Pantoprazole Effectiveness: How Well It Works and What You Need to Know
When you’re dealing with constant heartburn or acid reflux, pantoprazole, a proton pump inhibitor used to reduce stomach acid production. Also known as a PPI, it’s one of the most prescribed medications for conditions like GERD and peptic ulcers. But does it actually work? And how does it stack up against other options? The answer isn’t just yes or no—it’s about timing, dosage, and your body’s response.
Pantoprazole works by blocking the proton pumps in your stomach lining—the tiny engines that produce acid. Unlike antacids that just coat the irritation, pantoprazole stops the acid at the source. Studies show it reduces acid by up to 90% within 24 hours for most people. That’s why doctors often recommend it for long-term GERD management, not just quick relief. But effectiveness isn’t the same for everyone. Some feel better in days. Others need weeks. And a small group finds it doesn’t help at all—often because their symptoms aren’t from excess acid, but from functional issues like IBS or bile reflux.
It’s also important to know how pantoprazole compares to other proton pump inhibitors, medications like omeprazole, esomeprazole, and lansoprazole that target the same acid-producing system. In head-to-head trials, pantoprazole performs just as well as omeprazole for healing esophagitis and reducing symptoms. The big difference? Pantoprazole has fewer interactions with other drugs, which matters if you’re on multiple medications. It’s also less affected by food, so you can take it before or after meals without losing power.
But here’s the catch: pantoprazole isn’t magic. It won’t fix poor diet, stress, or lying down after eating. If you’re still having symptoms after 4–8 weeks, it’s not the drug—it’s the lifestyle. That’s why many of the posts below focus on related topics like medication adherence, combination treatments, and how to reduce pill burden. People don’t just need the right drug—they need the right plan.
Some users report side effects like headaches, diarrhea, or long-term nutrient loss, especially with years of use. That’s why doctors now recommend the lowest effective dose for the shortest time possible. If you’ve been on pantoprazole for more than a year, you’re not alone—but you should talk to your provider about whether it’s still necessary.
The posts below dive into real-world issues around medications like pantoprazole: how generics match brand drugs in absorption, how drug interactions can sneak up on you, and how to avoid common mistakes that make treatment fail. You’ll find practical advice from people who’ve been there—what worked, what didn’t, and when to ask for help. Whether you’re new to PPIs or wondering if it’s time to switch, this collection gives you the facts without the fluff.
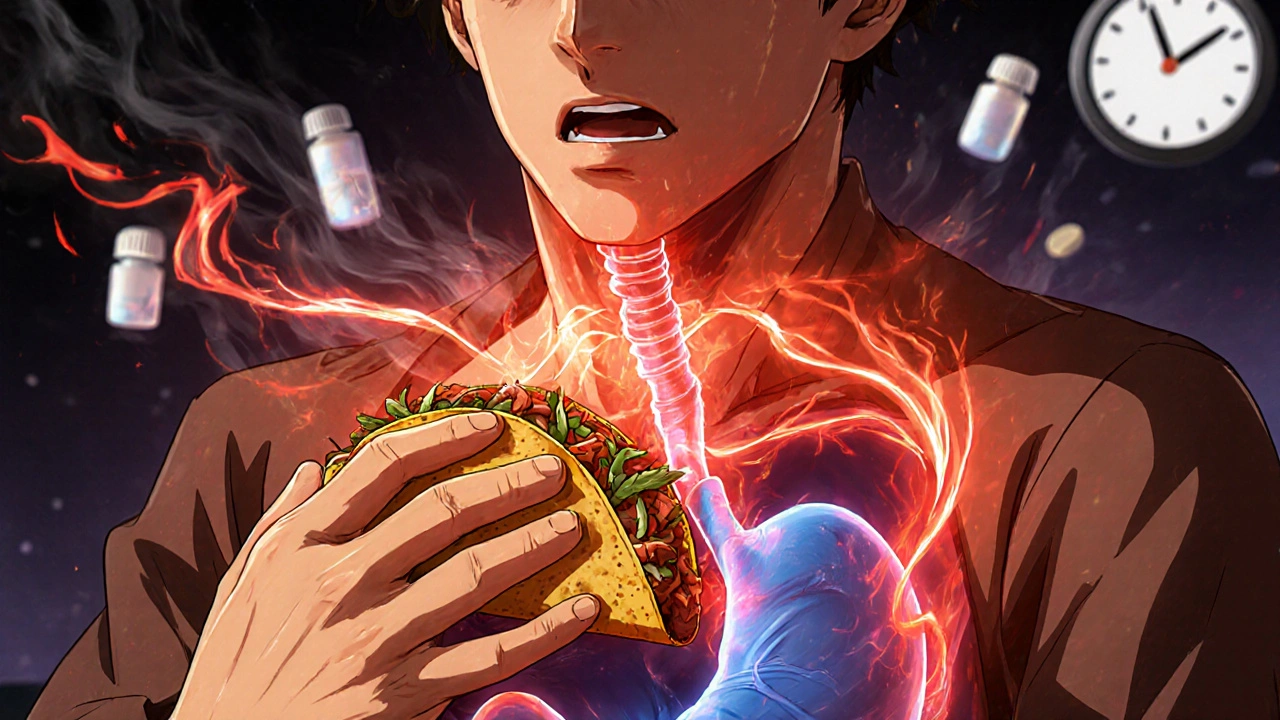
Spicy Foods and GI-Irritating Medications: How to Reduce Heartburn Risk
Learn how spicy foods and common medications like aspirin and pantoprazole trigger heartburn-and what actually works to reduce symptoms without giving up flavor or your prescriptions.