blood to pool in the lower extremities. Nortriptyline already can cause orthostatic hypotension. Together they amplify the drop, making you feel faint.
Is it safe to stop drinking completely while on nortriptyline?
Yes. Eliminating alcohol removes the interaction risk entirely. If you enjoy occasional social drinks, discuss a safe limit with your prescriber instead of quitting abruptly.
Can I switch to an SSRI to avoid this interaction?
Many clinicians do switch patients from TCAs like nortriptyline to SSRIs because SSRIs have fewer sedative effects. However, the switch must be done gradually under medical supervision to avoid withdrawal or relapse.
What should I do if I accidentally binge‑drink while on nortriptyline?
Stay hydrated, sit or lie down safely, and avoid driving. If you feel severe dizziness, rapid heartbeat, or confusion, seek emergency care right away.









Barbara Ventura
October 26, 2025 AT 17:10 PMWow, this guide really breaks down the nortriptyline‑alcohol combo in plain terms!!! It’s refreshing to see the science laid out with clear headings, and the checklist is super handy. Just remember: the liver can only handle so much, so moderation is key.
Barna Buxbaum
October 26, 2025 AT 19:06 PMGreat rundown! I appreciate the practical tips like timing your dose and staying hydrated – those are easy changes that can make a big difference. If you ever feel light‑headed, it’s a solid idea to check your blood pressure at home before reaching for a drink. Also, a quick reminder: mixing other CNS depressants can amplify sedation, so keep a medication list handy. Keep sharing these clear, evidence‑based posts!
Carolyn Cameron
October 26, 2025 AT 21:03 PMOne must acknowledge the erudite synthesis presented herein; the juxtaposition of pharmacokinetic and pharmacodynamic considerations is most commendable. Nevertheless, a more exhaustive exposition on CYP2D6 polymorphisms would elevate the discourse to an academic standard.
Leah Ackerson
October 26, 2025 AT 23:00 PMAh, the age‑old dilemma of pleasure versus prudence 🌟. One could argue that the fleeting euphoria of a glass of wine pales in comparison to the lingering specter of orthostatic collapse. Yet, perhaps the true peril lies not in the drink itself, but in the complacency it breeds. 🍷🤔
Gary Campbell
October 27, 2025 AT 00:56 AMEveryone’s told to "just avoid alcohol", but they don’t realize the pharma industry’s hidden agenda to keep us scared and dependent. The real story is that the FDA’s data on nortriptyline interactions are deliberately suppressed. Trust the community, not the corporations.
ahmed ali
October 27, 2025 AT 02:53 AMWhile many enthusiasts champion the simplistic view that a single drink is innocuous, the reality is vastly more intricate.
First, nortriptyline’s half‑life can extend beyond two days, meaning residual plasma levels persist long after the last dose.
Second, alcohol acts as a competitive inhibitor of CYP2D6, the very enzyme responsible for metabolizing nortriptyline, thereby prolonging its activity.
Third, the synergistic depressant effect on the central nervous system can precipitate profound sedation, far beyond what either substance induces alone.
Fourth, both agents influence serotonergic pathways, raising a non‑trivial risk of serotonin syndrome, especially in binge‑drinking scenarios.
Fifth, orthostatic hypotension, a hallmark adverse effect of nortriptyline, is exacerbated by alcohol‑induced vasodilation, leading to dizziness and potential falls.
Sixth, cardiovascular ramifications such as QT prolongation become more likely when plasma concentrations spike due to hepatic competition.
Seventh, the gastrointestinal tract suffers; nausea and vomiting are magnified, impairing nutrient absorption and hydration.
Eighth, genetic polymorphisms in CYP2D6 mean that poor metabolizers may experience drug accumulation even with modest alcohol intake.
Ninth, age‑related declines in liver function further compound these interactions in older adults.
Tenth, co‑administration with other CNS depressants-benzodiazepines, antihistamines, opioids-creates a perfect storm of sedation.
Eleventh, empirical studies have shown that even low‑dose alcohol can double the sedative load when combined with TCAs.
Twelfth, the subjective feeling of “being fine” is deceptive; impaired motor coordination can persist unnoticed.
Thirteenth, patients often underestimate the delayed onset of adverse effects, attributing them to other causes.
Fourteenth, clinicians may not routinely monitor blood pressure after a patient reports occasional drinking, missing early warning signs.
Fifteenth, the safest approach remains to either abstain or strictly limit intake, adhering to the checklist provided.
In sum, the interplay between nortriptyline and alcohol is a multifaceted pharmacological challenge that deserves rigorous attention rather than casual dismissal.
Deanna Williamson
October 27, 2025 AT 04:50 AMYour post is overly simplistic and ignores critical metabolic pathways.
Miracle Zona Ikhlas
October 27, 2025 AT 06:46 AMThanks for the balanced advice; staying hydrated and checking blood pressure are simple steps that can protect everyone.
Samantha Taylor
October 27, 2025 AT 08:43 AMOh, brilliant-another reminder that we should all act like perfect little lab rats. Your thoroughness is truly awe‑inspiring, especially for those of us who love reading about every possible worst‑case scenario. I’m sure this will put an end to all spontaneous drinking adventures forever.
Joe Langner
October 27, 2025 AT 10:40 AMLet’s keep the convo positive-if you can manage a single drink responsibly, you’re already on the right path! Remember, small steps lead to big gains, and a mindful approach to medicaion and booze can boost your overall wellness.