A severe hypertensive crisis isn't just a bad day with high blood pressure. It’s a medical emergency where systolic pressure spikes above 180 mmHg or diastolic climbs past 120 mmHg-sometimes within minutes-and starts tearing through your organs. Think brain, heart, kidneys, eyes. This isn’t theoretical. People end up in the ICU because they took a common cold medicine with their antidepressant, ate aged cheese while on an MAOI, or doubled up on a weight-loss pill thinking it would help more. And in most cases, no one saw it coming.
How a Normal Drug Becomes a Danger
Most medications work fine on their own. But when two or more interact, the body’s natural balance breaks. One drug might block the system that normally keeps blood pressure in check. Another might flood your system with norepinephrine, the chemical that tightens blood vessels. The result? Blood pressure rockets. This isn’t rare. Around 15-20% of all secondary hypertension cases come from drug interactions, and that number is likely low because many cases go unreported.
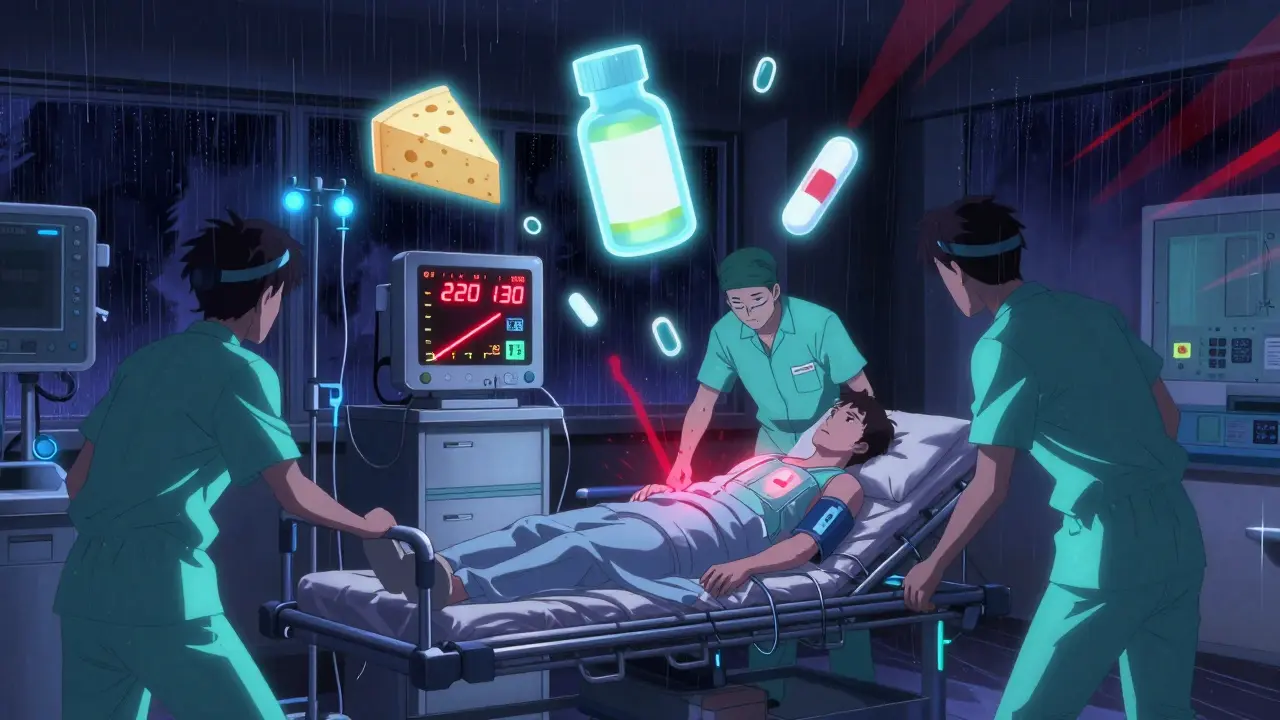
Take cocaine and propranolol. Cocaine raises blood pressure by triggering norepinephrine release. Propranolol blocks beta receptors, which normally help dilate blood vessels. Without that counterbalance, the alpha receptors take over-unopposed-and squeeze arteries like a vise. Cases have shown systolic pressure hitting 220 mmHg in under an hour. No warning. No symptoms until it’s too late.
Then there’s licorice. Yes, candy. Eating just a few pieces a day can cause a crisis. Licorice contains glycyrrhizin, which blocks the enzyme that breaks down cortisol. Cortisol then acts like aldosterone, a hormone that makes your body hold onto salt and water. Blood volume swells by 10-15%. Potassium drops. Sodium spikes. Blood pressure climbs slowly over weeks-but when it hits, it hits hard. And doctors often miss it because they’re looking for kidney disease, not candy.
The Hidden Triggers You’re Probably Using
Some of the most dangerous interactions come from things you think are harmless.
- MAOIs and tyramine-rich foods: MAOIs like phenelzine or selegiline stop your body from breaking down tyramine, a compound in aged cheese, cured meats, soy sauce, and tap beer. When tyramine builds up, it forces norepinephrine out of nerve endings, causing sudden, violent spikes. Systolic pressure can jump 50-100 mmHg in 30-120 minutes. One patient on Reddit described waking up at 220/130 after eating cheddar with their selegiline. They spent three days in the ICU.
- Venlafaxine and stimulants: Venlafaxine (Effexor) at doses above 300 mg/day can raise diastolic pressure above 90 mmHg. When combined with ADHD meds like Adderall or even OTC decongestants like pseudoephedrine, the risk jumps 40% compared to historical data. Many patients report headaches or blurred vision-but doctors dismiss it as stress or migraines.
- Cyclosporine and calcium channel blockers: Used in transplant patients, cyclosporine causes hypertension in up to half of users. It reduces sodium excretion and increases vasoconstrictors. When paired with drugs like diltiazem, the effect multiplies. In 55% of cases, this was mistaken for organ rejection, leading to higher immunosuppressant doses-and worse blood pressure.
- Sibutramine and other weight-loss drugs: Even though sibutramine was pulled from the U.S. market in 2010, it still shows up in unregulated supplements. It raises systolic and diastolic pressure by 7 mmHg in people who already have hypertension. That might sound small, but in someone with borderline high blood pressure, it’s enough to push them into crisis territory.

Why Doctors Miss It-And What You Can Do
A 2022 study found that 65% of emergency doctors don’t routinely check for drug interactions when someone shows up with a hypertensive crisis. Why? Because they’re trained to look for kidney disease, pheochromocytoma, or adrenal tumors-not the patient’s OTC cold medicine.
Patients aren’t blameless, either. A 2021 survey showed 68% of people who had a drug-induced crisis had complained of unexplained headaches or vision changes to their doctor-but only 22% had their meds reviewed. Most assume their doctor knows what they’re taking. They don’t. You have to tell them.
Here’s what you need to do:
- Make a full list of everything you take: Prescription, OTC, supplements, herbal teas, even licorice candy. Write it down. Bring it to every appointment.
- Ask: “Could this interact with anything else I’m on?” Don’t wait for your doctor to bring it up. Especially if you’re on antidepressants, blood pressure meds, or immunosuppressants.
- Know the red flags: Sudden, severe headache, chest pain, blurred vision, shortness of breath, nosebleeds, confusion. If you’re on a high-risk drug and get one of these, go to the ER. Don’t wait.
- Use apps: Tools like “MAOI Diet Helper” improved adherence by 78% in a Mayo Clinic study. Even if you’re not on an MAOI, apps that flag interactions can save your life.
What Happens in the ER-And How It’s Treated
If you’re admitted with a hypertensive emergency, they won’t just give you a pill and send you home. They need to bring pressure down-slowly and safely. Dropping it too fast can cause stroke or heart attack.
The treatment depends on what caused it:
- MAOI-tyramine crisis: IV phentolamine is the gold standard. It blocks alpha receptors and works in under 20 minutes with 92% success. Labetalol is also used and is 85% effective.
- Cyclosporine-induced: Calcium channel blockers like amlodipine are preferred. They’re 78% effective at reducing pressure without harming kidney function.
- Mineralocorticoid excess (licorice, steroids): Stopping the trigger is key. Blood pressure can take weeks to normalize. Potassium supplements and fluid restriction are often needed.
- Cocaine or stimulant-related: Benzodiazepines like lorazepam calm the nervous system and reduce adrenaline. Nitroglycerin or nitroprusside may be used for rapid control.
One critical point: You’re not getting a simple blood pressure pill. The goal isn’t just to lower the number-it’s to stop organ damage. That means continuous IV monitoring, frequent blood tests, and often ICU-level care.
What’s Changing-and What’s Still Broken
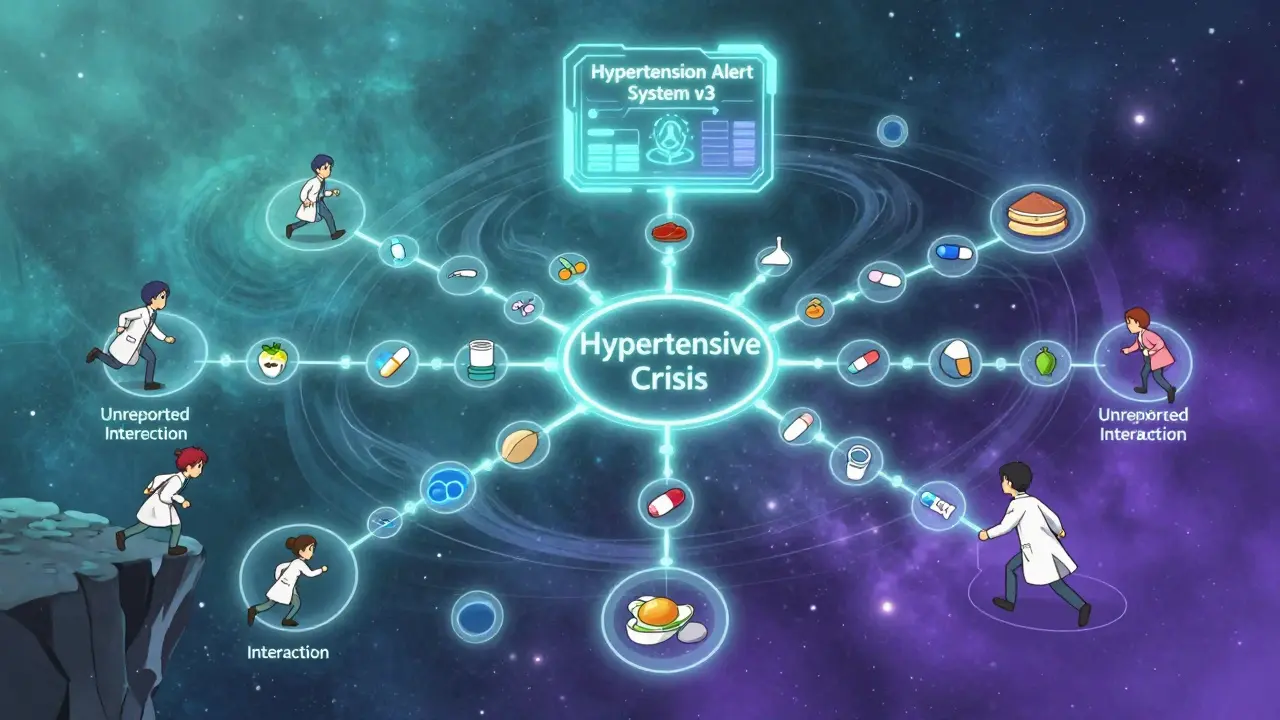
There’s progress. The FDA now requires black box warnings on all MAOIs about tyramine interactions-up from 65% in 2015 to 100% today. Prescription monitoring programs have cut MAOI-related crises by 28% in states that use them. A new AI tool called the “Hypertension Interaction Alert System” is in phase 3 trials and predicts severe events with 92% accuracy by scanning 15,000+ known interactions.
But gaps remain. Only 12% of OTC decongestant labels mention hypertension risk. Most weight-loss supplements still contain hidden stimulants. And genetic testing for CYP2D6 variants-which can identify people 3.2 times more likely to have a bad reaction to certain antidepressants-isn’t routine anywhere.
The American Heart Association estimates drug-induced crises cost $2.3 billion a year in unnecessary ER visits and hospitalizations. That’s preventable. But prevention requires two things: better systems and better communication.
Final Reality Check
You’re not invincible. Just because you’ve been on a medication for years doesn’t mean it’s safe with everything else you’ve added since. A new supplement. A different painkiller. A friend’s recommendation for “natural energy.” That’s how it starts.
The most dangerous part? It doesn’t feel like a crisis until it’s too late. No chest pain. No dizziness. Just a headache you ignore. A nosebleed you wipe off. A blurry vision you blame on screen time.
Know your meds. Know your risks. Speak up. If you’re on an MAOI, avoid aged cheese, cured meats, and soy sauce. If you’re on venlafaxine above 225 mg/day, get your blood pressure checked every three months-even if you feel fine. If you’re on cyclosporine after a transplant, don’t assume your high pressure is rejection-it might be your cold medicine.
This isn’t about fear. It’s about awareness. And awareness saves lives.
Can over-the-counter cold medicine cause a hypertensive crisis?
Yes. Decongestants like pseudoephedrine and phenylephrine are stimulants that raise blood pressure. If you’re on MAOIs, venlafaxine, or other antidepressants, even one dose can trigger a crisis. Many OTC labels don’t warn about this risk. Always check with your pharmacist before taking any cold, flu, or allergy medicine if you’re on blood pressure or psychiatric meds.
Is it safe to eat cheese if I’m on an antidepressant?
Only if your antidepressant is not an MAOI. If you’re taking phenelzine, tranylcypromine, or selegiline (especially the patch), avoid aged cheeses (cheddar, parmesan, blue cheese), cured meats, tap beer, soy sauce, and fermented foods. These contain tyramine, which can cause a dangerous spike in blood pressure. Newer antidepressants like SSRIs and SNRIs (e.g., sertraline, venlafaxine) don’t have this risk.
How long does it take for blood pressure to return to normal after stopping the triggering drug?
It depends on the drug. For MAOI-tyramine reactions, pressure often drops within hours after treatment. For mineralocorticoid excess from licorice or steroids, it can take weeks-even after stopping the substance-because the hormone receptors stay activated. Cyclosporine-induced hypertension may improve in days but often requires ongoing medication. Always follow up with your doctor for monitoring.
Can genetic testing predict if I’m at risk for a drug-induced hypertensive crisis?
Yes, for certain drugs. Testing for CYP2D6 gene variants can identify people who metabolize antidepressants like venlafaxine or nortriptyline too slowly, leading to toxic buildup and higher risk of severe hypertension. These patients are 3.2 times more likely to have a crisis. While not yet standard, this testing is becoming available through specialized clinics and may be recommended if you’ve had unexplained high blood pressure on these meds.
Are there any new tools or apps to help prevent these interactions?
Yes. The FDA approved a decision-support tool in early 2023 that flags dangerous combinations in electronic health records, reducing MAOI-related emergencies by 40% in trials. Apps like “MAOI Diet Helper” and “Drug Interaction Checker” (from Medscape or Epocrates) can alert you to risks before you take a new medication. Use them. They’re free, easy, and could save your life.










claire davies
December 23, 2025 AT 16:54 PMOkay but have y’all ever considered that licorice candy is basically a silent assassin? I used to eat a whole bag of those black ones every week thinking it was just a ‘comfort snack’ - turns out my BP was creeping up for months. My doctor didn’t even blink until I mentioned it. Now I swap it for dark chocolate and my numbers are stable. Weird how something so sweet can be so sneaky. 🍫
Harsh Khandelwal
December 24, 2025 AT 07:04 AMlol so now even my morning coffee is gonna kill me? next they’ll say breathing is dangerous. they’re just scared people will stop taking meds and start using ‘natural remedies’ like yoga and sunlight. also who even eats aged cheese anymore? it tastes like regret.
Lindsey Kidd
December 25, 2025 AT 15:40 PMTHIS. I’m on venlafaxine and took a NyQuil last winter for a cold… woke up with a pounding headache and vision like a kaleidoscope. ER said I was lucky. Now I keep a list on my phone and show it to every doc. 🙏💊 #DontBeLikeMe
Rachel Cericola
December 25, 2025 AT 16:49 PMLet’s be real - the system is broken. Doctors get 12 minutes per patient. They’re not going to ask about your herbal tea, your CBD gummies, or your grandma’s ‘natural blood pressure remedy’ that’s just powdered licorice root. You are your own best advocate. Write down everything. Even the ‘harmless’ stuff. Even the ‘I’ve been taking this for years’ stuff. Even the ‘it’s just a supplement’ stuff. Your life isn’t a guess. It’s a data set. And you’re the only one holding the keys.
Blow Job
December 26, 2025 AT 20:01 PMMan, I used to think my BP was just high because I’m stressed. Turns out it was the Adderall + Zoloft combo my psych doctor didn’t flag. I didn’t even know they could interact. Now I use an app that scans every pill I take. It’s like having a nerdy bodyguard. And yeah, I still take my meds - but now I know which ones to triple-check. Don’t be like me. Check. Your. Interactions.
Christine Détraz
December 27, 2025 AT 19:30 PMMy mom had a crisis from a cold med and her blood pressure pill. She didn’t even realize it was dangerous. I made her a little card with all her meds and the red flags. She keeps it in her wallet. It’s dumb, but it works. Sometimes the simplest things save you.
EMMANUEL EMEKAOGBOR
December 28, 2025 AT 21:39 PMIt is truly remarkable how modern pharmacology has advanced, yet the human element - communication, diligence, and patient empowerment - remains the most critical variable in preventing adverse events. One must not underestimate the potency of self-advocacy in the clinical context, as the data presented herein clearly illustrates. I commend the author for this lucid exposition.
CHETAN MANDLECHA
December 30, 2025 AT 13:58 PMMAOIs and cheese? That’s old news. But did you know some Indian herbal tonics like ashwagandha can also raise BP when mixed with stimulants? No one talks about this. My cousin had a stroke after mixing it with his energy drink. He thought it was ‘natural’ so it was safe. Never again.
Jillian Angus
December 31, 2025 AT 16:59 PMjust got off a 12 hour shift and took a sudafed because my nose was stuffed... now i'm paranoid i'm gonna die. thanks for the reminder i guess
Paula Villete
January 1, 2026 AT 13:12 PMWow. So the real villain isn’t the drug - it’s the fact that we’ve outsourced our brains to pharmacists and Google. You know what’s worse than a drug interaction? A doctor who says ‘it’s fine’ because they didn’t read your 17-item list. Also, ‘MAOI Diet Helper’? That’s not an app, that’s a cry for help. But hey, at least we’ve got emojis to make it cute.
Georgia Brach
January 3, 2026 AT 11:14 AMThis article is alarmist nonsense. Hypertensive crises are rare. Most people who take these meds don’t die. You’re scaring people into avoiding life-saving medications because of statistically insignificant interactions. The real crisis is fearmongering disguised as medical advice.
Lu Jelonek
January 5, 2026 AT 03:02 AMI work in a pharmacy and see this all the time. Someone comes in for antibiotics and grabs a cold med with pseudoephedrine - no questions asked. We’re trained to ask, but most people just want to leave. I’ve stopped handing out the meds without a 2-minute chat. It’s not my job? Maybe not. But it’s my conscience.
Ademola Madehin
January 6, 2026 AT 15:19 PMmy cousin died from this. he took a ‘natural energy boost’ from a guy at the gym. turned out it had sibutramine. he was 29. no warning. no symptoms. just… gone. i don’t even trust supplements anymore. if it’s not in a bottle with a barcode, i don’t touch it.
Diana Alime
January 7, 2026 AT 12:45 PMso like… if i eat blue cheese and take my antidepressant am i gonna have a stroke?? i’m not even joking. i just want to know if i need to stop my cheese habit or if this is just fear porn
Raja P
January 8, 2026 AT 00:15 AMMy dad’s on cyclosporine after his kidney transplant. We found out his high BP wasn’t rejection - it was his OTC allergy pill. He cried. We all did. He’s fine now, but I made him a little chart with his meds and the red flags. We hang it on the fridge. It’s not fancy. But it’s alive.