SJS/TEN Early Warning Symptom Checker
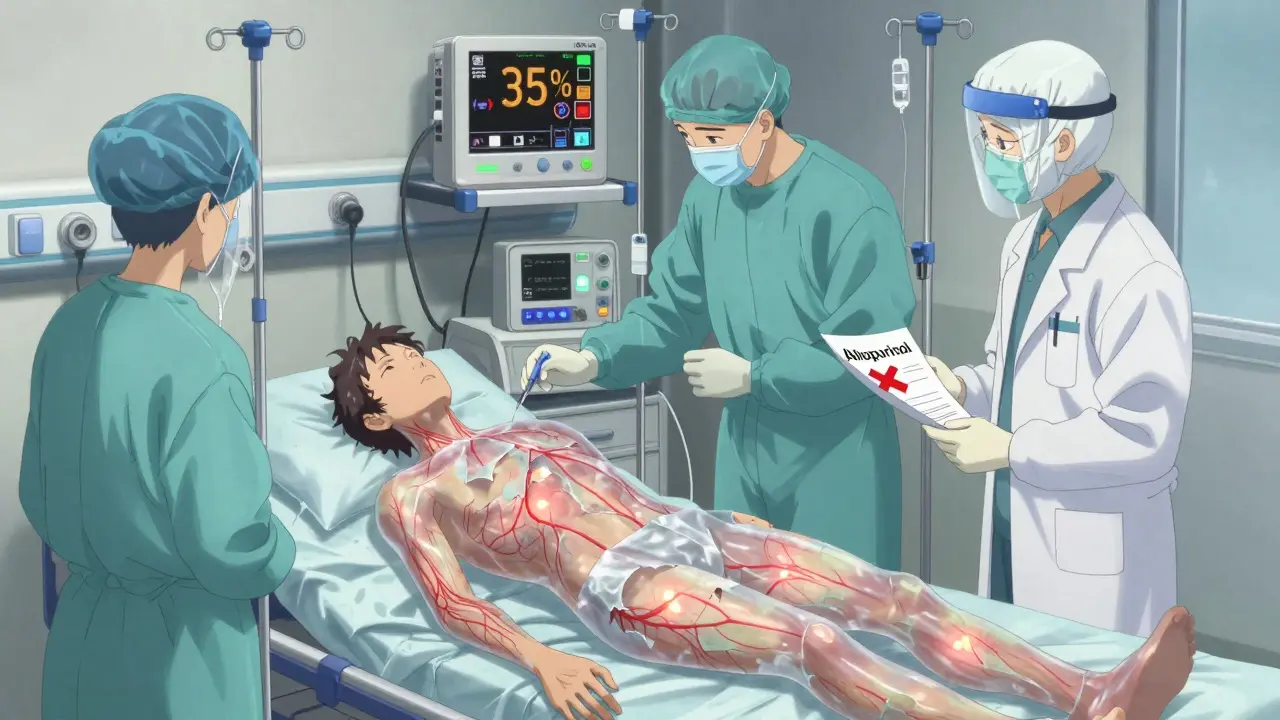
Early Warning Symptoms
Select all symptoms you or someone you know is experiencing. This tool is designed to help recognize potential SJS/TEN symptoms which require immediate medical attention.
Symptom Analysis
URGENT WARNING
SJS/TEN is a medical emergency requiring immediate hospital care. Do not delay seeking medical attention if you have these symptoms.
When a medication you’ve been taking suddenly turns your skin into a burning, blistering mess, it’s not just a rash - it’s a medical emergency. Stevens-Johnson Syndrome (SJS) and Toxic Epidermal Necrolysis (TEN) are rare but deadly reactions triggered by certain drugs. They don’t wait for permission. They strike fast, and if you don’t recognize them early, the consequences can be permanent - or fatal.
What Exactly Are SJS and TEN?
Stevens-Johnson Syndrome and Toxic Epidermal Necrolysis are two ends of the same dangerous spectrum. Both are severe skin reactions caused by medications, and they share the same root problem: your immune system attacks your own skin and mucous membranes.
SJS typically affects less than 10% of your body surface area. TEN is the more extreme form, where more than 30% of your skin dies and peels off - like a severe burn, but from the inside out. Between those two? A gray zone called SJS/TEN overlap, where 10% to 30% of your skin is involved. The difference isn’t just numbers - it’s survival.
Death rates jump sharply as the condition worsens. For SJS, the risk of dying is about 5%. For TEN, it’s over 30%. And those numbers don’t include the long-term damage that can follow even if you survive.
How Does It Start?
It doesn’t begin with a few itchy spots. It starts like the flu. Fever, sore throat, burning eyes, fatigue - you might think you’re coming down with something common. Then, within one to three days, your skin changes.
A red or purple rash appears, often starting on your face and chest. It spreads fast. Blisters form. Your skin begins to slough off in sheets. Inside your mouth, nose, eyes, and genitals, the lining breaks down. You can’t eat. You can’t blink. You can’t urinate without pain.
This isn’t an allergic reaction you can treat with antihistamines. It’s full-thickness epidermal necrosis - your outer skin layer dies and detaches. A skin biopsy is the only way to confirm it, but by then, you’re already in the hospital.
Which Medications Cause It?
Not every drug causes this. But some carry a known, documented risk. The most common culprits are:
- Allopurinol - used for gout
- Carbamazepine, lamotrigine, phenytoin, phenobarbital - antiseizure meds
- Nevirapine - an HIV drug
- Meloxicam and piroxicam - NSAIDs, often sold as joint pain relievers
- Sulfamethoxazole - part of the antibiotic Bactrim
Here’s the scary part: if you’ve had SJS from one of these, you can’t take any drug in the same class again. Cross-reactivity is real. Survivors of lamotrigine-induced SJS can’t safely take carbamazepine or phenytoin. Someone who reacted to sulfamethoxazole shouldn’t take any sulfa drug, ever.
And timing matters. Reactions can happen within days of starting a new drug - or up to two weeks after you stop. Some cases flare up if you restart a medication too quickly after a break. For lamotrigine, restarting at the old dose after a few days off is a known trigger.
Who’s at Higher Risk?
It’s not random. Certain people are more vulnerable:
- Those with HIV or weakened immune systems from chemotherapy
- People who’ve had a previous rash from epilepsy meds
- Those allergic to trimethoprim
- Anyone taking sodium valproate with lamotrigine - this combo increases risk
- People with a family history of SJS/TEN - suggesting a genetic link
Children are more likely to get SJS than adults, but the condition hits anyone on high-risk drugs. And once you’ve had it? Your risk of recurrence if you’re exposed again is extremely high. That’s why avoiding even similar drugs is non-negotiable.
What Happens After You Survive?
Surviving SJS or TEN doesn’t mean you’re back to normal. Far from it.
Up to half of survivors develop serious eye problems: dry eyes, scarring, abnormal eyelash growth, corneal damage, and even blindness. Many need lifelong care from ophthalmologists.
Your skin doesn’t heal cleanly. Scarring, dark or light patches, and permanent hair loss are common. Nails may fall off and take months to grow back - if they do. Mouth sores can lead to gum disease and difficulty eating. Swallowing can become painful if your esophagus scars shut. Women may face vaginal stenosis; men can develop phimosis.
Internal damage is also possible. Sepsis, lung clots, heart attacks, and kidney failure can follow. Recovery isn’t just about skin. It’s about rebuilding your whole body.

What Do You Do If You Suspect It?
If you’re on a high-risk drug and you develop a rash with blisters, fever, or mouth sores - go to the emergency room immediately. Don’t wait. Don’t call your doctor tomorrow. Don’t try an OTC cream.
Time is everything. The sooner the drug is stopped and you’re in a specialized unit (often a burn or ICU unit), the better your chance of survival. Treatment is supportive: fluids, pain control, wound care, infection prevention. There’s no magic drug that cures it.
Some hospitals use IVIG or steroids, but evidence is mixed. The most proven step? Stopping the drug - and fast.
Can You Prevent It?
You can’t predict who will react. But you can reduce your risk.
- If you’re starting lamotrigine, carbamazepine, or allopurinol - follow the slow titration schedule exactly. Rushing the dose increase is a known trigger.
- Don’t start new medications or supplements during the first 8 weeks of treatment with high-risk drugs.
- Know your family history. If a close relative had SJS, tell your doctor before starting any new meds.
- Keep a list of all drugs you’ve reacted to - and share it with every provider you see.
- If you’ve had SJS before, wear a medical alert bracelet.
Most rashes from these drugs are harmless. But if yours spreads fast, hurts, or involves your mouth or eyes - treat it like a fire. Call 911. Go to the ER. Your life depends on it.
Why This Matters More Than You Think
SJS and TEN are rare - about five cases per million users per week. But rarity doesn’t mean irrelevance. These reactions kill more people than many rare cancers. And because they’re triggered by common drugs, they’re not going away.
Doctors know the risks. But patients? Too often, they’re not warned. A simple rash gets labeled as "allergic" and ignored. A fever gets chalked up to a cold. By the time someone realizes it’s SJS, it’s too late.
The truth? You don’t need to avoid all meds. You need to know the signs. You need to act fast. And you need to tell every doctor you’ve ever had a reaction - even if it was years ago.
Because when your skin starts to die, there’s no second chance. Only speed.










Cassie Widders
January 13, 2026 AT 14:21 PMI had a rash from allopurinol last year. Thought it was just heat. Turned out it was SJS. I spent three weeks in ICU. Don’t ignore rashes anymore.
Konika Choudhury
January 15, 2026 AT 13:40 PMWhy do western doctors always blame meds first? In India we know its pollution and bad diet that kills people not pills
Jose Mecanico
January 16, 2026 AT 01:37 AMThis is one of the most important posts I’ve read all year. I’m a nurse and I’ve seen TEN up close. The skin peeling off like wet paper... it’s not something you forget. If you’re on lamotrigine or allopurinol, listen to this.
steve ker
January 17, 2026 AT 20:24 PMSo drugs bad huh. Wow groundbreaking. Next you’ll tell me breathing air can be dangerous
Alice Elanora Shepherd
January 19, 2026 AT 09:40 AMImportant note: If you’ve had SJS/TEN from any drug, please, please, please tell every single provider you see-even the dentist. I’ve seen patients get re-exposed because they forgot to mention it. Keep a list. Write it on your phone. Tell your mom. This isn’t drama-it’s survival.
Also: If you’re on lamotrigine, the titration schedule isn’t a suggestion. It’s a lifeline. Skip steps? You’re gambling with your skin.
And if you’re a caregiver? Watch for fever + rash + mouth sores. Don’t wait for blisters. By then, it’s too late. Call 911.
I’ve worked in dermatology for 18 years. This is the one thing I beg every patient to remember.
Christina Widodo
January 19, 2026 AT 16:39 PMWait so if I had a mild rash from Bactrim five years ago, does that mean I can never take any sulfa drug again? Even for a UTI? What if it’s life-threatening? Like if I get pneumonia?
Prachi Chauhan
January 21, 2026 AT 05:42 AMIt’s funny how we fear drugs more than the systems that give them to us. We blame the pill, not the doctor who prescribed it without genetic screening. We panic about skin shedding but ignore how healthcare ignores patient history. SJS isn’t just a reaction-it’s a symptom of broken medicine.
Why don’t we screen for HLA-B*15:02 before giving carbamazepine? Why isn’t this mandatory? Why is survival left to luck and timing?
We treat the body like a machine. But when the immune system turns on itself, it’s not a glitch-it’s a cry. And we’re not listening.
Katherine Carlock
January 21, 2026 AT 12:03 PMThank you for posting this. My cousin survived TEN after a reaction to meloxicam. She lost her eyelashes, her nails, and now she has chronic dry eyes. She can’t wear contacts anymore. She’s 29. It’s heartbreaking. Please, if you’re on any of these meds-know the signs. Don’t wait.
Sona Chandra
January 21, 2026 AT 16:13 PMMY BEST FRIEND DIED FROM THIS AND NO ONE TOLD ME IT COULD HAPPEN!!! I WAS JUST TOLD IT WAS "ALLERGY" AND TO TAKE BENADRYL!!! NOW SHE’S GONE AND I’M LEFT WITH NOTHING BUT GUILT AND ANGER!!!
Jennifer Phelps
January 21, 2026 AT 18:08 PMSo if I had a rash from phenytoin 10 years ago and now I need something for seizures can I ever take anything again or am I just screwed
beth cordell
January 22, 2026 AT 10:31 AMThank you for this 💔 I’m so glad someone finally said this out loud. My sister’s skin peeled off like a sunburn but worse… she cried because she couldn’t feel her own hands. I’ll never forget that. 🫂
Craig Wright
January 24, 2026 AT 08:39 AMIt is imperative that all pharmaceutical manufacturers be held accountable for the failure to adequately warn patients regarding the potential for severe cutaneous adverse reactions. The current regulatory framework is insufficient and demands immediate reform.
Lelia Battle
January 24, 2026 AT 16:10 PMThere’s something deeply human about how we treat skin as separate from the self. But when your skin dies, it’s not just a surface-it’s your boundary with the world. You can’t touch, you can’t be touched. It’s not just physical. It’s existential.
I’ve seen patients who survived, but never stopped feeling like they were made of glass.
Rinky Tandon
January 26, 2026 AT 03:29 AMWhy are we still using these dangerous drugs? It's 2025. We have alternatives. Why are we still letting people die from outdated medications? Someone needs to sue the pharmaceutical industry and make them pay.
Ben Kono
January 26, 2026 AT 05:33 AMMy dad died from this after taking piroxicam. They said it was "rare" so they didn’t warn him. Now I’m the one who has to tell every new doctor he sees. Don’t let this happen to your family.