Medication Allergies: Signs, Triggers, and How to Stay Safe
When your body mistakes a medication allergy, an immune system overreaction to a drug that can range from mild rash to life-threatening shock. Also known as drug hypersensitivity, it's not just a side effect—it’s your body fighting something it thinks is an invader. Unlike nausea or dizziness, which are common side effects, a true medication allergy involves your immune system releasing histamines and other chemicals, often within minutes or hours of taking the pill. This isn’t rare—about 5% to 10% of people report a drug allergy, and many of them are wrong. But some are dangerously right.
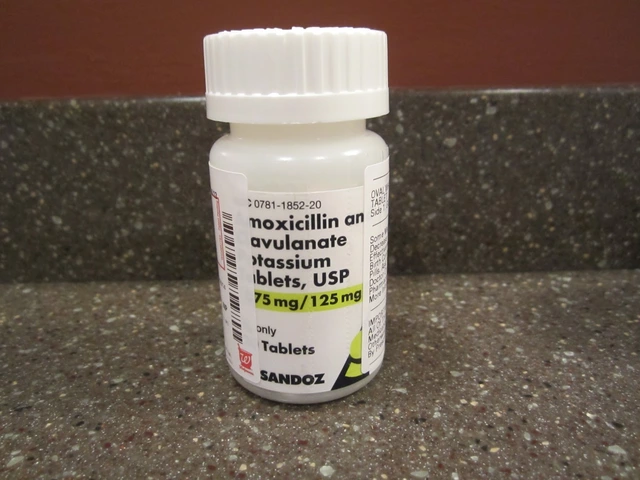
Some drugs are far more likely to cause trouble. penicillin, a common antibiotic that triggers the most frequent and severe allergic reactions tops the list. If you’re allergic to penicillin, you might also react to related drugs like amoxicillin or cephalosporins—that’s called cross-reactivity, when one drug’s structure fools your immune system into reacting to another. NSAIDs, like ibuprofen and aspirin, are another big culprit, especially for people with asthma or nasal polyps. Even antihistamines, which are supposed to stop allergies, can sometimes cause them. And yes, it’s possible to develop an allergy to a drug you’ve taken safely for years.
Symptoms vary. A rash or hives is common. Swelling of the lips or throat? That’s urgent. Trouble breathing, dizziness, or a sudden drop in blood pressure could mean anaphylaxis—this kills people every year. Many don’t realize they’re having an allergic reaction until it’s too late. That’s why knowing your triggers matters. Keep a written list: what drug, when you took it, what happened. Show it to every doctor, pharmacist, and ER nurse. Don’t just say "I’m allergic to antibiotics." Say "I broke out in hives after amoxicillin in 2021." Specifics save lives.
Some reactions aren’t allergies at all—like the flushing from niacin or the stomach upset from metformin. But confusing them can lead to unnecessary restrictions or worse, dangerous substitutions. If you’ve had a reaction, get tested. Skin tests and blood tests can confirm true allergies for many drugs. And if you’re told you’re allergic to penicillin, ask if you’ve been tested. Up to 90% of people who think they are allergic aren’t—and they miss out on safer, cheaper, more effective treatments.
Below, you’ll find real, practical guides on how to avoid dangerous mix-ups, recognize hidden allergens in common meds, understand why some drugs trigger reactions while others don’t, and what to do when you’re handed a prescription that could be risky. These aren’t theory pieces—they’re tools made for people who’ve been burned before, or who want to stay one step ahead.
How to Address Allergies to Inactive Ingredients in Generics
Many generic medications contain allergens like lactose, gluten, or food dyes that aren't listed clearly. Learn how to identify risky inactive ingredients and protect yourself from hidden reactions when switching brands.