Every year in the U.S., medication errors contribute to tens of thousands of preventable deaths. The numbers aren’t hypothetical-they’re tracked, documented, and terrifying. According to the Agency for Healthcare Research and Quality, one in every 131 outpatient deaths and one in every 8,548 inpatient deaths are tied directly to mistakes in how drugs are ordered, dispensed, or given. These aren’t rare glitches. They’re systemic failures that happen in hospitals, clinics, and even community pharmacies. And if you work in pharmacy or patient care, you’ve probably seen them up close.
What Are the National Patient Safety Goals?
The National Patient Safety Goals (NPSGs) aren’t suggestions. They’re mandatory standards set by The Joint Commission, the same group that accredits nearly every U.S. hospital. First launched in 2003, these goals were created after a landmark 1999 report from the Institute of Medicine found that medical errors kill more people than car accidents or breast cancer. Since then, medication safety has been the #1 focus.
The 2025 NPSGs have three core medication-related requirements:
- NPSG.03.04.01: Label every medication, syringe, IV bag, and container-on and off the sterile field. The label must include the drug name, strength, concentration, and expiration date. Font size? Minimum 10-point. No exceptions.
- NPSG.03.05.01: Reduce harm from anticoagulants like warfarin and heparin. This means standardized protocols for INR monitoring, clear documentation of therapeutic ranges, and patient education. Compliance must hit 95% or higher, tracked quarterly.
- NPSG.03.06.01: Manage high-alert medications. These are drugs that can cause serious harm if given wrong-insulin, opioids, chemotherapy, injectable potassium. Facilities must have specific safeguards in place, including double-checks, restricted access, and automated dispensing cabinet controls.
These aren’t just paperwork. They’re enforced. Hospitals that fail audits risk losing accreditation-and with it, Medicare and Medicaid payments.
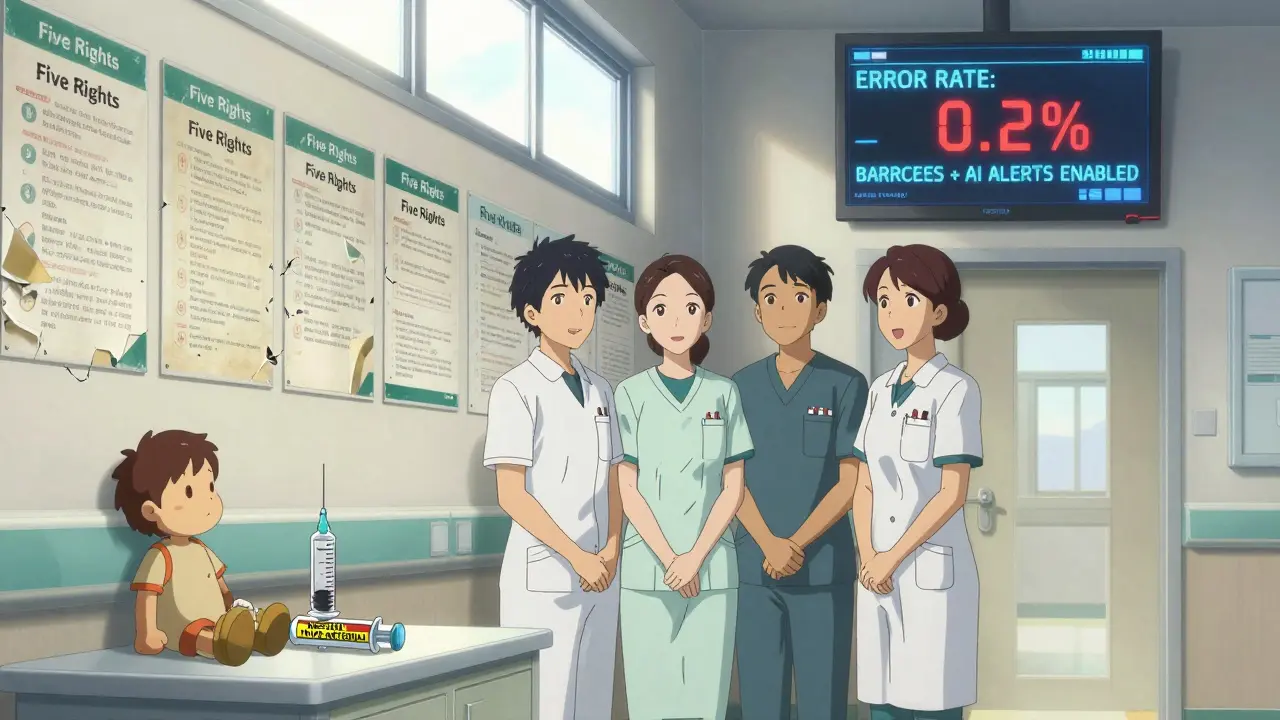
Why the Five Rights Don’t Cut It Anymore
You’ve heard the mantra: right patient, right drug, right dose, right route, right time. It’s taught in nursing school. It’s printed on wall posters. But here’s the hard truth: 83% of medication errors still happen even when nurses confirm all five rights.
Why? Because the Five Rights put the burden on people, not systems. Imagine a nurse rushing through a 12-hour shift, juggling eight patients, a broken IV pump, and a last-minute stat order. They check the wristband. They scan the barcode. They read the label. But the label was printed wrong. The barcode was mislabeled. The system didn’t catch it. Now what? Blame the nurse? That’s not safety-that’s punishment.
The Institute for Healthcare Improvement says it plainly: the Five Rights are a checklist, not a solution. Real safety comes from designing systems that make mistakes harder to make. That means barcode scanning at the bedside, automated dispensing cabinets with audit trails, and electronic alerts that block dangerous interactions before they happen.
High-Alert Medications: Where the Real Risks Live
Not all drugs are created equal. Some are so dangerous that even a small error can kill. The Institute for Safe Medication Practices (ISMP) tracks 19 high-risk scenarios. Here are three that still cause avoidable deaths:
- Promethazine injections: Between 2006 and 2018, 37 patients lost limbs because this anti-nausea drug was accidentally given into an artery instead of a vein. It destroys tissue. Now, hospitals must use dedicated syringes, label them clearly, and never mix them with other meds.
- Opioid overdoses: Before giving opioids, pharmacists and nurses must verify the patient’s current opioid use, tolerance level, and recent respiratory status. One missed detail-and a patient who’s been on methadone for years can stop breathing after a single dose.
- Insulin errors: A 10-unit dose given instead of 1 unit? That’s a medical emergency. Hospitals now require insulin to be stored separately, labeled with bold text, and double-checked by two staff members before administration.
These aren’t theoretical risks. They’re documented, counted, and preventable. The tools to stop them exist. What’s missing is consistent execution.
Automated Dispensing Cabinets: A Double-Edged Sword
Automated dispensing cabinets (ADCs) were supposed to fix medication errors. They store drugs securely, track who takes what, and prevent unauthorized access. But they’ve created a new problem: overrides.
An override happens when a clinician bypasses the system to grab a drug immediately-usually during emergencies. Sounds reasonable. Except: 34% of pharmacists report override rates exceeding 5%, the safety threshold. One hospital in Ohio had an override rate of 18%. In the same period, their wrong-drug error rate jumped 40%.
Why? Because overrides are often used for convenience, not crisis. A nurse grabs morphine from the ADC without scanning because “the patient’s in pain and I’m too busy.” The system doesn’t log who took it. The label isn’t checked. The dose isn’t verified. And now, you’ve got a hidden error.
The fix? Proactive risk assessment. Hospitals need to analyze why overrides happen. Is it staffing? Workflow? Training? Then build solutions-like keeping emergency meds in a separate, easily accessible cabinet with its own safety protocols.
Barcodes, EHRs, and AI: The Tech That’s Actually Working
Technology isn’t magic. But when it’s used right, it saves lives.
Barcode-assisted medication administration (BCMA) has cut wrong-drug errors by 86% in hospitals that use it consistently. But here’s the catch: it only works if every step is followed. If a nurse scans the wrong barcode, skips the patient ID, or disables the alert because “it’s too slow,” the system fails.
Electronic health records (EHRs) integrated with clinical decision support are another game-changer. A 2025 study at Mayo Clinic showed that AI-powered alerts reduced potential adverse drug events by 47%. The system flagged a patient on multiple blood thinners who was about to get a new antibiotic that would spike their INR. The pharmacist caught it. The patient was safe.
But tech alone won’t fix culture. If pharmacists are overworked, nurses are burnt out, and administrators don’t prioritize safety, even the best system becomes a glorified checklist.
What’s Working: Real-World Success Stories
Not every hospital is stuck in the same cycle. Some are getting it right.
Children’s Hospital of Philadelphia implemented a pediatric-specific safety model. They required double-checks for all high-alert meds in the NICU and ICU. They standardized weight-based dosing with pre-calculated charts. Result? A 91% drop in dosing errors.
A hospital in Minnesota installed bedside specimen labeling with two-identifier verification. Before, 1 in 10 blood samples were mislabeled. After? Zero errors in 18 months.
These aren’t outliers. They’re proof that when you combine technology, clear protocols, and leadership commitment, errors drop-not because people are better, but because the system is smarter.
The Hidden Cost of Poor Safety
Medication errors don’t just hurt patients. They hurt hospitals financially.
The Centers for Medicare & Medicaid Services (CMS) now withhold 2% of hospital reimbursements if they have high rates of preventable errors. The global patient safety software market is projected to hit $4 billion by 2028-not because it’s trendy, but because hospitals have no choice. Non-compliance = lost revenue.
And then there’s the human cost. A mother who loses her child because a syringe wasn’t labeled. A veteran who overdoses because his opioid history wasn’t checked. A nurse who quits because she’s tired of being blamed for a system that’s broken.
These aren’t just statistics. They’re real lives.
What Needs to Change
Here’s the bottom line: patient safety isn’t about doing more. It’s about doing things differently.
- Stop blaming individuals. Errors are system failures, not moral failures.
- Invest in automation. Barcode scanning, EHR alerts, and smart dispensing cabinets aren’t luxuries-they’re necessities.
- Train like it matters. 38% of hospitals give less than 4 hours of safety training per year. That’s not enough. Require 12 hours. Quarterly.
- Make safety a leadership priority. Hospitals with executive sponsorship have 89% sustainability rates. Those without? 42%.
- Engage patients. Facilities that ask patients to confirm their meds report 42% fewer errors. A simple question: “Is this the right medicine for you?” can save a life.
The tools exist. The data is clear. The goals are non-negotiable. The question isn’t whether we can do better. It’s whether we’re willing to.









