Gallstone Pancreatitis: What You Need to Know
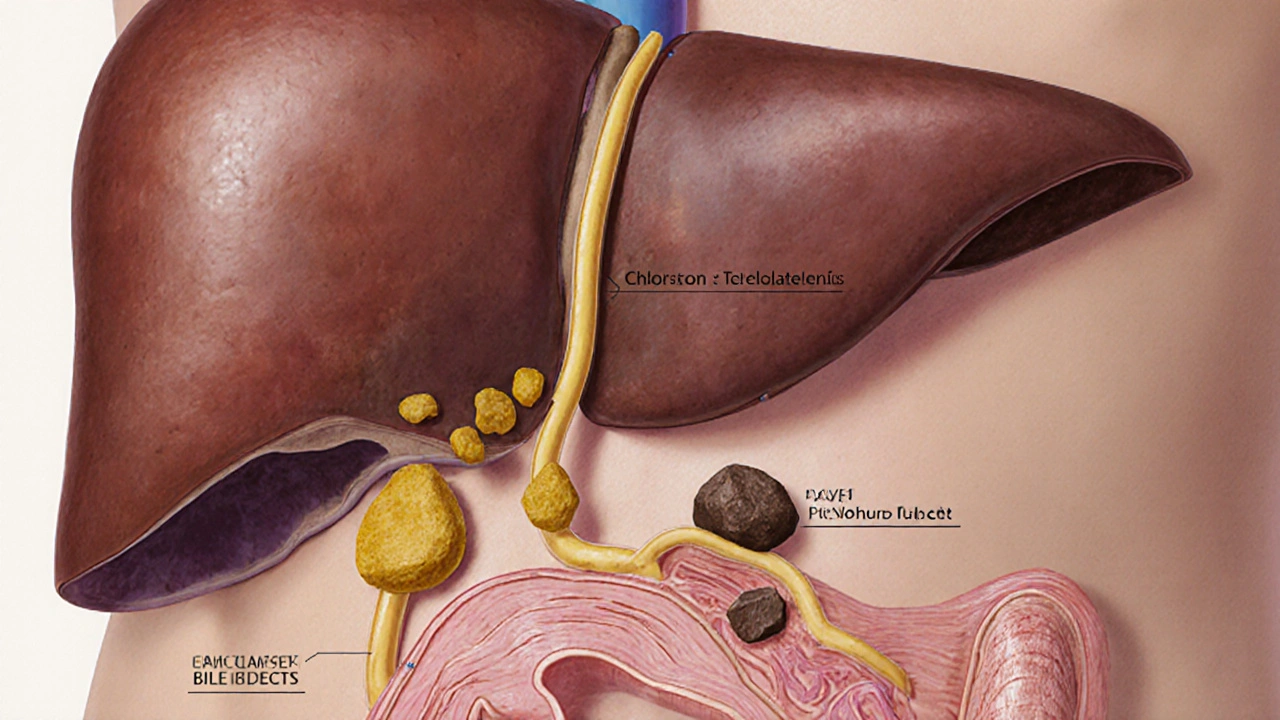
When dealing with Gallstone Pancreatitis, an acute inflammation of the pancreas triggered by a gallstone blocking the pancreatic duct. Also known as biliary pancreatitis, it combines two common problems – Gallstones, solid deposits that form in the gallbladder and can travel into the bile ducts and Pancreatitis, inflammation of the pancreas caused by enzyme activation inside the organ. The blockage creates a pressure surge that forces digestive enzymes to damage pancreatic tissue, leading to sudden, severe abdominal pain and a cascade of systemic effects. Understanding how these pieces fit together helps you spot the warning signs early and seek the right care.
Why It Happens: The Biliary Obstruction Cycle
The core trigger is a gallstone that slips from the gallbladder into the common bile duct. When the stone lodges at the ampulla of Vater, it blocks the exit pathway for bile and pancreatic juices. This Biliary obstruction, the interruption of normal flow of bile and pancreatic secretions raises ductal pressure, causing enzymes like amylase and lipase to become active inside the pancreas instead of the intestine. The resulting self‑digestive attack inflames the organ and can spread to nearby tissues. The severity often depends on stone size, the duration of blockage, and the patient's overall health. Recognizing that a simple stone can set off a chain reaction underscores why swift medical attention matters.
Doctors confirm the diagnosis by checking blood for elevated amylase and lipase levels, which typically rise three‑fold or more. Imaging plays a big role – an abdominal ultrasound can spot gallstones and duct dilation, while a contrast‑enhanced CT scan maps the extent of pancreatic inflammation. When imaging shows a stone lodged in the duct, the next step may involve ERCP, endoscopic retrograde cholangiopancreatography, a procedure that uses an endoscope and contrast dye to visualize and clear the biliary tree. ERCP not only confirms the blockage but also offers a therapeutic avenue to retrieve the stone and relieve pressure.
Treatment starts with aggressive fluid resuscitation to prevent dehydration and support organ perfusion. Pain control is essential; opioids are used cautiously under supervision. If infection is suspected, broad‑spectrum antibiotics may be added. Once the acute episode stabilizes, the definitive solution is usually a Cholecystectomy, surgical removal of the gallbladder to stop future stones from forming. This can be performed laparoscopically within a week of recovery, dramatically cutting the risk of recurrence. In some cases, early ERCP with sphincterotomy is performed before surgery to clear the duct and reduce the chance of another attack.
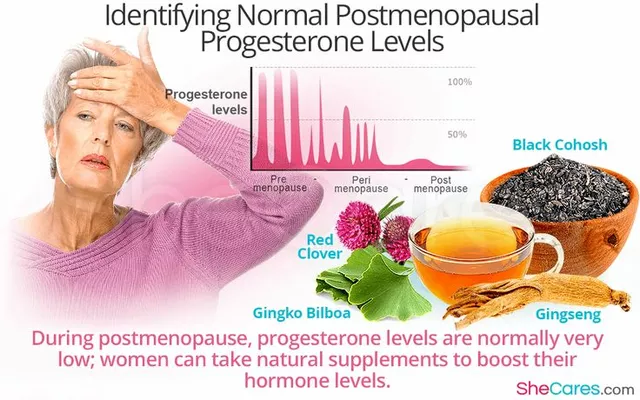
Preventing gallstone pancreatitis centers on lowering the likelihood of stone formation. Lifestyle tweaks like maintaining a healthy weight, eating a diet low in refined carbs and high in fiber, and limiting alcohol intake can make a big difference. For patients with known gallstones but no symptoms, doctors often recommend elective cholecystectomy to avoid an unexpected pancreatitis episode. Regular monitoring of liver function tests and abdominal ultrasounds helps catch stones before they cause trouble.
Complications can be serious if the inflammation spreads. Necrotizing pancreatitis may develop, where portions of the pancreas die and become infected, requiring intensive care and possibly surgical debridement. Pseudocysts—fluid‑filled sacs that form weeks after the attack—can compress nearby organs or rupture, leading to bleeding. Early recognition of these complications, guided by repeat imaging and clinical assessment, improves outcomes. Knowing the warning signs—persistent fever, worsening pain, or sudden drop in blood pressure—helps patients and caregivers act fast.
Below you’ll find a curated set of articles that dive deeper into each of these aspects. From spotting the first hint of a gallstone blockage to navigating post‑procedure recovery, the posts cover practical tips, detailed explanations, and up‑to‑date treatment guidelines. Keep reading to arm yourself with the knowledge you need to manage gallstone pancreatitis confidently and reduce the risk of future episodes.
Gallstones and Pancreatitis: How They’re Linked & What to Do
Learn how gallstones can trigger pancreatitis, spot the symptoms, understand diagnosis and treatment options, and discover prevention tips to avoid future episodes.