When you’re pregnant and have asthma, every decision about your health feels heavier. You’re not just thinking about yourself anymore-you’re thinking about your baby. The fear isn’t irrational: asthma medication pregnancy worries are common. Many women wonder if their inhaler could cause birth defects, or if skipping a dose might be safer. The truth? Not treating asthma is far riskier than using the right medications.
Why Uncontrolled Asthma Is More Dangerous Than Medication
It’s easy to assume that avoiding drugs during pregnancy is the safest path. But when asthma flares up, your body struggles to get enough oxygen. That means less oxygen for your baby too. Uncontrolled asthma increases the risk of preeclampsia, preterm birth, and low birth weight. Studies show these risks are 30% to 60% higher when asthma isn’t managed well. In fact, research from the National Asthma Education and Prevention Program found that 20% to 45% of pregnant women with asthma have flare-ups-most between weeks 24 and 36. That’s not a small chance. It’s a real, measurable danger.
Doctors don’t recommend stopping asthma meds because they’re scared of side effects. They recommend continuing them because the data is clear: keeping asthma under control gives your baby the best shot at a healthy start. The American College of Allergy, Asthma, and Immunology says the benefits of well-controlled asthma outweigh any theoretical risks from medications. And that’s not just opinion-it’s backed by data from over 1.2 million pregnancies.
Which Asthma Medications Are Safe During Pregnancy?
Not all asthma drugs are created equal when you’re pregnant. The safest options are inhaled medications because they target your lungs directly and barely enter your bloodstream. That means less exposure for your baby.
Inhaled corticosteroids (ICS) are the first-line treatment. Among these, budesonide has the strongest safety record. Over 1,000 documented pregnancies show no increased risk of birth defects. It’s been studied longer and more thoroughly than any other ICS. Beclomethasone and fluticasone propionate are also considered safe, with large studies confirming no rise in major congenital malformations. In fact, a 2021 meta-analysis of nearly 124,000 pregnancies found budesonide’s adjusted risk for birth defects was almost identical to women not taking any asthma meds-1.01 versus 1.00.
For quick relief during an attack, albuterol (salbutamol) is your go-to. It’s been used for decades in pregnancy with no link to birth defects. The Allergy & Asthma Network reviewed data from more than a million pregnancies and found no safety red flags. Levalbuterol, a cleaner version of albuterol, is equally safe.
If you need long-term control beyond an ICS, your doctor might add a long-acting beta-agonist (LABA) like formoterol or salmeterol. But these are only used in combination with an ICS-never alone. Data from over 37,000 pregnancies show no increased risk of problems when used this way.
Montelukast (Singulair), a leukotriene modifier, is another option. While not as powerful as ICS, it’s considered low-risk. The European Network of Teratology Information Services tracked over 1,000 pregnancies and found no significant rise in birth defects.
Medications to Avoid or Use With Extreme Caution
Not all asthma treatments are safe during pregnancy. Some carry clear risks.
Oral corticosteroids like prednisone are the biggest concern. A 2023 study of 1.8 million pregnancies found that taking them in the first trimester increased the risk of cleft lip or palate by 56%. They also raised the chance of preterm birth and low birth weight. These are powerful drugs, and while they’re sometimes necessary for severe flare-ups, they should be used for the shortest time possible and only when absolutely needed.
Theophylline is rarely used today because it requires blood tests to make sure the dose is right. It can interact with common antibiotics like erythromycin and cause toxicity. While it’s not proven to cause birth defects, it’s harder to manage safely than inhaled options.
Tiotropium (Spiriva), a long-acting anticholinergic, has almost no safety data in pregnancy. Only 324 pregnancies have been documented in global databases. GINA recommends avoiding it as a first choice.
Newer biologics like omalizumab, mepolizumab, and dupilumab are exciting for severe asthma-but not yet for pregnancy. While early data on omalizumab (from 715 pregnancies) is reassuring, there’s still too little information to recommend them routinely. Experts agree they should only be considered in rare, severe cases under close supervision.
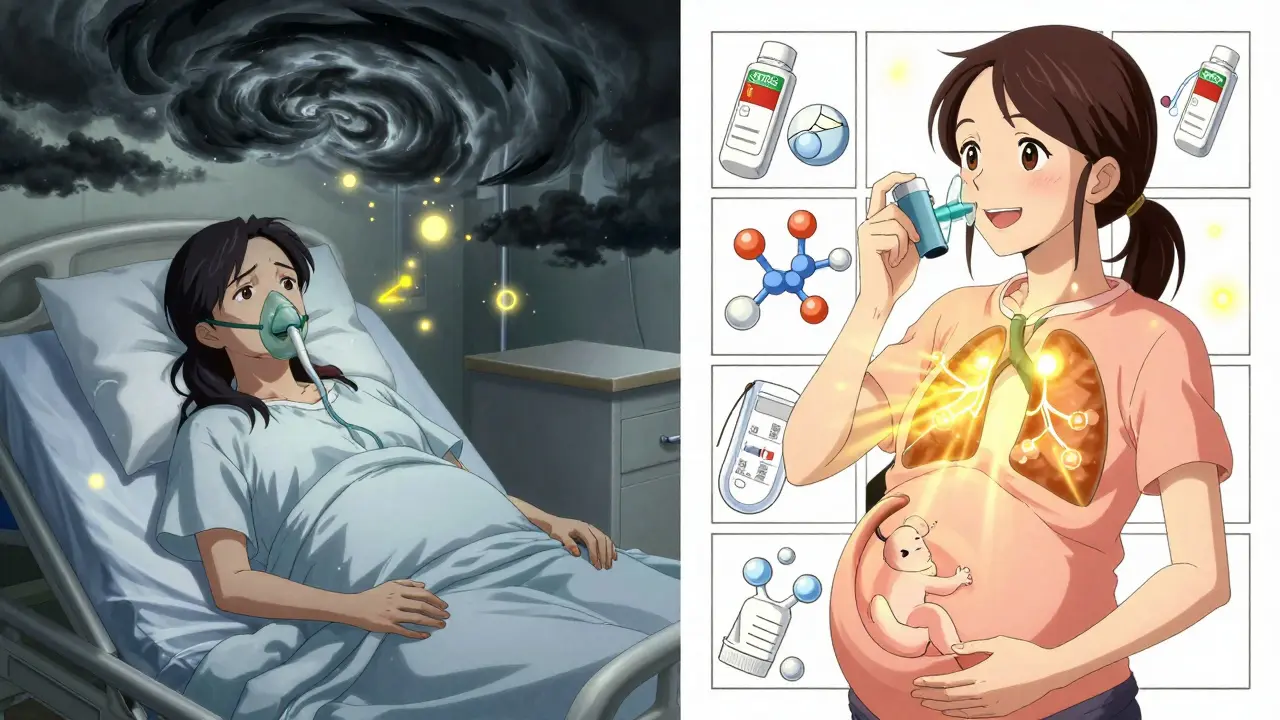
What Happens If You Stop Your Asthma Meds?
Many women stop their inhalers out of fear. But the consequences are real.
A 2021 study from the Canadian Asthma Primary Care Registry tracked 342 pregnant women with asthma. Of those who stopped their inhaled corticosteroids, 41% had at least one severe asthma attack requiring emergency care. Only 17% of women who kept taking their meds had the same outcome. That’s more than double the risk.
One woman in Seattle, 32, stopped her budesonide in her first trimester because her OB said, “Just see how you feel.” By week 28, she was in the ER with a near-fatal attack. Her baby was born at 34 weeks with a low birth weight. She didn’t need to go through that. Her asthma was stable before pregnancy. There was no reason to change anything.
Continuing your pre-pregnancy regimen isn’t reckless-it’s smart. A 2022 survey by the Allergy & Asthma Network found that 89% of pregnant women who stayed on their usual asthma meds had better outcomes than those who changed their treatment.
How to Monitor Your Asthma During Pregnancy
Control isn’t just about taking meds. It’s about tracking your symptoms and lung function.
Use a peak flow meter daily. Your goal is to stay above 80% of your personal best reading. Keep a symptom diary. Note coughing, wheezing, nighttime awakenings, and how often you use your rescue inhaler.
The Asthma Control Test (ACT) is a simple 5-question tool. Score 20 or higher? Your asthma is under control. Below 20? Talk to your doctor. You might need an adjustment.
Doctors recommend check-ins at 8, 16, 24, and 32 weeks-ideally with both your OB and your asthma specialist. If you’re in a rural area or have trouble getting to appointments, telehealth visits are now widely available. In 2023, nearly half of asthma patients used telemedicine during pregnancy, and it’s just as effective as in-person visits.

Environmental Triggers to Watch For
Medication isn’t the only tool in your belt. Reducing exposure to triggers can cut down on flare-ups.
Use allergen-proof mattress and pillow covers-they reduce dust mite exposure by 83%. Keep indoor humidity between 30% and 50% to stop mold growth (a 67% reduction). Remove carpets if you can-they trap allergens. Avoid cigarette smoke, strong perfumes, and air pollution. If you live in a city, check local air quality reports. On bad air days, stay indoors with windows closed and your air filter on.
These steps won’t replace medication, but they’ll make it easier to stay in control. Less exposure means less need for rescue inhalers-and less stress for you and your baby.
What About Breastfeeding?
Good news: almost all asthma medications are safe while breastfeeding. Inhaled corticosteroids and albuterol pass into breast milk in tiny, harmless amounts. You can keep using your inhalers without worry. In fact, keeping your asthma under control helps you care for your newborn better. Fatigue from breathing problems doesn’t help anyone.
There’s no need to pump and dump. No need to wait after using your inhaler. Just use it as directed. The benefits to you and your baby far outweigh any theoretical risk.
Final Thought: You’re Not Alone
You’re not the first pregnant woman to worry about asthma meds. In fact, 78% of women on asthma forums say they’re terrified of harming their baby. But the data doesn’t support that fear. The real danger isn’t the inhaler-it’s the uncontrolled asthma.
Your job isn’t to be perfect. It’s to be informed. Work with your doctors. Stick to your plan. Track your symptoms. And remember: taking your medication isn’t a compromise. It’s an act of care-for you, and for your baby.










Aysha Siera
January 19, 2026 AT 02:23 AMThe government and Big Pharma are pushing these meds hard because they make billions off pregnant women’s fear
They don’t want you to know natural remedies work better
My cousin stopped inhalers and ate turmeric and ginger-baby was born healthy at 42 weeks
They’ll call you crazy but the truth is buried under clinical trials paid for by drug companies
rachel bellet
January 19, 2026 AT 22:41 PMLet’s be clear: the risk-benefit calculus is unequivocal. Inhaled corticosteroids, particularly budesonide, demonstrate a teratogenic risk profile indistinguishable from background population rates (OR 1.01, 95% CI 0.94–1.09)
Conversely, uncontrolled maternal hypoxia triggers inflammatory cascades that directly impair placental perfusion, elevating odds of preterm birth by 47% and IUGR by 52%
Discontinuation of maintenance therapy constitutes a preventable iatrogenic hazard-this isn’t ‘natural parenting,’ it’s negligence masked as caution
Pat Dean
January 20, 2026 AT 12:22 PMOf course they say it’s safe-these doctors are all on the payroll of Big Pharma
They don’t care about your baby, they care about the next quarterly report
My sister took albuterol and her kid had a heart defect-no one talks about that
Why is no one asking who funded these ‘studies’?
It’s not about health, it’s about profit
Jay Clarke
January 20, 2026 AT 23:24 PMLook, I get it-you’re scared. I was too when my wife was pregnant
But here’s the thing: asthma isn’t just ‘breathing funny’-it’s your body screaming for oxygen
And if you’re gasping, your baby’s drowning in slow motion
That inhaler? It’s not poison. It’s a lifeline
Staying off meds because you’re scared of side effects that don’t even exist? That’s not bravery. That’s suicide with a baby inside you
Selina Warren
January 22, 2026 AT 05:56 AMYOU ARE STRONGER THAN YOUR FEAR
Every time you reach for that inhaler, you’re choosing life-for you, for your baby
Don’t let fear write your story. Let data, let science, let love write it
You’re not risking your baby by using meds-you’re risking them by NOT using them
Stop listening to the noise. Breathe. Take your medicine. You’ve got this
Joni O
January 23, 2026 AT 12:47 PMthank you for this post i was so scared but reading this made me feel less alone
i started using my budesonide again after week 12 and my peak flow is up 20%
no more midnight coughing fits
my baby is kicking like crazy now-i think they’re happy too
you’re right-this isn’t about being perfect, it’s about being smart
Ryan Otto
January 23, 2026 AT 17:27 PMThe data presented is statistically convenient but methodologically suspect. The 1.2 million pregnancy cohort lacks stratification for socioeconomic confounders, and the majority of studies originate from U.S. institutions with vested pharmaceutical interests.
Furthermore, the normalization of pharmacological intervention during gestation reflects a broader pathological trend: the medicalization of natural biological processes.
One must question whether the perceived safety is not merely the absence of acute harm, rather than the presence of long-term epigenetic integrity.
Max Sinclair
January 24, 2026 AT 20:18 PMI appreciate how clearly this breaks things down-seriously, thank you.
I was one of those women who stopped my inhaler because my mom said ‘pregnancy isn’t the time for chemicals.’
Turns out, my asthma got worse and I ended up in the ER at 28 weeks.
Started back on budesonide, and within two days I could sleep again.
My daughter is now 8 months old and breathing just fine.
Don’t let fear silence the science. You’re doing the right thing by listening to your doctor.
Naomi Keyes
January 25, 2026 AT 12:41 PMWhile the article cites multiple studies, it fails to acknowledge the limitations of observational data-particularly the absence of double-blind, placebo-controlled trials in pregnant populations, which are ethically constrained.
Moreover, the conflation of ‘no increased risk’ with ‘proven safety’ is a logical fallacy.
Additionally, the promotion of telehealth as ‘equivalent’ to in-person care ignores disparities in device access, digital literacy, and the loss of physical auscultation.
And yet-despite these caveats-I still agree with the conclusion. Just… please, cite the limitations.
Zoe Brooks
January 27, 2026 AT 11:06 AMMy OB told me to stop my inhaler. My pulmonologist told me to keep it.
I listened to the pulmonologist.
My son is two now, runs like a cheetah, and still steals my budesonide canister to ‘pretend’ he’s a superhero.
He doesn’t know he was a miracle.
But I do.
And I’m never letting fear win again.