Medicare Part D Biosimilars: What You Need to Know About Cost-Saving Alternatives
When you’re on Medicare Part D biosimilars, affordable versions of complex biologic drugs approved by the FDA to work like their brand-name counterparts. Also known as generic biologics, they help lower costs without sacrificing safety or effectiveness for conditions like rheumatoid arthritis, diabetes, and cancer. Unlike regular generics that copy simple chemical pills, biosimilars are made from living cells—so they’re more complex, but still tightly regulated to match the original biologic drug’s performance.
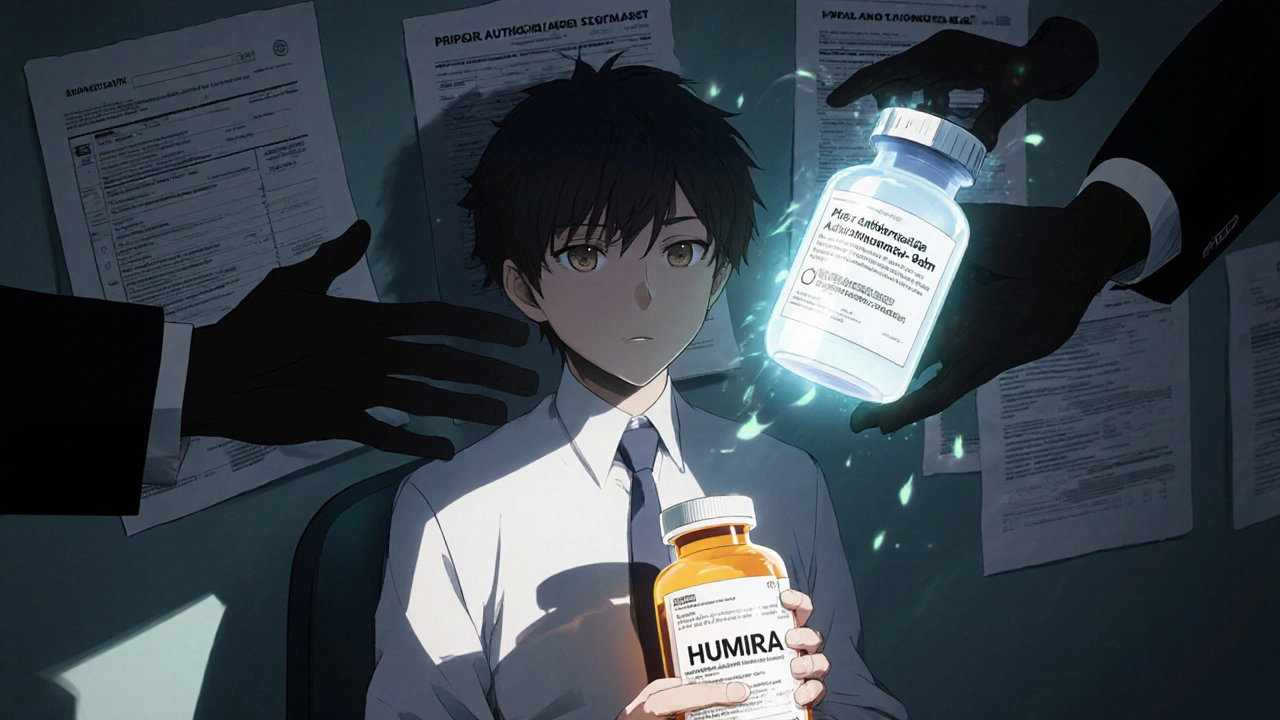
Biologic drugs, large-molecule medications made from living organisms, often cost thousands per month. These include drugs like Humira, Enbrel, and Lantus. Medicare Part D, the prescription drug benefit for Medicare beneficiaries covers many of these, but the high prices put pressure on both patients and the system. That’s where biosimilars come in—they’re not exact copies, but they’re close enough that the FDA says they work the same way. And because they’re cheaper, Medicare plans often push them first before approving the brand-name version.
You might wonder if biosimilars are safe. They’re not experimental. The FDA requires them to go through rigorous testing to prove they have no meaningful difference in how they work, how safe they are, or how strong their effects are. Many patients switch from Humira to a biosimilar and see the same results with lower out-of-pocket costs. Some Medicare plans even require you to try a biosimilar first before covering the brand-name drug.
But it’s not always simple. Not all biosimilars are covered the same way. Some plans have step therapy rules. Others might only cover one biosimilar version of a drug. And while biosimilars are cheaper, they’re still biologics—so they’re not as cheap as your typical generic pill. Still, for people on long-term treatments, even a 20% to 30% savings can mean hundreds of dollars a month.
What you’ll find in the posts below isn’t just theory. It’s real-world stuff: how drug shortages hit biosimilar supply chains, why absorption rates matter even for complex drugs, how patient identification systems prevent mix-ups with similar-looking names, and what happens when a medication error occurs with a biologic. You’ll also see how health literacy helps people read their prescriptions correctly, how combination pills reduce pill burden, and why whistleblower protections matter when manufacturing quality slips.
If you’re on Medicare Part D and taking a biologic, you’re not just a patient—you’re a decision-maker. Knowing how biosimilars fit into your plan, what to ask your pharmacist, and how to spot potential errors can save you money and keep you safe. The posts ahead give you the tools to do exactly that—no jargon, no fluff, just what you need to understand your meds and your coverage.
Insurance Coverage of Biosimilars: How Prior Authorization and Tier Placement Block Savings
Biosimilars can cut biologic drug costs by up to 33%, but insurance rules like prior authorization and same-tier placement block access. Here's how coverage works - and what you can do about it.