Drug Name Confusion: How Similar-Sounding Medications Cause Errors and How to Stay Safe
When you hear drug name confusion, the dangerous mix-up between medications with similar names or spellings. Also known as look-alike sound-alike (LASA) errors, it’s one of the most common causes of preventable harm in healthcare. A pill meant for high blood pressure ends up in the hands of someone with diabetes. A sedative gets swapped for an antibiotic. These aren’t hypotheticals—they happen every day, often because two drugs sound almost identical when spoken aloud or look nearly the same on a label.
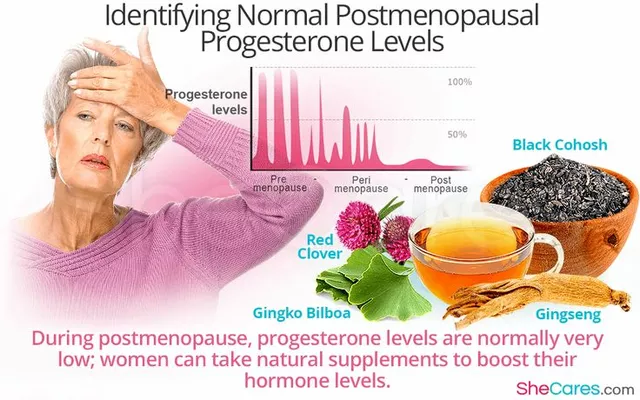
This isn’t just a pharmacy problem. It affects patients at home, nurses in hospitals, and even doctors writing prescriptions. generic names, the non-brand chemical names for drugs. Also known as international nonproprietary names, it are often long, complex, and easy to mishear—like hydroxyzine and hydralazine, or clonazepam and clonidine. Even brand names, the trademarked names companies use to sell drugs. Also known as proprietary names, it can trip you up. Pamelor and Premarin sound alike but treat completely different things—one for depression, the other for menopause. And when a pharmacist is rushing, or a doctor’s handwriting is unclear, the risk spikes.
It’s not just about spelling. It’s about how your brain processes sounds. Studies show that errors spike when drugs are ordered verbally over the phone—like when a nurse calls in a prescription. The brain hears "Zyrtec" and thinks "Zoloft." It hears "Lanoxin" and hears "Lotronex." One letter, one syllable, can change everything. And the consequences? Hospital visits, organ damage, even death. That’s why places like the FDA and Joint Commission push for medication errors, preventable mistakes in drug use that cause harm. Also known as adverse drug events, it prevention programs—using barcode scanners, double-checks, and clear labeling.
But you don’t have to wait for the system to fix itself. You can protect yourself right now. Always ask: "Is this the right drug for me?" Spell it out loud. Ask for the generic name. Check the pill against the bottle. If you’re on multiple meds, keep a simple list with both brand and generic names. Show it to every doctor and pharmacist. Don’t assume they know what you’re taking. And if a pill looks different than usual? Speak up. That’s not being difficult—that’s being smart.
The posts below dig into real cases where drug mix-ups happened—and how they were avoided. You’ll find guides on using two patient identifiers to stop errors, how generic absorption rates are tested for safety, why combination pills help seniors avoid confusion, and how digital tools are making it harder for drugs to be mistaken for one another. These aren’t theory pieces. They’re real-world tools used by clinics and hospitals to save lives. And they’re just as useful in your kitchen, your medicine cabinet, or your next doctor’s visit.
Look-Alike, Sound-Alike Medication Names That Cause Errors: Real Risks and How to Stop Them
Look-alike, sound-alike (LASA) drug names cause thousands of medication errors each year, leading to overdoses, hospitalizations, and even deaths. Learn which drugs are most dangerous, why mistakes keep happening, and how to protect yourself.