Heartburn Medications: What Works, What to Avoid, and How to Use Them Safely
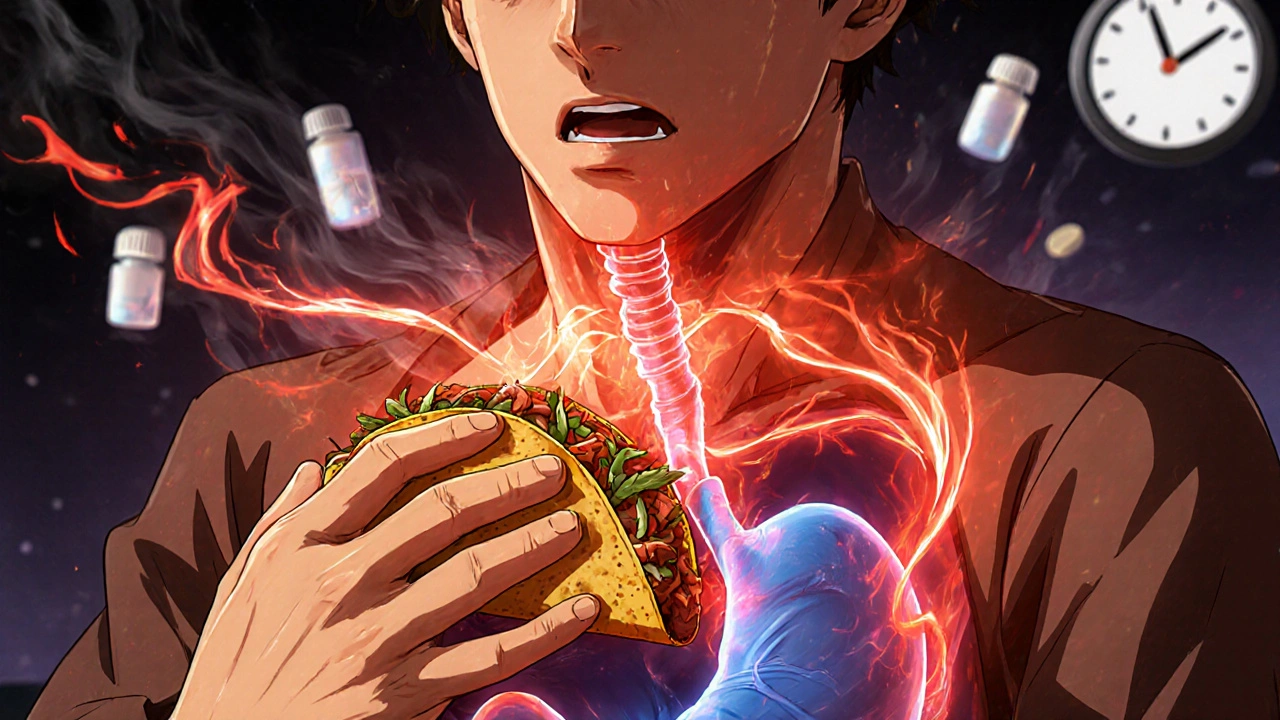
When you feel that burning feeling rising from your stomach into your chest, you’re not just dealing with discomfort—you’re dealing with heartburn medications, drugs designed to reduce stomach acid and relieve the burning sensation caused by acid reflux. Also known as acid reflux treatments, these medications are among the most commonly used over-the-counter and prescription drugs in the U.S., with millions reaching for them every day. But not all heartburn meds are the same, and using the wrong one—or the right one too long—can do more harm than good.
There are three main types you’ll find on shelves or in prescriptions: antacids, fast-acting drugs that neutralize stomach acid right away, often used for quick relief after meals; H2 blockers, medications like famotidine that reduce acid production over several hours; and proton pump inhibitors, stronger drugs like omeprazole that shut down acid production at the source, often used for chronic or severe cases. Each has its place. Antacids give fast relief but don’t last. H2 blockers are good for mild, occasional heartburn. PPIs are powerful but come with risks if used long-term without a doctor’s guidance.
Many people think if a little helps, more must be better. But taking PPIs daily for years without knowing why your heartburn started can mask serious problems like GERD, ulcers, or even Barrett’s esophagus. Some studies show long-term use may increase the risk of bone fractures, kidney issues, or nutrient deficiencies like magnesium and B12. Meanwhile, antacids with aluminum or magnesium can cause diarrhea or constipation if overused. And H2 blockers? They work well for most, but can interact with other meds like blood thinners or antifungals.
What’s missing from the shelves? Understanding. Most people don’t know that heartburn isn’t always about too much acid—it can be about weak muscles at the bottom of the esophagus, certain foods, stress, or even lying down too soon after eating. That’s why some of the best advice isn’t in a pill bottle: eat smaller meals, avoid spicy or fatty foods, don’t lie down for three hours after eating, and raise the head of your bed a few inches. These simple habits can cut heartburn in half—for many, they’re the real fix.
The posts below cover exactly what you need to know: how different heartburn meds compare, what side effects you might not expect, how they interact with other drugs you’re taking, and when it’s time to see a doctor instead of reaching for another tablet. You’ll find real-world advice on choosing between OTC and prescription options, how to reduce your reliance on pills, and what to watch for if your symptoms change. No fluff. No marketing. Just clear, practical info to help you take control—without risking your health.
Spicy Foods and GI-Irritating Medications: How to Reduce Heartburn Risk
Learn how spicy foods and common medications like aspirin and pantoprazole trigger heartburn-and what actually works to reduce symptoms without giving up flavor or your prescriptions.