Most people assume that if two pills have the same active ingredient, they’re the same. But that’s not true when it comes to inactive ingredients. These are the fillers, dyes, and preservatives that make up most of your pill-sometimes over 90%. And for people with allergies or intolerances, these seemingly harmless additives can trigger serious reactions. The problem isn’t rare. A 2019 study from Brigham and Women’s Hospital and MIT found that 90% of all oral medications in the U.S. contain at least one ingredient that can cause problems for sensitive patients. That includes lactose, gluten, food dyes, soy, and even traces of peanut oil. And here’s the catch: generic versions often have different inactive ingredients than brand-name drugs-even when the active ingredient is identical.
What Are Inactive Ingredients, and Why Do They Matter?
Inactive ingredients, also called excipients, don’t treat your condition. They’re there to help the medicine work: to bind the pill together, make it easier to swallow, preserve it, or give it color. But for some people, they’re dangerous. Lactose, for example, is in more than 20% of prescription drugs. If you have a severe milk protein allergy, even a tiny amount can cause hives, swelling, or anaphylaxis. Gluten shows up in pills for people with Celiac disease, triggering intestinal damage. Food dyes like Red #40 or Yellow #5 can cause reactions in kids with sensitivities. And bisulfites, used as preservatives, can trigger asthma attacks in up to 5% of asthmatics.The issue isn’t just about allergies. Some people can’t tolerate FODMAP sugars like lactulose or sorbitol, which are in about half of all medications. These can cause bloating, cramps, and diarrhea in people with IBS. And because these ingredients aren’t always labeled clearly, many patients don’t realize why they feel worse after switching to a generic.
Brand vs. Generic: The Hidden Differences
The FDA requires generic drugs to match the brand-name version in strength, dosage, and active ingredient. But it doesn’t require them to match the fillers. That means a 10mg tablet of Singulair® might contain lactose, while the 4mg version doesn’t. The brand-name version might use corn starch, while the generic uses wheat starch. One version might be dyed with Red #40; the other might be white.This isn’t a glitch-it’s standard practice. Manufacturers choose different excipients based on cost, availability, and patent restrictions. The result? You might take the same medicine for years without issue, then switch to a generic and suddenly get a rash, stomach pain, or breathing trouble. The American Pharmacists Association says 87% of pharmacists have seen patients react to this exact scenario.
And it’s not just generics. Even different batches of the same brand can change ingredients over time. A 2021 Safe Medication report warns: “Always check the most current inactive ingredient list. Ingredients may change without notice.”
Which Inactive Ingredients Are Most Dangerous?
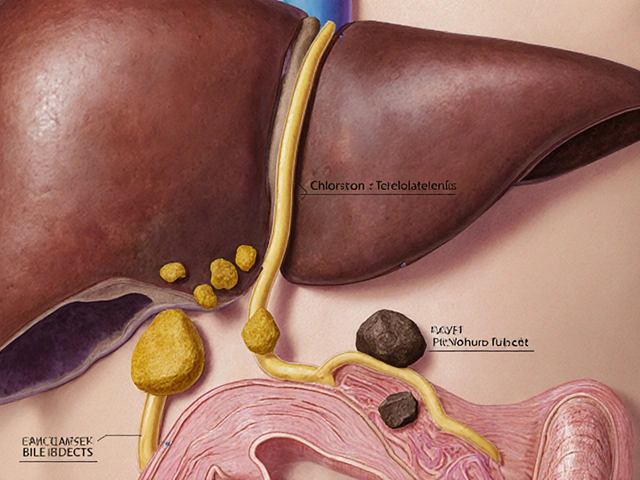
Not all excipients are equal. Some are far more likely to cause trouble. Here are the top eight to watch for:- Lactose - Found in over 20% of prescription drugs. Can trigger reactions in people with milk protein allergy or severe lactose intolerance.
- Gluten - Even trace amounts can damage the intestines in people with Celiac disease. Often hidden in starches derived from wheat.
- FD&C Dyes - Yellow #5, Red #40, Blue #1, and others are linked to hyperactivity in children and allergic reactions in sensitive adults.
- Bisulfites - Used in injectables and some oral meds. Can cause wheezing, chest tightness, and anaphylaxis in asthmatics.
- Gelatin - Common in capsules. Derived from animal collagen. A problem for vegans, vegetarians, or those with beef or pork allergies.
- Soy oil - Used as a lubricant. Can trigger reactions in people with soy allergy, though highly refined versions are often tolerated.
- Peanut oil - Rare, but strictly labeled by the FDA. Still, some patients avoid it entirely.
- Shellfish derivatives - Found in some injectables. Can trigger reactions in people with seafood allergies.
Some medications contain multiple high-risk ingredients. A single pill might have lactose, gelatin, and Red #40. For someone with multiple allergies, that’s a minefield.

How to Find Out What’s in Your Medicine
You can’t rely on your doctor to know. Most aren’t trained to check excipients. Pharmacists are your best bet. Here’s how to get the facts:- Check the package insert - Every prescription comes with a paper insert. Look for the “Inactive Ingredients” section.
- Ask your pharmacist - Pharmacists have access to databases like Micromedex or Lexicomp that list every ingredient. They can compare brand and generic versions side by side.
- Use the FDA’s database - The FDA’s Drugs@FDA portal lets you search for drug labels. Type in the brand or generic name, then click “Labeling” to see the full ingredient list.
- Download the Inactive Ingredient Finder - A free app launched in 2023 by MIT researchers tracks over 98% of U.S. medications. It shows allergens, gluten, and lactose content instantly.
- Read OTC labels - Over-the-counter meds list ingredients on the Drug Facts panel. Look under “Inactive Ingredients.”
Don’t assume “sugar-free” or “dye-free” means safe. Some products still contain hidden allergens like gelatin or soy.
What to Do If You Have a Known Allergy
If you know you react to certain ingredients, take control before your next prescription:- Get tested - See an allergist to confirm which ingredients trigger you. Skin prick tests or blood tests can identify sensitivities to milk, gluten, soy, and more.
- Create a personal list - Write down every ingredient you can’t tolerate. Include brand names and generic equivalents that contain them.
- Carry a medication card - Keep a small card in your wallet listing your allergens. Show it to any new prescriber or pharmacist.
- Ask for alternatives - Say: “I have a severe allergy to lactose. Is there a version of this drug without it?” Many drugs have multiple formulations. For example, some metformin tablets are lactose-free.
- Never switch without checking - Even if your doctor says “it’s the same,” always verify the inactive ingredients before taking a new version.
Some pharmacies now use electronic systems that flag allergens in prescriptions. Ask if your pharmacy offers this service. As of 2023, 42% of U.S. pharmacies have this feature-up from just 17% in 2020.
Why This Problem Persists
You’d think this would be fixed by now. But regulation is lagging. In the U.S., only peanut oil and bisulfites must be clearly labeled. Lactose? Gluten? Dyes? No mandatory labeling. The FDA proposed rules in 2022 to require clearer labeling of eight high-risk ingredients-but it’s still pending.Meanwhile, the EU has required full excipient disclosure since 2019. The result? A 37% drop in adverse reactions. In the U.S., only 12% of generic medications offer allergen-free versions. The pharmaceutical industry is slowly responding: 68% of major companies have improved labeling since the 2019 MIT study. But change is slow.
And the risk grows with age. About 30% of people over 65 take five or more pills daily. Each one could contain a new allergen. Multiply that over months or years, and you’re building up exposure without realizing it.
What’s Changing-and What to Expect
The tide is turning, but slowly. By 2027, IQVIA predicts 30% of new generic drugs will include at least one allergen-free version. Insurance companies and patient advocacy groups are pushing for it. The American Medical Association has called for mandatory labeling of all excipients by 2026.Some companies are stepping up. Specialty pharmacies now offer compounded medications without common allergens. Online tools like the Inactive Ingredient Finder are becoming essential. And more patients are speaking up-demanding transparency.
For now, the responsibility falls on you. You can’t wait for regulations to catch up. You need to know what’s in your pills. You need to ask questions. And you need to trust your body-if you feel different after a switch, it’s not in your head. It might be in the filler.
Can generic medications cause allergic reactions even if they have the same active ingredient as the brand?
Yes. Generic medications must match the brand in active ingredient strength and effectiveness, but they can-and often do-use different inactive ingredients like lactose, gluten, dyes, or preservatives. These can trigger allergic reactions or intolerances in sensitive individuals, even if the active ingredient is identical.
How do I find out what inactive ingredients are in my medication?
Check the package insert that comes with your prescription, ask your pharmacist directly, or search the FDA’s Drugs@FDA portal. For over-the-counter drugs, look at the Drug Facts label under “Inactive Ingredients.” The free Inactive Ingredient Finder app, developed by MIT, also tracks over 98% of U.S. medications and flags allergens like lactose, gluten, and dyes.
Are there medications available without lactose or gluten?
Yes. Many drugs have multiple formulations, and some manufacturers now offer lactose-free or gluten-free versions. For example, certain brands of metformin, levothyroxine, and ibuprofen are available without lactose. Compounded medications from specialty pharmacies can also be made without common allergens. Always ask your pharmacist: “Is there a version of this drug without lactose or gluten?”
Why don’t drug labels always list allergens like lactose or gluten?
In the U.S., the FDA only requires labeling of a few high-risk ingredients like peanut oil and bisulfites. Lactose, gluten, and most food dyes are not legally required to be labeled as allergens-even though they can cause serious reactions. This lack of mandatory disclosure makes it hard for patients to identify safe options. The EU requires full excipient labeling, which has reduced adverse reactions significantly.
Should I talk to my allergist about medication ingredients?
Yes. If you have food allergies or intolerances, your allergist can help identify which medication ingredients you need to avoid. They can perform tests to confirm sensitivities and help you create a personalized list of unsafe excipients. Bring this list to every doctor’s visit and pharmacy visit to ensure safe prescribing.
Can I trust a “sugar-free” or “dye-free” medication label?
Not always. “Sugar-free” might still contain lactose or gelatin. “Dye-free” might still contain soy oil or gluten-derived starches. Always read the full list of inactive ingredients. Terms like “natural” or “hypoallergenic” are not regulated and don’t guarantee safety. Only the complete ingredient list tells you what’s really in the pill.










sean whitfield
December 4, 2025 AT 17:22 PMSo the government lets Big Pharma poison us with lactose and dye because it's cheaper. Classic. We're not patients. We're test subjects. And the FDA? Just a rubber stamp for corporate greed.
Jennifer Patrician
December 5, 2025 AT 11:38 AMLactose in pills? That's not an accident. It's a control mechanism. They want you dependent. They want you weak. You think they care if you're allergic? They profit off your suffering.
Mark Curry
December 5, 2025 AT 21:16 PMI never thought about this before. My stomach's been acting up since I switched to generic metformin. Maybe it's not me. Maybe it's the filler. I'll check with my pharmacist tomorrow.
Manish Shankar
December 7, 2025 AT 20:46 PMThis is a deeply concerning issue that requires immediate regulatory attention. The absence of mandatory labeling for excipients represents a significant gap in patient safety protocols. I urge all healthcare professionals to prioritize this matter.
Lynette Myles
December 9, 2025 AT 13:07 PMThey lied. Again.
Annie Grajewski
December 10, 2025 AT 01:56 AMOMG I thought I was just weird for getting hives after my generic Adderall. Turns out it had Red #40. My doctor didn't even know. I'm gonna start a petition. #FreeMyPills
Rupa DasGupta
December 11, 2025 AT 14:22 PMI've been suffering for years and no one listens. My kids cry after their ADHD meds. They say it's 'just anxiety'. But I know. It's the soy. It's always the soy. 😭
Marvin Gordon
December 13, 2025 AT 08:00 AMThis is why you have to be your own advocate. Don't wait for the system to fix itself. Ask. Research. Push back. Your health is worth fighting for. I've done it. You can too.
ashlie perry
December 14, 2025 AT 12:34 PMI told you all this was a cover-up. The FDA, the pharma giants, the doctors-they're all in on it. They want you sick. They want you dependent. The pills are weapons. You're being weaponized.
James Moore
December 15, 2025 AT 21:37 PMLet me be clear: this is not an isolated incident. This is the inevitable result of decades of deregulation, the erosion of public trust, and the moral bankruptcy of a capitalist healthcare system that treats human beings as cost centers. The FDA’s inaction is not incompetence-it’s complicity. We are not patients. We are consumers. And consumers are expendable.
Lucy Kavanagh
December 16, 2025 AT 16:15 PMI'm British and I'm horrified. Over here we've had full ingredient disclosure since 2019. It's basic human decency. How can America still be this backwards? I've sent this to my MP. Someone needs to do something.
Chris Brown
December 16, 2025 AT 21:16 PMThis is what happens when you let the weak and the fearful dictate policy. People with allergies should just take responsibility. If you can't handle a little lactose in your medicine, maybe you shouldn't be taking medicine at all. Weakness is not a right.