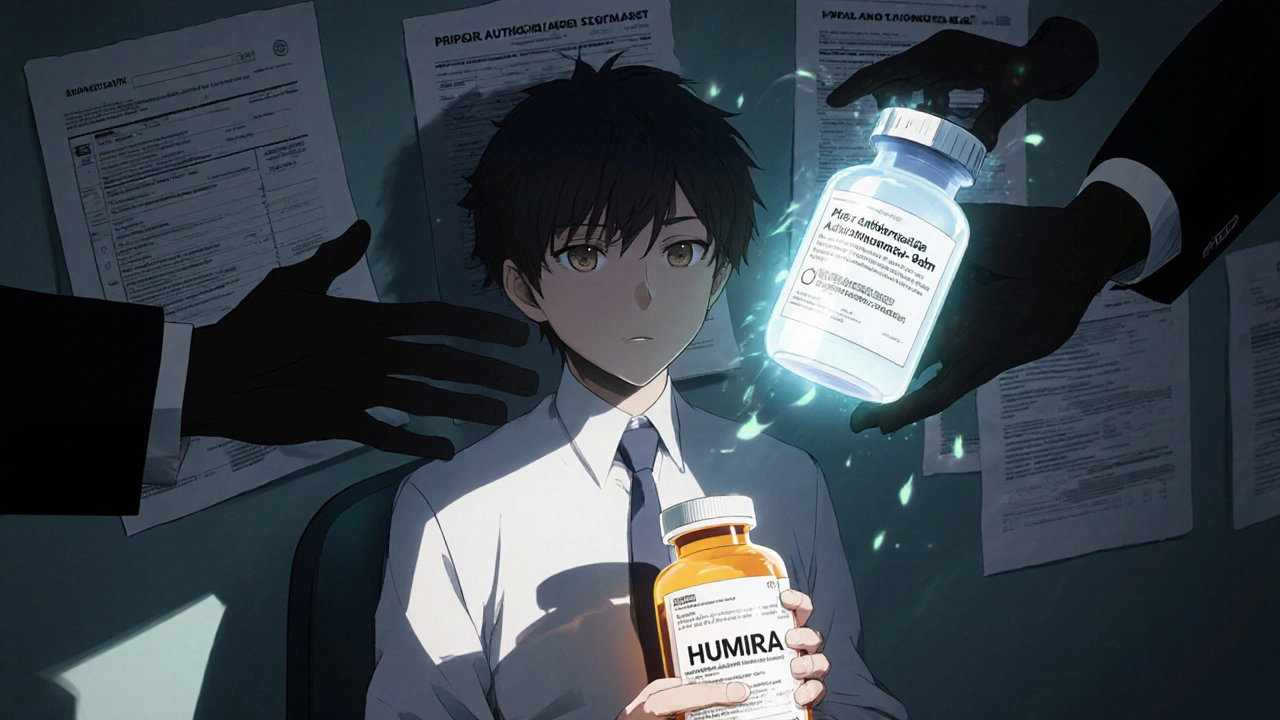
Humira Biosimilar Coverage: What You Need to Know About Cost, Access, and Alternatives
When you’re managing a chronic condition like rheumatoid arthritis or Crohn’s disease, Humira biosimilar coverage, affordable versions of the biologic drug adalimumab approved by the FDA. Also known as adalimumab biosimilars, these drugs work just like the original but cost significantly less—often 15% to 35% cheaper. Many insurers now require patients to try a biosimilar first before approving the brand-name Humira, making coverage a make-or-break factor for treatment. If you’ve been on Humira for years, switching isn’t just about price—it’s about understanding how your body reacts, what your plan allows, and whether your doctor supports the change.
Biosimilar drugs, medications designed to be highly similar to an already-approved biologic with no clinically meaningful differences in safety or effectiveness. Also known as follow-on biologics, they’re not generics—they’re more complex to make because they come from living cells, not chemicals. That’s why they’re still pricier than pills, but way cheaper than Humira. In the U.S., biosimilars like Humira alternatives, FDA-approved versions of adalimumab including Amjevita, Cyltezo, and Hyrimoz. Also known as adalimumab biosimilars are now widely available. But coverage doesn’t mean automatic approval. Some plans still restrict which biosimilar you can get, or require prior authorization. Others only cover one brand, forcing you to switch even if you’re stable on Humira. If your insurer denies coverage, you’re not stuck. Many manufacturers offer patient assistance programs, coupons, or co-pay cards to bring costs down—even if you’re on Medicare or private insurance.
It’s not just about money. People worry about side effects, effectiveness, and whether switching will trigger a flare-up. Studies show most patients do just as well on biosimilars as they did on Humira, but your doctor needs to monitor you closely in the first few months. If you’ve had bad reactions to other biologics, or if your condition is severe, your provider might push back on a switch. That’s okay—coverage rules don’t override medical judgment. You have the right to appeal, request an exception, or ask for a step therapy exemption based on your history.
What you’ll find below are real, practical guides on how to navigate insurance hurdles, what questions to ask your pharmacist, how to spot coverage changes in your plan documents, and why some biosimilars work better for certain conditions than others. You’ll also see how drug shortages, manufacturer pricing shifts, and new FDA approvals are changing the landscape. No fluff. Just what you need to get the right treatment at a price you can afford.
Insurance Coverage of Biosimilars: How Prior Authorization and Tier Placement Block Savings
Biosimilars can cut biologic drug costs by up to 33%, but insurance rules like prior authorization and same-tier placement block access. Here's how coverage works - and what you can do about it.