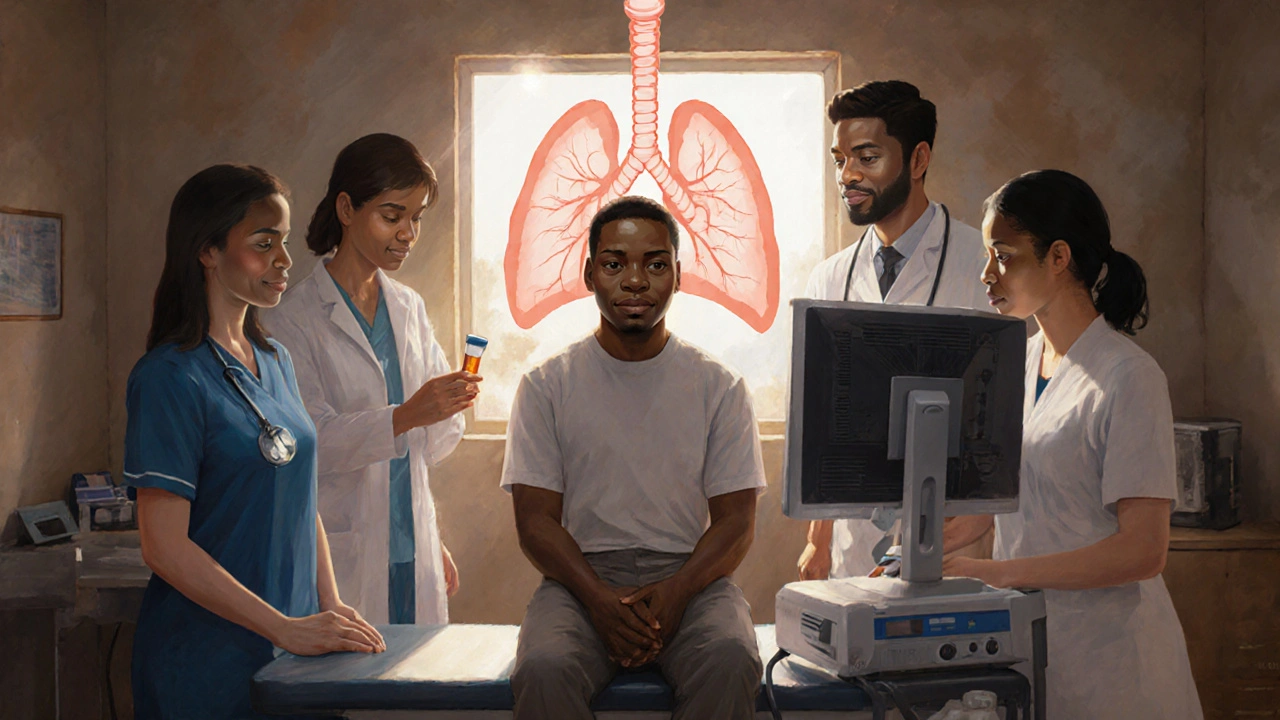
TB Treatment HIV: What You Need to Know
When dealing with TB treatment HIV, the medical approach that combines tuberculosis therapy with HIV care to improve outcomes for people living with both infections. Also known as TB/HIV co‑infection therapy, it requires close coordination between antibiotics and antiretroviral drugs, careful monitoring for side effects, and often a public‑health support system. The goal is simple: kill the TB bacteria while keeping the HIV virus suppressed, so patients can stay healthy and avoid complications like drug‑resistant TB or immune reconstitution inflammatory syndrome (IRIS).
Key Players in the Management Puzzle
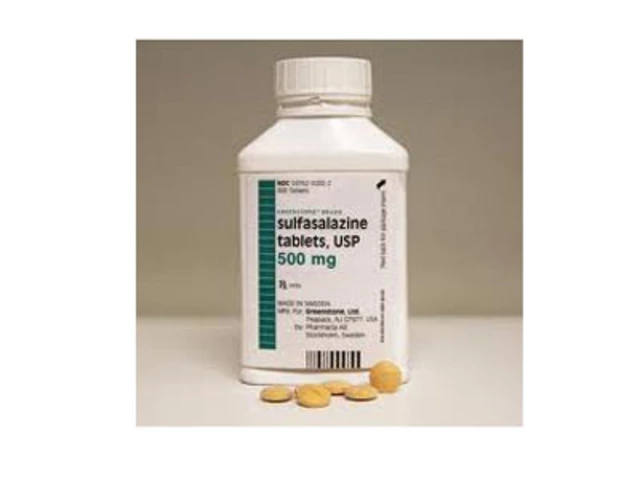
Understanding Tuberculosis, a bacterial lung disease caused by Mycobacterium tuberculosis is the first step. TB spreads through the air, and people with weakened immune systems—especially those with Human Immunodeficiency Virus, the virus that attacks CD4 cells and leads to AIDS if untreated—are far more likely to develop active disease after exposure. Because HIV lowers immunity, the standard TB drug regimen (usually isoniazid, rifampicin, pyrazinamide, and ethambutol) must be timed with Antiretroviral therapy, a combination of medicines that block HIV replication and restore immune function. Starting ART too early can trigger IRIS, while delaying it raises the risk of TB progression, so clinicians follow evidence‑based timing guidelines.
Another essential component is Directly Observed Therapy, a strategy where a health worker watches patients take their TB meds to ensure adherence. DOT works well for co‑infected patients because missed doses can lead to drug‑resistant TB, which is harder and more expensive to treat. In many Canadian programs, DOT is combined with community‑based HIV support services, creating a seamless care pathway. When drug‑resistant TB does appear, clinicians may need to add second‑line agents like fluoroquinolones or injectables, and they must adjust ART to avoid harmful drug interactions, especially with rifampicin, which can lower the levels of many antiretrovirals.
All these pieces—TB diagnostics, ART selection, DOT implementation, and monitoring for side effects—form a network of interdependent decisions. The central idea is that effective TB treatment HIV hinges on integration: you cannot treat one disease in isolation without compromising the other. This perspective shapes the articles you’ll find below. We’ve gathered practical guides on selecting the right drug combos, handling common adverse reactions, navigating pregnancy with co‑infection, and using newer therapies like shorter TB regimens and integrase‑strand transfer inhibitors for HIV. Whether you’re a patient, a caregiver, or a health professional, the collection offers clear, actionable information to help you manage TB/HIV co‑infection confidently.
How Tuberculosis and HIV/AIDS Interact: Risks, Diagnosis, and Treatment
Explore the complex relationship between tuberculosis and HIV/AIDS, covering transmission, clinical impact, diagnosis, treatment, and global health strategies.