Chronic Ulcer
When dealing with chronic ulcer, a long‑lasting sore that fails to heal within the typical three‑week window. Also known as persistent ulcer, it often signals underlying health issues that need attention. Closely related conditions include ulcerative colitis, an inflammatory bowel disease that causes continuous ulcers in the colon lining and peptic ulcer, a sore in the stomach or duodenal lining caused by acid and H. pylori infection. Even skin ulcer, a break in the skin often seen on legs or feet shares management principles with chronic ulcer, like proper wound care and infection control.
Why do these sores stick around? A key semantic link is that chronic ulcer encompasses persistent tissue damage (Subject‑Predicate‑Object). It often stems from poor circulation, diabetes, or prolonged pressure on a bony prominence. When blood flow falters, cells can’t get the oxygen they need, so the wound stalls in the inflammatory phase. This relationship explains why “management of chronic ulcer requires proper wound care” – cleaning, debridement, and moisture‑balanced dressings become essential tools.
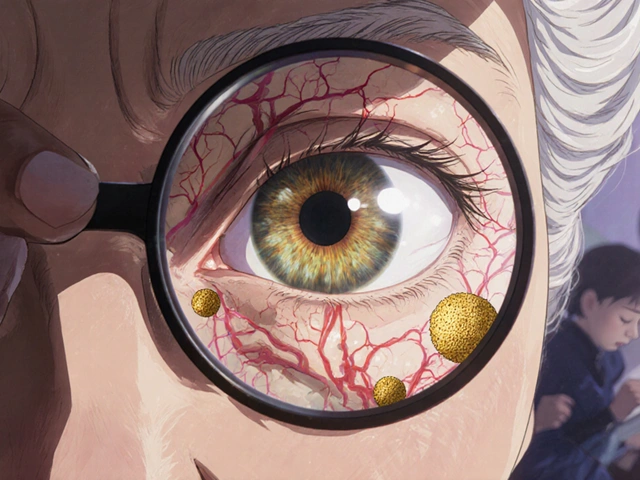
Risk factors act as another semantic bridge: “risk factors such as diabetes influence chronic ulcer development.” High blood sugar damages small vessels, making it harder for nutrients to reach the wound. Likewise, smoking narrows arteries, and obesity adds pressure to weight‑bearing areas. Recognizing these contributors lets you target prevention—quitting smoking, controlling glucose, and wearing pressure‑relieving footwear can tip the healing process back on track.
Diagnosis isn’t just a visual check. Health professionals often use the Ankle‑Brachial Index to gauge circulation, and may order a biopsy if infection is suspected. For ulcers inside the gut, endoscopy can reveal peptic lesions, while colonoscopy spots ulcerative colitis ulcers. Understanding that “diagnostic testing guides appropriate treatment” helps you see why a thorough work‑up matters before picking a therapy.
Treatment options vary, but they all share a common goal: restore healthy tissue. Topical antibiotics like mupirocin, mentioned in our article on mupirocin allergy, are frequently used to prevent bacterial overgrowth in skin ulcers. For gastrointestinal ulcers, proton‑pump inhibitors reduce acid, while antibiotics clear H. pylori. In chronic ulcer care, off‑loading devices—special shoes, cushions, or casts—reduce pressure, allowing blood to flow. Nutritional support, especially protein and vitamin C, fuels collagen formation, a crucial step in wound closure.
Practical Steps You Can Take Today
First, keep the wound clean. Gently rinse with saline, avoid harsh soaps, and change dressings according to your provider’s schedule. Second, protect the area from extra pressure; a simple cushion or custom‑made shoe insert can make a big difference. Third, manage any underlying disease—check your blood sugar, take prescribed heart meds, and talk to your doctor about smoking cessation. Fourth, watch for signs of infection: increased redness, swelling, foul odor, or a fever. If you notice these, seek care promptly to avoid deeper complications.
Lifestyle tweaks also play a role. Staying hydrated supports circulation, while a balanced diet supplies the building blocks for skin repair. Light exercise improves overall blood flow, but be careful not to over‑stress the ulcer site. And if you’re pregnant with ulcerative colitis, the “Ulcerative Colitis Pregnancy Guide” in our collection walks you through medication safety and flare‑up management—bridging gut health and chronic ulcer care.
Medication affordability matters, too. Our guides on buying cheap generic drugs like Allegra, Atenolol, and Zovirax show how to get quality meds without breaking the bank. The same principles apply when you need prescription dressings or antibiotics for a chronic ulcer—shopping smart can keep treatment sustainable.
In short, chronic ulcer sits at the crossroads of wound care, systemic disease, and daily habits. By understanding its ties to ulcerative colitis, peptic ulcer, and skin ulcer, you gain a clearer roadmap for healing. Below you’ll find articles that dive deeper into related topics—whether it’s spotting a mupirocin allergy, managing overactive bladder hydration, or learning home remedies for severe stomach pain. Use these resources to build a comprehensive plan that tackles the ulcer from every angle.
How Type 2 Diabetes Undermines Wound Healing and Skin Health
Explore how type 2 diabetes hampers wound healing, the underlying reasons, practical steps to improve skin health, and emerging treatments for stubborn ulcers.