Generic Drug Labeling: What You Need to Know About Ingredients, Safety, and Errors
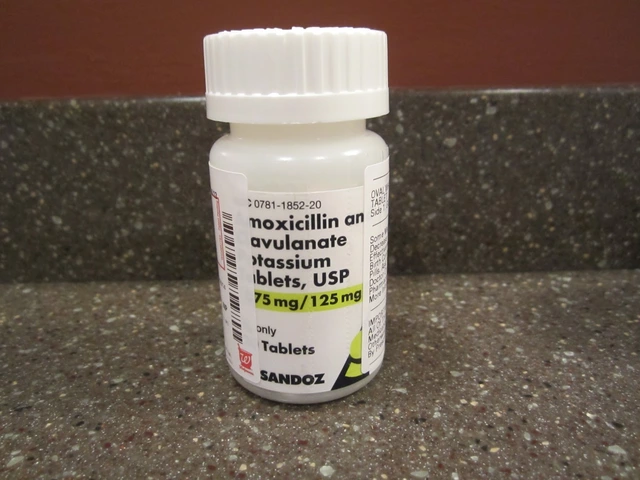
When you pick up a generic drug labeling, the printed information on a generic medication that includes active and inactive ingredients, dosage, storage instructions, and warnings. Also known as medication label, it’s the only thing standing between you and a dangerous mistake. Most people assume generics are just cheaper versions of brand-name drugs—but the label holds the real story. It’s not just about the drug name. It’s about what’s inside, how it’s stored, and whether the tiny print could be hiding an allergen, a dosing trap, or a recall risk.
Behind every inactive ingredient, non-active components like lactose, gluten, or food dyes used to bind or color pills is a hidden danger. Over 1 in 5 people react to these fillers, but they’re rarely spelled out clearly. A pill labeled "lactose-free" might still contain corn starch that triggers a reaction. And if you’re managing kidney disease, a chronic condition requiring careful medication control to prevent toxin buildup, even small changes in how a drug is absorbed can throw off your whole treatment. That’s why the bioequivalence, the FDA requirement that generic drugs absorb into the body at the same rate and extent as the brand version, within 80-125% rule matters. It’s not a suggestion—it’s the law. But even when generics meet that standard, differences in how they’re made can still cause problems. One brand might use a coating that delays absorption, while another dissolves too fast. Your body doesn’t care about the brand name—it only reacts to what’s in your bloodstream.
And then there’s the human side. A pharmacist misreads a label. A parent stores antibiotics in the fridge when they shouldn’t. A senior takes two pills because the font is too small. These aren’t rare mistakes—they’re everyday risks. That’s why pharmacy safety, the systems and practices designed to prevent medication errors in pharmacies and clinics relies on two patient identifiers, barcode scans, and clear instructions. But you can’t just rely on the system. You need to know how to read the label yourself. Is that pill supposed to be taken with food? Does it need refrigeration after opening? Is the expiration date real, or just a suggestion? The answers are on that tiny strip of paper. And if you miss them, you’re not just wasting money—you’re risking your health.
What you’ll find below isn’t just a list of articles. It’s a toolkit. From how to spot look-alike drug names that cause deadly mix-ups, to why some generics fail in storage, to what to do when your insurance blocks a cheaper option—every post cuts through the noise. No fluff. No theory. Just what you need to know to read the label, ask the right questions, and stay safe.
Generic Drug Labeling Requirements: What the FDA Mandates
The FDA requires generic drug labels to match brand-name labels exactly, with few exceptions. This ensures patient safety but creates delays in updating critical safety information. Learn what's mandated, how manufacturers comply, and why the system is under review.