Kidney Disease Meds: What Works, What to Watch For, and How to Stay Safe
When your kidneys aren’t working right, kidney disease meds, prescription drugs used to manage symptoms and slow damage in chronic kidney disease. Also known as renal medications, they help control blood pressure, balance minerals, and reduce waste buildup in your blood. These aren’t cure-all pills—they’re tools to keep you feeling better and avoid complications like heart problems or bone damage. Many people on these meds also need to watch what they eat, track fluid intake, and get regular lab tests. It’s not just about popping pills; it’s about making them work with your whole body.
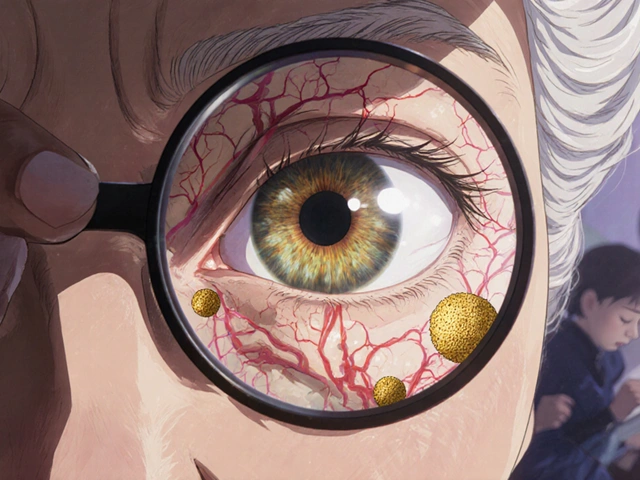
One big group of phosphorus binders, medications that attach to dietary phosphorus in the gut so it doesn’t get absorbed. Also known as phosphate binders, it includes calcium acetate and sevelamer. Too much phosphorus from food can harden your blood vessels and weaken your bones, so these pills are taken with every meal. But they don’t work if you skip meals or forget to take them with food. Another key player is blood pressure meds, drugs like ACE inhibitors or ARBs that protect kidney function by lowering pressure in the filtering units. Also known as renal-protective antihypertensives, they are often the first line of defense—not just for high blood pressure, but to slow kidney damage itself. Then there are diuretics to manage fluid, erythropoietin to fight anemia, and vitamin D analogs to keep bones strong. Each has its own risks: too much fluid loss, too low iron, or calcium buildup in your eyes or arteries.
What you won’t find in most doctor’s notes is how messy this gets in real life. You might be taking six different pills just for your kidneys, each with different timing, food rules, and side effects. One person’s miracle drug is another’s nightmare—like prednisone causing mood swings or calcium acetate affecting vision. And if you’re on dialysis, the list gets longer: iron infusions, anticoagulants, even antibiotics to fight infections from the access site. The goal isn’t to take more pills—it’s to take the right ones, at the right time, without mixing them up or missing doses. That’s why labeling, storage, and double-checking with your pharmacist matters just as much as the prescription itself.
Below, you’ll find real guides from people who’ve been there. You’ll learn how to spot dangerous interactions, what to do when a medication runs out, how to tell if a generic version is truly safe, and how to avoid hidden allergens in pills. Some posts break down how phosphorus binders really work. Others show how to manage side effects like nausea or fatigue. You’ll see what works for seniors, what to watch for after a transplant, and why some meds need refrigeration while others don’t. This isn’t theory—it’s what people actually need to know to stay healthy while managing kidney disease.
Kidney Disease Medications: Phosphate Binders, Diuretics, and Anticoagulants Explained
Phosphate binders, diuretics, and anticoagulants are essential for managing chronic kidney disease. Learn how they work, which ones are safest, and how to avoid dangerous side effects and dosing errors.