IBD Pregnancy: Managing Health for Mom and Baby
When navigating IBD pregnancy, the coexistence of inflammatory bowel disease and pregnancy, IBD in pregnancy you face a unique mix of challenges. A flare can affect fetal growth, while some IBD medicines cross the placenta. Understanding how the disease, the drugs, and the growing baby interact helps you make smarter choices and reduces anxiety.
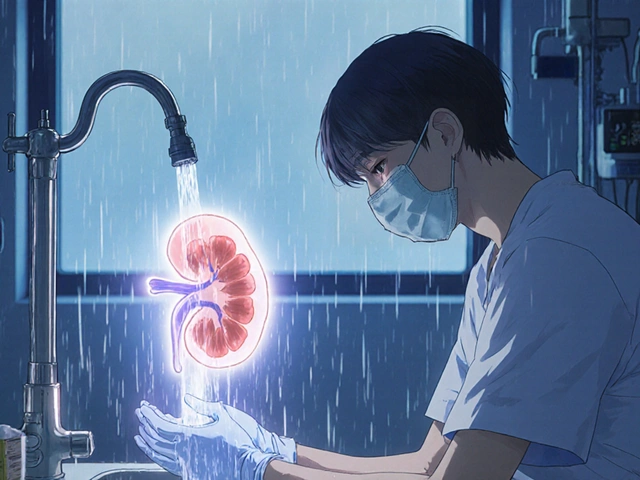
One of the first steps is to recognize what Inflammatory Bowel Disease (IBD), a chronic condition that includes Crohn’s disease and ulcerative colitis, actually does to the digestive system during pregnancy. IBD can cause malabsorption, anemia, and weight loss, which in turn influence Pregnancy, the 40‑week journey of fetal development, outcomes. Research shows that well‑controlled disease leads to birth weights similar to the general population, but uncontrolled inflammation raises the risk of preterm delivery. This relationship means that IBD pregnancy requires proactive disease monitoring and tailored treatment plans.
Key Considerations for a Healthy IBD Pregnancy
Medication safety sits at the core of any IBD pregnancy plan. Not all drugs are created equal; some biologics like anti‑TNF agents have a solid safety record, while steroids and certain immunomodulators need careful timing. Medication safety, evaluating drug risks versus benefits during gestation, therefore becomes a collaborative decision between you, a gastroenterologist, and an obstetrician. When a flare threatens, the goal is to choose the least risky option that still controls inflammation. This balance influences flare management, which directly impacts fetal health.
Nutrition is another pillar. IBD can deplete iron, folate, vitamin B12, and calcium—nutrients essential for a growing baby. Prenatal nutrition, the diet and supplement plan for pregnant women, should therefore include iron‑rich foods, folic‑acid supplements, and possibly vitamin D. Working with a dietitian can help you avoid trigger foods while ensuring you get enough calories and protein. Good nutrition not only supports the baby but also reduces the chance of a flare caused by nutritional deficiencies.
Regular monitoring ties everything together. Blood tests, stool markers, and ultrasound scans give a clear picture of disease activity and fetal growth. When labs show rising inflammatory markers, you can adjust medication before a full‑blown flare occurs. This proactive approach exemplifies the semantic triple: "IBD pregnancy requires continuous monitoring," and "continuous monitoring influences medication safety," creating a feedback loop that protects both mother and child.
Beyond the medical side, mental well‑being matters. Anxiety about drug side effects or baby outcomes can trigger stress‑related gut symptoms. Counseling or support groups provide emotional relief and practical tips from other parents who have walked the same path. When you feel supported, adherence to treatment improves, which in turn lowers flare risk—a clear example of how emotional health influences IBD management.
Finally, postpartum care deserves attention. After delivery, breastfeeding decisions intersect with medication choices. Some biologics are compatible with nursing, while others require a short washout period. Planning ahead with your care team ensures a smooth transition, protecting newborn immunity while maintaining disease control.
All these pieces—disease control, safe meds, nutrition, monitoring, mental health, and postpartum planning—form a comprehensive roadmap for IBD pregnancy, the management of inflammatory bowel disease during pregnancy,. Below you’ll find a curated list of articles that dive deeper into each of these topics, offering practical tips, medication guides, and real‑world stories to help you navigate this journey with confidence.
Ulcerative Colitis Pregnancy Guide: Risks, Meds & Delivery Tips
A comprehensive guide on ulcerative colitis and pregnancy covering fertility, medication safety, flare management, delivery options, and postpartum care.