Chronic Pain Meds: What Works, What to Avoid, and How to Stay Safe
When you live with chronic pain meds, medications used to manage persistent pain lasting more than three months. Also known as long-term pain relievers, they’re not just about numbing discomfort—they’re about helping you move, sleep, and live again. Unlike short-term pain from a sprain or surgery, chronic pain doesn’t go away after the injury heals. It becomes its own condition, often tied to arthritis, nerve damage, fibromyalgia, or past surgeries. That’s why choosing the right chronic pain meds isn’t a one-size-fits-all decision. It’s about matching the drug to your body, your lifestyle, and your risks.
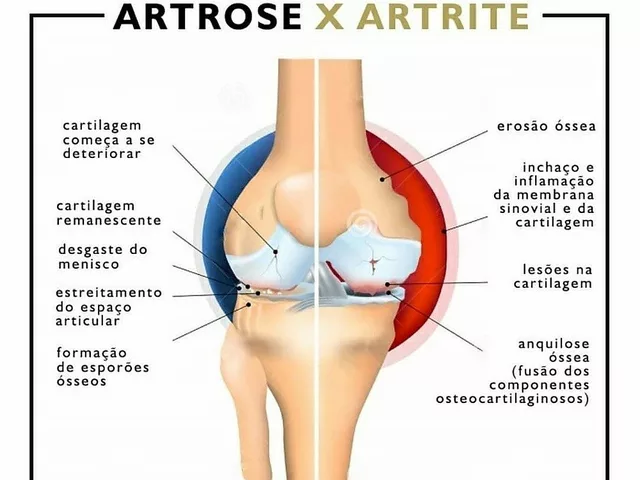
Many people start with NSAIDs, nonsteroidal anti-inflammatory drugs like ibuprofen or naproxen that reduce swelling and pain. Also known as over-the-counter painkillers, they’re the first line for joint and muscle pain. But if they don’t cut it, doctors may turn to opioid alternatives, medications that target nerve pain without the addiction risk of opioids. This includes drugs like gabapentin, duloxetine, or even topical lidocaine patches. These aren’t just backups—they’re often safer and more effective for nerve-related pain like diabetic neuropathy or sciatica. And while opioids still get prescribed, guidelines now push hard to avoid them unless absolutely necessary. Why? Because tolerance builds fast, side effects pile up, and withdrawal can be brutal.
What you won’t find in most doctor’s offices is a magic pill. Chronic pain meds work best when paired with movement, sleep, and stress management. That’s why the posts here cover real-world issues: how indomethacin compares to other NSAIDs, what to watch for with statin-related muscle cramps, and how to spot a mupirocin allergy before it turns serious. You’ll also find guides on medication safety, how to buy generic versions without getting scammed, and what to do when one drug stops working.
This isn’t about chasing the strongest drug. It’s about finding the right balance—enough relief to get through your day, without losing control of your health. Whether you’re managing back pain, arthritis, or nerve damage, the goal is simple: live better, not just hurt less. Below, you’ll find clear, no-fluff guides on exactly which meds help, which ones to question, and how to talk to your doctor about your options.
Compare Pamelor (Nortriptyline) with Alternatives for Depression and Chronic Pain
Compare Pamelor (nortriptyline) with SSRIs, SNRIs, and other antidepressants for depression and nerve pain. Learn which alternatives offer better side effect profiles, faster relief, or lower cost.